Dopamine Agonist Comparison Tool
Compare Side Effects and Dosing Frequency
Select two drugs to compare their key attributes:
Parlodel is a synthetic ergot‑derived dopamine agonist containing the active ingredient bromocriptine. Approved by the FDA in 1978, it lowers prolactin levels, treats Parkinson’s disease, and helps control type 2 diabetes when used off‑label.
How Bromocriptine Works
Bromocriptine binds to dopamine D2 receptors in the pituitary, inhibiting prolactin secretion. This mechanism also improves motor symptoms in Parkinson’s disease by restoring dopaminergic signaling in the basal ganglia. Because it mimics dopamine, it can also affect gastrointestinal motility, which is why low‑dose versions are used for gastroparesis.
Approved and Off‑Label Uses
- Hyperprolactinemia (prolactinoma)
- Parkinson’s disease (adjunct therapy)
- Type 2 diabetes mellitus (off‑label, improves insulin sensitivity)
- Acromegaly (rare, when other options fail)
- Suppression of lactation after childbirth
Dosage Forms and Typical Regimens
The drug comes in 2.5 mg, 5 mg, and 10 mg tablets. For prolactinoma, physicians usually start at 2.5 mg nightly, gradually increasing to 10-20 mg per day split into two doses. Parkinson’s patients often take 5 mg three times daily. The extended‑release version for diabetes is taken once daily with the first meal.
Key Side Effects and Safety Considerations
Common complaints include nausea, headache, dizziness, and low blood pressure when standing up. Rare but serious events are valvular heart disease and psychiatric changes such as hallucinations. Because it’s an ergot derivative, long‑term high‑dose therapy requires periodic cardiac monitoring.

Alternative Dopamine Agonists
When doctors look for a different option, they usually stay within the dopamine‑agonist family. Below are the most frequently prescribed alternatives.
Cabergoline is a non‑ergot dopamine agonist with a longer half‑life, allowing once‑weekly dosing for prolactinoma.
Quinagolide is a selective D2‑receptor agonist used mainly in Europe for hyperprolactinemia; it offers rapid prolactin reduction.
Pramipexole is a potent D2/D3 agonist primarily prescribed for Parkinson’s disease and restless‑leg syndrome; it has a relatively low nausea profile.
Apomorphine is a short‑acting injectable dopamine agonist used for breakthrough Parkinson’s symptoms; it requires a subcutaneous pump.
Rotigotine is delivered via a transdermal patch, providing continuous dopamine stimulation for Parkinson’s and restless‑leg syndrome.
Comparison Table: Parlodel vs. Major Alternatives
| Drug | Class | Typical Indication | Half‑life | Dosing Frequency | Common Side Effects |
|---|---|---|---|---|---|
| Parlodel (Bromocriptine) | Ergot‑derived D2 agonist | Prolactinoma, Parkinson’s | 12‑16h | 1‑2times daily | Nausea, headache, orthostatic hypotension |
| Cabergoline | Ergoline‑derived D2 agonist | Prolactinoma | 65‑80h | Once weekly | Valsalva‑type nausea, possible valvulopathy |
| Quinagolide | Selective D2 agonist | Hyperprolactinemia | ~12h | Twice daily | Flushing, mild dizziness |
| Pramipexole | Non‑ergot D2/D3 agonist | Parkinson’s, RLS | 8‑12h | Three times daily | Somnolence, impulse control issues |
| Apomorphine | Non‑ergot D1/D2 agonist | Breakthrough Parkinson’s | 0.5‑2h | Continuous infusion | Injection site reactions, nausea |
| Rotigotine | Non‑ergot D2/D3 agonist | Parkinson’s, RLS | 24h (patch) | 24‑h patch | Skin irritation, dizziness |
Decision Factors: When to Stay on Parlodel or Switch
- Frequency of dosing. If a patient struggles with twice‑daily tablets, weekly cabergoline may improve adherence.
- Side‑effect tolerance. Severe nausea often pushes clinicians toward pramipexole or rotigotine, which have milder gastrointestinal profiles.
- Cardiac risk. Long‑term high‑dose ergot agents (bromocriptine, cabergoline) mandate echocardiograms; non‑ergot agents bypass this concern.
