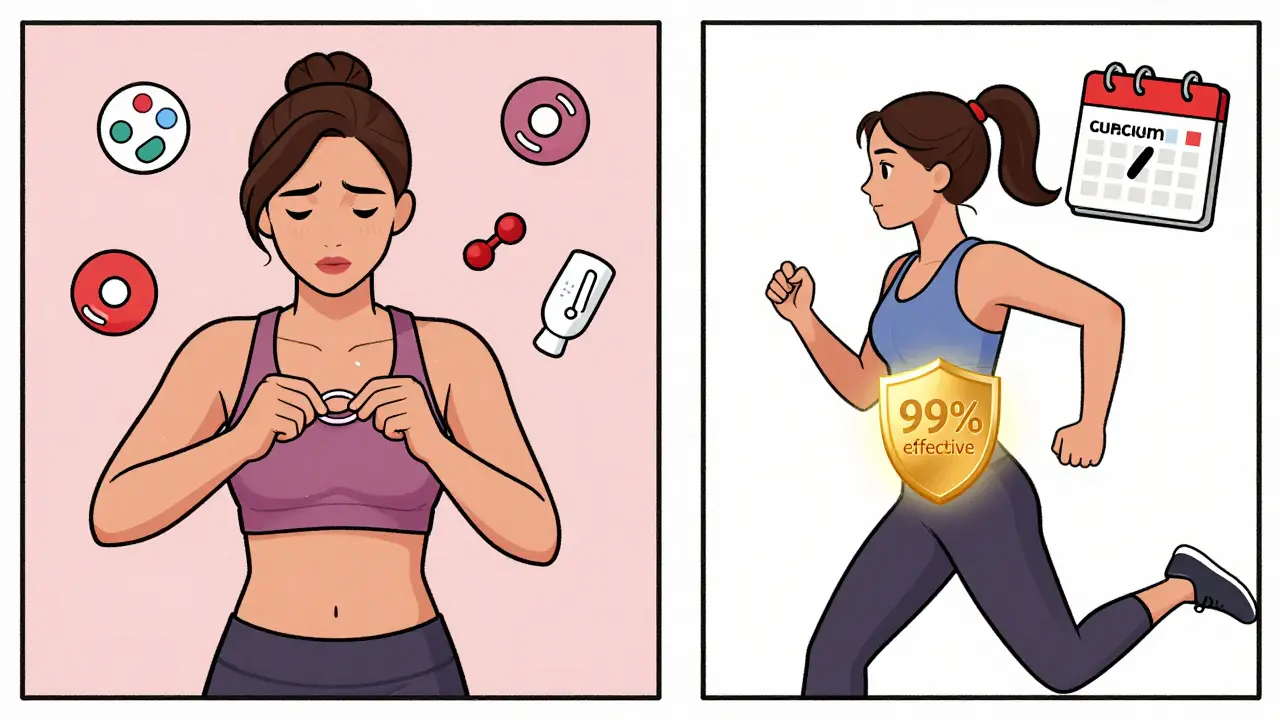
Choosing birth control isn’t just about convenience-it’s about your body, your health, and your life. If you’re weighing the contraceptive patch, vaginal ring, or IUD, you’re not alone. Thousands of women in Australia and beyond face this decision every year. But here’s the thing: not all methods are created equal when it comes to safety and risk. Some carry hidden dangers. Others are nearly foolproof. And the differences aren’t just technical-they can change your daily life, your menstrual cycle, even your long-term health.
How Each Method Works (And Why It Matters)
The contraceptive patch (like Xulane®) sticks to your skin and releases hormones-norelgestromin and ethinyl estradiol-through your bloodstream. You change it once a week for three weeks, then take a break. The vaginal ring (NuvaRing®) works similarly but sits inside your vagina, releasing etonogestrel and ethinyl estradiol daily. You leave it in for three weeks, then remove it for a week.
Neither of these is a daily pill. That’s the appeal. But here’s what most people don’t realize: both deliver more estrogen than the average birth control pill. That’s not a small detail. Higher estrogen means higher risk of blood clots. The FDA has flagged this. So has the contraceptive patch-it’s been linked to a greater chance of dangerous clots in the legs or lungs compared to oral contraceptives, even though exact numbers vary by study.
