When your doctor switches your brand-name blood pressure pill to a generic, you might feel uneasy. Is it really the same? Will it work? Could it hurt you? These aren’t just patient worries-they’re backed by real data, conflicting studies, and years of clinical experience. The truth about cardiovascular generics isn’t simple. It’s not a clear win for brand names, nor is it a flawless win for generics. It’s a nuanced picture shaped by chemistry, manufacturing, patient behavior, and how we measure success.
What Exactly Are Cardiovascular Generics?
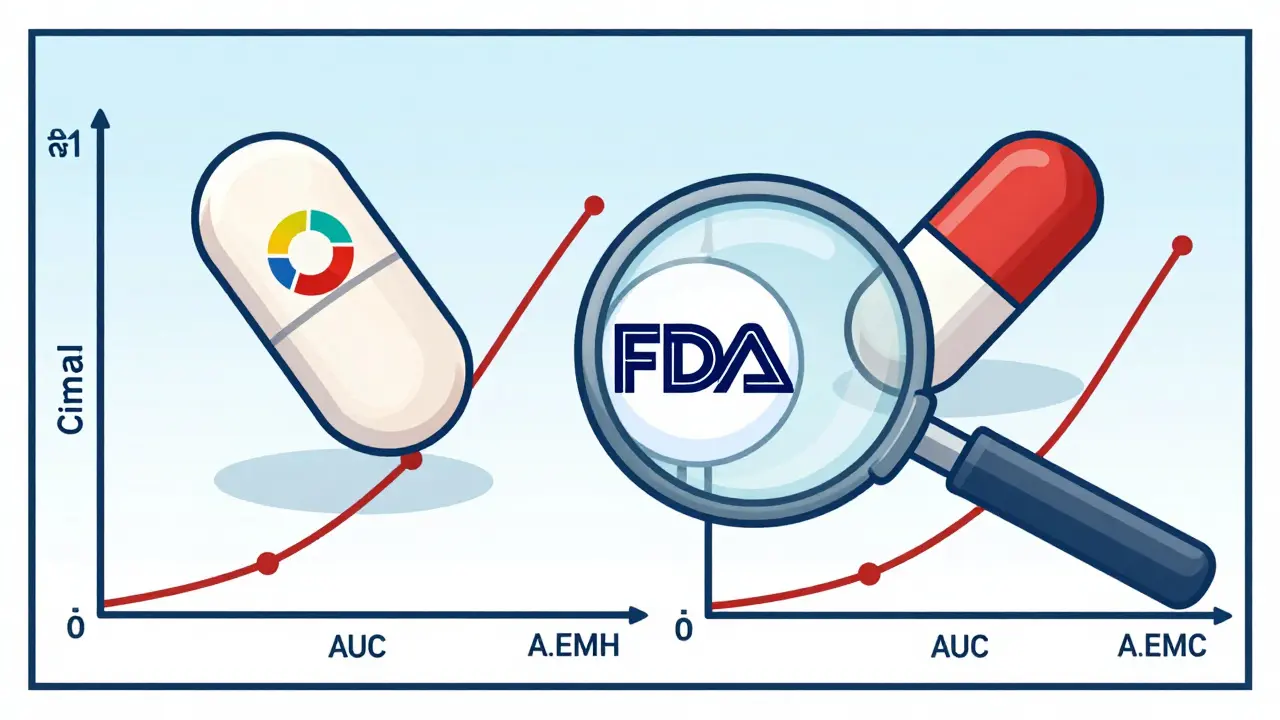
Cardiovascular generics are exact chemical copies of brand-name heart and blood pressure drugs-like losartan, atorvastatin, or metoprolol-released after the original patent expires. The U.S. Food and Drug Administration (FDA) doesn’t require them to repeat the massive clinical trials that brand-name drugs went through. Instead, they must prove bioequivalence: that the body absorbs the active ingredient at nearly the same rate and level as the original. The standard? The 90% confidence interval for absorption (measured by AUC and Cmax) must fall between 80% and 125% of the brand-name drug. In practice, most generics land within 3.5% of the original, according to FDA data from 2021.
That sounds tight. And for most people, it is. But bioequivalence doesn’t mean identical. It means functionally equivalent under controlled lab conditions. The active ingredient is the same. The dose is the same. But the fillers, dyes, coatings, and manufacturing processes? Those can vary. And for some patients-especially those with sensitive systems or complex health conditions-that can matter.
Do Generics Work as Well as Brand Names?
Large studies give a mostly reassuring answer. A 2020 Harvard Health meta-analysis of 38 randomized controlled trials found that 35 of them (92.1%) showed no meaningful difference in outcomes between generics and brand-name cardiovascular drugs. That’s powerful evidence. So why do some studies show the opposite?