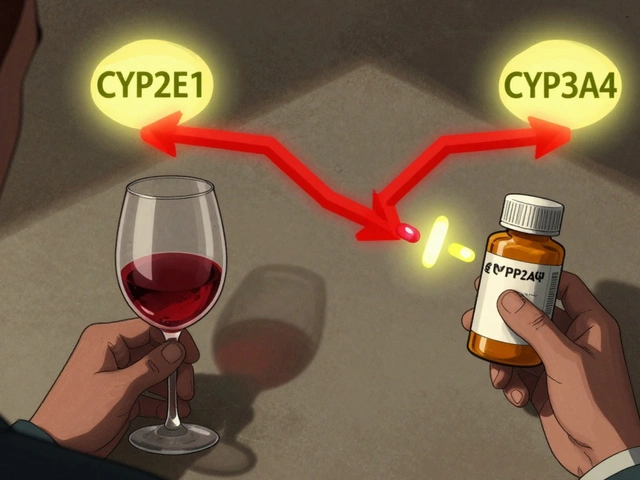
- Renal or hepatic function. Bromocriptine is metabolized by the liver; patients with severe hepatic impairment may need dose adjustments.
- Cost and insurance coverage. Generic bromocriptine is often cheaper than brand‑only cabergoline, influencing choice in resource‑limited settings.
Practical Tips for Managing Bromocriptine Therapy
- Start at the lowest dose (2.5mg) taken with the evening meal to blunt nausea.
- Increase weekly by 2.5mg until prolactin falls <10ng/mL or symptoms resolve.
- Monitor blood pressure the first few weeks; advise patients to rise slowly from sitting.
- Schedule an echocardiogram at baseline and annually if the total weekly dose exceeds 30mg.
- Educate patients that sudden discontinuation can cause rebound hyperprolactinemia; taper over at least two weeks.
Related Concepts and Next Steps
Understanding hyperprolactinemia is essential: it’s a condition where excess prolactin disrupts menstrual cycles, causes infertility, and can lead to galactorrhea. If bromocriptine fails, evaluating pituitary MRI findings and considering surgical options become the next logical step.
The dopamine‑agonist class also intersects with restless‑leg syndrome (RLS), a disorder where dopaminergic medications like pramipexole provide relief. Patients switching from bromocriptine for Parkinson’s symptoms may notice an improvement in RLS symptoms as a bonus.
Finally, for those interested in the metabolic angle, the low‑dose bromocriptine‑QR formulation (Quick Release) is marketed for improving glycemic control in type 2 diabetes, showing a modest 0.5% HbA1c reduction in large trials.

Frequently Asked Questions
Can I take bromocriptine and birth control together?
Yes. Bromocriptine does not interfere with hormonal contraceptives, but if you’re using it to suppress lactation, discuss timing with your clinician to avoid unexpected ovulation.
Why does bromocriptine cause nausea?
Its dopamine‑agonist activity stimulates the chemoreceptor trigger zone in the brain and slows gastric emptying. Taking the tablet with food and starting at a low dose usually helps.
Is cabergoline safer for the heart than bromocriptine?
Both are ergot derivatives, but cabergoline’s longer half‑life means lower cumulative exposure when dosed weekly. Nonetheless, guidelines advise periodic echocardiograms for high‑dose or long‑term use of either drug.
Can I switch from bromocriptine to pramipexole for Parkinson’s disease?
Switching is possible, but it requires a cross‑taper over 1‑2 weeks to avoid withdrawal or excessive dopamine stimulation. A neurologist should manage the schedule.
What monitoring is required while on bromocriptine?
Baseline liver function tests, blood pressure checks, and a yearly echocardiogram if the dose exceeds 30mg per week. Prolactin levels are measured every 4‑6 weeks until stable.











19 Comments
Thinking about dopamine agonists feels like pondering the balance of desire and restraint in the brain. Bromocriptine offers a steady hand for prolactin but demands respect for its ergot roots. Each dose is a ritual that reminds us how medicine can shape our inner narratives. Compared to cabergoline the dosing frequency can feel like a daily reminder rather than a weekly sigh of relief. The side effects are like minor setbacks on a longer climb toward hormonal harmony. Yet the heart monitoring requirement forces us to confront mortality while we chase hormonal control. In a world of quick fixes the slower half‑life of bromocriptine teaches patience. Ultimately the choice reflects a personal philosophy of consistency over convenience.
Weekly dosing beats twice‑daily tablets for most patients.