Now, contrast that with an IUD. There are two types: copper and hormonal. The copper IUD (Paragard®) doesn’t use hormones at all. It releases copper ions that make your uterus hostile to sperm. It lasts up to 12 years. Hormonal IUDs-like Mirena®, Liletta®, Kyleena®, and Skyla®-release tiny amounts of levonorgestrel directly into your uterus. That’s local. Not systemic. Your blood doesn’t get flooded with hormones. That’s why IUDs don’t carry the same clotting risks as the patch or ring.
Real Risks: What the Data Shows
Let’s cut through the marketing. What do the numbers actually say?
For typical use (meaning people forget, lose, or delay), the patch has a 9% failure rate. That’s 9 pregnancies per 100 women in a year. The vaginal ring? About 7%. Both are much higher than the 0.2% failure rate of IUDs. That’s not a typo. IUDs are over 99% effective. One study in JAMA Network Open found that short-acting methods like the patch and ring led to 4.55 pregnancies per 100 women-years. IUDs? Just 0.27. That’s a 16x difference.
Now, the risks. Estrogen-containing methods-patch and ring-raise your risk of venous thrombosis from about 2-10 cases per 10,000 women per year to 7-10. That might sound rare. But when you’re young and healthy, you don’t think about blood clots. Until you’re the one with a swollen leg, chest pain, or a stroke. Women over 35 who smoke? Don’t use these. Women with migraines with aura? Avoid them. That’s not a suggestion-it’s a medical red flag.
What about IUDs? They’re safer for your heart. But they come with their own set of issues. Copper IUDs often make periods heavier and cramps worse. One in two users report bleeding that’s unbearable for the first few months. Hormonal IUDs? The opposite. Many women stop getting periods entirely after six months. But in the first 3-6 months, you might have spotting every few days. It’s messy. It’s unpredictable. And yes, some women panic thinking it’s a sign of something wrong.
Then there’s the procedure. IUD insertion isn’t fun. It feels like intense menstrual cramps, sometimes worse. You might feel dizzy or faint. But it’s over in 5 to 10 minutes. Expulsion (when the IUD comes out on its own) happens in 2-10% of cases, mostly in the first year. Perforation? Extremely rare-less than 1 in 1,000. Infection risk? Highest in the first 20 days after insertion, then drops off. Still, it’s something to watch for.
What Real Women Are Saying
Reddit threads and review sites aren’t clinical trials, but they tell you what no study can: how these methods actually feel in daily life.
One woman switched from NuvaRing to Mirena after three months of migraines with aura. She wrote: “The estrogen was killing me.” Another, who used Paragard for two years, said: “I bled for eight days straight every month. I couldn’t work. I switched to Liletta. Now I have two days of light spotting. I didn’t know life could be this easy.”
On Healthgrades, the patch has a 3.2 out of 5 rating. Why? 42% of users said the adhesive peeled off during exercise or showering. 37% had breakthrough bleeding. The ring? 3.6 out of 5. Some love the convenience. Others say it falls out during sex. One in three reported discomfort.
But IUDs? Mirena scores 3.9 out of 5. 68% say their periods got lighter. Even Paragard, with its 3.5 rating, has 57% of users saying they’d choose it again-because it’s reliable, hormone-free, and lasts a decade. The key? Patience. Most side effects fade after six months.
Cost, Convenience, and Long-Term Thinking
At first glance, the patch and ring seem cheaper. You pay $15 to $80 a month. The ring can cost up to $200 without insurance. But IUDs? Upfront cost is $0 to $1,300. Sounds steep. But spread over five to ten years? That’s less than $10 a month. And you don’t have to remember anything. No weekly application. No monthly insertion. No worrying if the ring slipped out.
Also, timing matters. If you start the patch or ring mid-cycle, you need a backup method for seven days. The copper IUD? Works immediately-even as emergency contraception within five days of unprotected sex. That’s a game-changer.
And here’s something most clinics don’t stress enough: switching methods requires planning. You can’t just take off a hormonal IUD and slap on a patch the same day. You risk hormone overlap, which can cause nausea, spotting, or worse. Always talk to your provider before switching.