One major study published in Circulation: Cardiovascular Quality and Outcomes tracked over 136,000 older adults in Quebec after generic versions of ARBs (losartan, valsartan, candesartan) hit the market. In the first month after switching, adverse events rose-from 10% to 14% for some drugs. That’s not a small uptick. It’s a signal. Researchers didn’t find the generics were less effective at lowering blood pressure. They found more patients had dizziness, kidney issues, or hospital visits. Why? The leading theory: patients’ bodies reacted to subtle formulation changes. Even tiny differences in how a pill dissolves can affect absorption, especially in elderly patients with slower digestion or kidney problems.
Another analysis from 2023, looking at 1.2 million patients, found a small but significant increase in major heart events with generic statins (risk ratio 1.13). At the same time, generic calcium channel blockers showed fewer adverse events (RR 0.90). That’s not random. It suggests that for some drug classes, the formulation matters more than others. Statins are absorbed in the gut, and small changes in coating or particle size can affect how much actually gets into the bloodstream. Calcium channel blockers? Less sensitive to those tweaks.
Why Do Some Patients Have Worse Outcomes?
It’s rarely the drug itself. It’s the switch.
A 2019 JAMA Internal Medicine study found that when patients got a generic version with a different pill color or shape, they were 14.2% more likely to stop taking it altogether. That’s not because the drug didn’t work. It’s because they didn’t recognize it. They thought it was the wrong medicine. Or worse-they thought it was fake. That fear alone can lead to missed doses, which leads to spikes in blood pressure or cholesterol, which leads to hospital visits.
And then there’s the issue of switching back and forth. Some patients get a generic from one pharmacy, then a different generic from another. Each time, the pill looks different. Each time, the body has to re-adapt. That’s not a problem with generics-it’s a problem with how we manage transitions.
One solution? Pharmacist-led medication therapy management. A 2020 pilot study at the University of Pittsburgh showed that when pharmacists sat down with patients, explained why the pill changed, and checked in after two weeks, discontinuation rates dropped by 22.7%. Simple. Human. Effective.
The Manufacturing Reality
Not all generic manufacturers are equal. The FDA inspects facilities, and in 2022, 12.7% of generic drug plants had critical deficiencies. That’s not a scandal-it’s routine oversight. But it matters. In 2018, a contamination crisis hit ARB generics. Nitrosamines-possible carcinogens-were found in valsartan, losartan, and irbesartan. Over 1,200 lots were recalled. The FDA didn’t shut down production. They tightened standards. Now, manufacturers must test for nitrosamines and keep levels below 96 nanograms per day. That’s less than a grain of salt in a swimming pool. But it’s a reminder: quality control isn’t guaranteed. It has to be enforced.
Market leaders like Teva, Mylan, and Sandoz produce the bulk of cardiovascular generics. But smaller manufacturers also compete. And while most are reliable, the pressure to cut costs means some may skimp on testing or use cheaper ingredients. That’s why the FDA’s 2023 Unannounced Inspection Pilot Program found 47.3% of inspected cardiovascular generic facilities had issues-nearly 50% higher than under normal inspections.
What Do Doctors Really Think?
There’s a gap between what the data says and what doctors believe. A 2020 American College of Physicians analysis found that 25% of physicians say they wouldn’t use generics for their own families. Half of medical journal editorials express hesitation. Yet, 89.4% of community pharmacists say generics are just as safe and effective.
Why the disconnect? For many doctors, it’s personal. They’ve seen patients crash after a switch. They’ve seen a 75-year-old with heart failure get dizzy after switching to a new generic ARB. They’ve seen lab results spike after a change in pill appearance. That’s not theory-that’s lived experience. And it’s hard to dismiss.
At the same time, cardiologists are under pressure to reduce costs. Medicare Part D plans achieve nearly 90% generic use for heart drugs. Commercial insurers are lower-around 76%. The financial incentive is real. But so is the risk of unintended harm.
When to Stick with Brand Names
Not every patient should be switched. The American Heart Association recommends caution with drugs that have a narrow therapeutic index-where small changes in blood levels can cause big problems. That includes:
- Warfarin (blood thinner)
- Some antiarrhythmics
- High-dose statins in patients with unstable cholesterol
For these patients, consistency matters more than cost. If you’re stable on a brand-name drug and doing well, switching might not be worth the risk. And if you’ve had a bad reaction to a generic before? Don’t try again.
What You Can Do
If you’re on a cardiovascular generic:
- Don’t panic. Most people do fine.
- Keep your pill bottle. Note the color, shape, and imprint. If it changes unexpectedly, ask your pharmacist why.
- Track how you feel. Dizziness? Fatigue? Swelling? Report it. It’s not "just in your head."
- Ask your pharmacist to explain the switch. They’re trained to help you understand.
- If you’re on warfarin or another narrow-therapeutic-index drug, ask your doctor if you should stay on brand.
If you’re a clinician:
- Don’t assume all generics are interchangeable. Know your drug class.
- Don’t switch without talking to the patient. Explain why.
- Monitor closely for the first 30 days after a switch.
- Respect patient concerns. They’re not irrational-they’re based on real experiences.
The Bottom Line
Cardiovascular generics are safe and effective for the vast majority of people. The data supports it. The savings are massive-$300 billion in the U.S. alone over the last decade. But safety isn’t just about chemistry. It’s about consistency, communication, and care. A pill that works perfectly in a lab can fail in a person’s body if the transition isn’t handled well.