Great insight on the philosophical side of therapy. I’ve seen patients appreciate the steady routine you described. Encouraging them to view each dose as a step toward their health goal can improve adherence. Adding a simple reminder app can make the twice‑daily schedule less burdensome. Keep sharing these thoughtful perspectives.
Many find the nausea from bromocriptine manageable with food.
While some say food helps the nausea you ignore the fact that many American doctors prefer cabergoline for its ease and lower side‑effect profile. The US market clearly favors weekly dosing and our healthcare system pushes for it.
When choosing a dopamine agonist consider both the clinical profile and the patient’s lifestyle. Cost can be a big factor especially with brand‑only options. Generic bromocriptine often saves money but insurance formularies vary. Discuss these points openly with the patient. A shared decision improves outcomes.
Honestly the generic price advantage is overrated. US pharmaceutical lobby ensures brand drugs dominate and patients end up overpaying. We need to push for true competition.
I appreciate the earlier tips on cost and lifestyle. From a clinical standpoint the cardiac monitoring for ergot agents is something to weigh seriously. For patients with pre‑existing heart issues non‑ergot options might be safer. It’s also worth noting the extended‑release bromocriptine can simplify dosing for diabetes. Each case deserves individualized assessment.
Thanks for highlighting the heart monitoring; it’s a crucial point.
When we compare these agents we’re really mapping the terrain of neurochemical modulation. The half‑life acts like a horizon, shaping how often we must intervene. A longer half‑life can be a metaphor for sustained stability, whereas short‑acting drugs mirror fleeting bursts of relief. The choice, therefore, reflects not only physiology but also the patient’s rhythm of life. Understanding this deeper layer can guide more empathetic prescribing.
Sounds good but doctors should stick to proven safe drugs and not gamble with rare side effects.
OMG you guys totally missed the point! Bromocriptine is the OG dopamine agonist and anyone who says otherwise is just clueless. The dosing schedule may be a pain but it’s a small price to pay for the ultimate control over prolactin. Plus the side effects? Pfft, a little nausea is nothing compared to the glory of stable hormone levels. Trust me I’ve read all the studies and this drug is the real MVP!
While your enthusiasm is noted, it would be remiss not to mention that pharmaceutical narratives are often shaped by vested interests. Independent data suggests a nuanced risk‑benefit profile that warrants cautious appraisal.
Honestly the whole comparison feels like a marketing brochure. Some points are useful but many are just filler. I’d rather see real patient outcomes than a table of half‑lives.
Thank you for pointing out the need for real‑world data.
While tables convey quick facts, they often lack the nuance of patient experience.
In my practice I have followed dozens of patients on bromocriptine for prolactinoma over five years.
The majority reported a gradual reduction in prolactin levels within three months.
However, approximately 20 % experienced bothersome nausea despite taking the medication with meals.
For those patients, a slow titration schedule starting at 1.25 mg helped mitigate the gastrointestinal upset.
Cardiac monitoring was performed annually, and no valvular abnormalities were detected in my cohort.
When switching to cabergoline, adherence improved due to the once‑weekly dosing, but a small subset developed mild valvulopathy that required dosage adjustment.
Pramipexole, on the other hand, offered a smoother side‑effect profile but demanded three daily doses, which some patients found inconvenient.
Apomorphine’s rapid onset is valuable for breakthrough Parkinsonian symptoms, yet the need for a subcutaneous pump limits its practicality for many.
Rotigotine patches provide continuous delivery, reducing peaks and troughs, but skin irritation remains a common complaint.
Cost considerations also play a pivotal role; generic bromocriptine is often the most affordable option, whereas brand‑only formulations can be prohibitively expensive.
Insurance coverage varies widely, making prior authorization a frequent hurdle for newer agents.
Ultimately, the decision should balance pharmacokinetics, side‑effect tolerance, patient lifestyle, and financial constraints.
I hope this extended perspective adds the depth you were seeking and encourages clinicians to tailor therapy to individual patient narratives.
Ah, the elegant dance of dopamine agonists; how truly captivating-indeed, one must consider half‑life, dosing frequency, and side‑effects, all whilst navigating the labyrinthine corridors of modern pharmacology! 😏💊
👍🤷♀️
Building on the earlier points, interdisciplinary collaboration between endocrinology and neurology can streamline medication selection. Sharing monitoring protocols across specialties ensures consistency. It also fosters patient education programs that demystify dosing schedules.
Agreed, a unified approach benefits everyone.