Who Should Choose What?
There’s no one-size-fits-all. But here’s a simple guide based on real-world safety and practicality.
- Choose an IUD if: You want the most effective, lowest-risk option. You hate taking daily or weekly action. You have a history of blood clots, migraines with aura, high blood pressure, or smoke. You want long-term freedom. You’re okay with possible heavier periods (copper) or irregular bleeding at first (hormonal).
- Choose the ring if: You want a non-daily method that doesn’t involve a procedure. You don’t have estrogen-related health risks. You’re okay with monthly maintenance and potential vaginal discomfort or expulsion.
- Avoid the patch if: You have any cardiovascular risk factors. You’re active, sweat a lot, or shower often. You don’t want higher estrogen exposure than necessary. You’re under 21-studies show younger women using short-acting methods have nearly double the pregnancy risk.
The American College of Obstetricians and Gynecologists (ACOG) recommends IUDs as first-line contraception for most women. Why? Because they’re safer, more effective, and require less user effort. Dr. Jen Gunter put it simply: “IUDs have the lowest failure rate of any reversible method and don’t carry the blood clot risks associated with estrogen-containing methods.”
What to Do Next
If you’re thinking about switching or starting a new method, don’t just pick what sounds easiest. Ask your provider these questions:
- Do I have any conditions that make estrogen unsafe for me?
- How will this affect my periods? Will I bleed more, less, or stop altogether?
- What’s the risk of expulsion or perforation with an IUD?
- What happens if I forget to change the patch or ring?
- Can I use this if I plan to get pregnant in the next year?
And remember: your body changes. What worked at 22 might not work at 32. Your risk profile changes. Your life changes. That’s okay. Birth control isn’t a one-time decision. It’s an ongoing conversation with your health.
Most women who try IUDs stay on them. Why? Because once the adjustment period is over, they forget they’re even using birth control. And that’s the real win.
Is the contraceptive patch safer than the vaginal ring?
Neither is significantly safer. Both deliver estrogen and carry similar risks for blood clots, especially if you smoke, are over 35, or have migraines with aura. The patch may have a slightly higher clot risk due to higher estrogen levels absorbed through the skin. The ring has a higher chance of expulsion or vaginal discomfort. Neither is recommended as a first choice for most women.
Can IUDs cause infertility?
No. IUDs do not cause infertility. This is a myth. Once removed, fertility returns quickly-often within a month. The only risk is infection shortly after insertion, which, if untreated, could lead to pelvic inflammatory disease (PID). But PID is rare (1-2% in the first 20 days) and preventable with proper screening and care. Most women who use IUDs go on to have healthy pregnancies later.
Which IUD is better: copper or hormonal?
It depends on your goals. Copper IUDs (Paragard) are hormone-free and last up to 12 years. But they often cause heavier, longer periods and worse cramps. Hormonal IUDs (Mirena, Liletta, etc.) reduce bleeding and cramps over time-many users stop getting periods. They last 3 to 8 years depending on the brand. Choose copper if you want no hormones. Choose hormonal if you want lighter periods and fewer cramps.
How soon after removing an IUD can I get pregnant?
You can get pregnant right away. Fertility returns as soon as the IUD is removed. There’s no waiting period. Studies show 80% of women conceive within a year after removal-same as women who never used an IUD. The device doesn’t affect your long-term ability to conceive.
Can I use the patch or ring if I’m breastfeeding?
It’s not recommended in the first 6 weeks postpartum. Estrogen can reduce milk supply. After six weeks, hormonal methods like the patch or ring are usually safe if you’re not exclusively breastfeeding. But progestin-only methods (like the hormonal IUD or implant) are preferred during breastfeeding because they don’t affect milk production. Always check with your provider before starting any hormonal method while nursing.










14 Comments
I used the patch for six months and woke up one morning with a leg like a balloon. No joke. They don't tell you this stuff until you're in the ER. I'm lucky I didn't lose it. Now I have a copper IUD and I forget it's even there. Life is quiet again.
The pharmacokinetic profile of transdermal estrogen delivery via patch versus intravaginal bioavailability via ring reveals a statistically significant elevation in Cmax and AUC for ethinyl estradiol, thereby amplifying thrombotic risk via hepatic first-pass modulation. 🤓 The IUD, by contrast, bypasses systemic circulation entirely-making it the gold standard in hormonal pharmacodynamics. #ScienceWins
In Australia we've got free IUDs through Medicare if you're under 26. Most GPs don't even mention the patch or ring anymore. Too many clot cases. The copper IUD is brutal for the first 3 months but after that? Absolute freedom. No more panic checks every week. Worth the cramps.
You know what's really dangerous? Letting doctors push IUDs on young girls. My cousin got one at 19 and now she's terrified of sex. The system wants you dependent on devices. Natural cycles are healthier. You just need to learn your body. Not let Big Pharma decide for you.
The patch? More estrogen than your grandma’s hormone replacement cocktail. And the ring? Falls out during sex like a goddamn tampon with a mind of its own. Meanwhile the IUD sits there like a silent ninja. No drama. No leaks. No ‘oops I forgot’. It’s not birth control. It’s liberation. The rest? Corporate marketing with a side of thrombosis.
Did you know the FDA hides the real clot stats? They only report what pharma lets them. I read a whistleblower report once. The patch has a 1 in 500 chance of stroke if you're under 25. They don't tell you that. They just say 'rare'. But I know. I saw the emails.
IUDs... are... NOT... safe...!!!... They... can... migrate... into... your... heart...!!!... I... read... it... on... a... forum... with... a... .gov... domain... and... the... admin... had... a... PhD... from... MIT...!!!... Also... the... copper... gives... you... mercury... poisoning...!!!... PLEASE... STOP... THIS... MADNESS...!!!
I think the real issue isn't which method is safer-it's whether we're giving people enough time and space to understand what their body needs. Most of us are rushed into decisions. I tried the ring, hated the spotting, switched to Mirena, had a panic attack thinking I was bleeding out... then realized it was normal. Took six months. Patience matters more than the device.
If you're new to this, don't stress. Talk to your provider, but also talk to women who've been there. I had Paragard for 5 years-cramps were hell at first, but I got used to it. Now I can't imagine going back. It's not about perfection. It's about finding what fits your life. You got this.
It's fascinating how we frame birth control as a personal choice when in reality it's a structural one. The patch and ring require consistent access to healthcare, money, and time-things not everyone has. The IUD, once inserted, becomes a quiet act of autonomy. It doesn't ask you to be perfect. It doesn't judge you for forgetting. It just... works. And maybe that's the real revolution: a device that doesn't require you to be flawless to be free.
I'm from the States and I've seen this play out in clinics across three states. The patch? Used mostly by teens who think it's 'easier'. But they peel it off in the shower, forget to change it, then panic when they get pregnant. The ring? Same thing. The IUD? One visit. One hour. Ten years of peace. I tell every woman I know: if you're not planning to get pregnant soon, get the IUD. It's not just better-it's smarter. And yeah, the insertion hurts. But so does an unplanned baby.
I find it deeply concerning that this article promotes the IUD as a 'first-line' option without acknowledging the psychological trauma associated with insertion. Many women experience PTSD from the procedure. This is not medical advice-it is ideological coercion. The patch, while imperfect, allows for reversible, controlled dosing. Why are we demonizing a method that gives women agency over timing? The IUD is not a moral imperative.
I went from patch to Mirena after three years of spotting, mood swings, and adhesive disasters. I thought I’d be stuck with cramps forever. Nope. Six months later, I had two days of light pink and zero stress. I forgot I was on birth control. Then I remembered-I’m free. If you’re on the fence, try the hormonal IUD. Don’t listen to the horror stories. Wait six months. Your future self will thank you.
The patch is a trap. They make it look easy. Then you’re stuck with a sticky mess on your butt and a blood clot in your lung. I’m not saying IUDs are perfect. But the patch? It’s like giving a toddler a loaded gun and calling it 'convenient'. Don’t be fooled by the marketing. It’s not freedom. It’s a gamble with your life.