Generics aren’t inferior. But they’re not identical. And treating them as if they are is where the risk lies.
Are generic heart medications as safe as brand names?
For most people, yes. Large studies show 92% of the time, generic cardiovascular drugs produce the same clinical results as brand-name versions. However, a small but significant number of patients-especially older adults or those with complex conditions-experience more side effects after switching. This isn’t because the active ingredient is weaker, but because of differences in fillers, coatings, or how the pill dissolves in the body. The risk is low overall, but it’s real for some.
Why do some studies show worse outcomes with generics?
Some studies, like the 2019 Quebec study, found a spike in hospital visits and side effects in the first month after switching to generic ARBs. The leading explanation is that patients’ bodies reacted to small formulation changes-like different dyes or binders-especially when switching multiple times or when patients were already fragile. The problem wasn’t the drug’s effectiveness, but the transition process. When pharmacists helped patients understand the switch, adverse events dropped.
Can I trust generic statins?
Most generic statins are safe and effective. But a 2023 meta-analysis found a small but significant increase in major heart events (13% higher risk) with some generic statins compared to brand names. This may be due to differences in how the drug is absorbed-statins are sensitive to coating and particle size. If you’re on a generic statin and your cholesterol levels have gone up or you’re feeling worse, talk to your doctor. Don’t assume it’s just your lifestyle.
What should I do if my generic pill looks different?
Don’t stop taking it. Call your pharmacist. Pill appearance changes are common with generics-different manufacturers use different colors, shapes, or logos. But if you’ve had side effects after a change, or if you’re unsure, ask for the name of the manufacturer. You can ask to stick with one brand of generic if you’re doing well. Pharmacists can help you track which version you’re on and alert you to changes.
Are there any cardiovascular generics I should avoid?
You shouldn’t avoid generics outright. But for drugs with a narrow therapeutic index-like warfarin, certain antiarrhythmics, or high-dose statins in unstable patients-switching can be risky. If you’re stable on a brand-name version and doing well, there’s no need to switch. Always talk to your doctor before changing, especially if you’ve had heart attacks, strokes, or kidney problems in the past.
How can I tell if my generic is from a reliable manufacturer?
You can’t always tell just by looking. But you can ask your pharmacist which company makes your generic. Major manufacturers like Teva, Mylan, and Sandoz have better track records. You can also check the FDA’s website for inspection reports (though it’s technical). If you’ve had a bad reaction, report it to the FDA’s MedWatch program. Your report helps improve safety for everyone.
What Comes Next?
The future of cardiovascular generics isn’t about cost anymore. It’s about precision. The FDA is now requiring advanced testing for complex generics-especially drugs like rivaroxaban and sacubitril/valsartan, which are just starting to go generic. The European Medicines Agency already requires food-effect studies to make sure the drug works the same whether taken with or without meals.
Manufacturers are also under more scrutiny. Unannounced inspections are rising. And patient education is becoming part of the standard of care. The goal isn’t to stop generics. It’s to make sure every switch is safe, informed, and intentional.
For you, the patient, that means staying informed. For your doctor, it means listening. And for the system, it means valuing safety as much as savings.











11 Comments
Okay, but let’s be real-my grandma switched to a generic lisinopril and started feeling like a zombie. Not because it didn’t work, but because the new pill was a tiny, neon-green capsule that looked like it came from a sci-fi movie. She stopped taking it for three days. Three days. Her BP spiked so high the EMTs came. She didn’t even know it was the same drug. The color change freaked her out. We need better labeling. Like, actual human instructions on the bottle. Not just ‘generic’ in tiny print.
Ugh, I knew this would happen. Big Pharma doesn’t want you to know how sketchy generics are. My uncle had a stroke after switching to a generic statin-*and* the pharmacy didn’t even tell him it changed. They just handed him a different pill. No warning. No explanation. That’s not healthcare, that’s corporate negligence. And now they want us to trust these ‘FDA-approved’ pills that are made in some basement factory in India? Please. I’d rather pay $200 a month than risk my life for a $5 pill.
As someone from India where generics are the only option for most people, I’ve seen this firsthand. My dad’s been on generic atorvastatin for 8 years-no issues. But I also know people who switched brands and got dizzy. It’s not the drug-it’s the *switching*. If you’re stable, don’t mess with it. If you need to switch, talk to your pharmacist. They’re the real MVPs here. And yes, Teva and Sandoz are way more reliable than the random small labs. Just ask for the manufacturer name.
I appreciate how balanced this post is. It’s easy to get swept up in fear or cheerleading, but the truth is messy. The data says generics are mostly fine. The lived experience says some people pay a price. That’s why we need systems-not just prescriptions. Pharmacist check-ins, consistent pill appearance, patient education. It’s not about distrust. It’s about dignity. People deserve to understand what’s in their body, even if it costs a little more.
Here’s the thing-most of us in India take generics because we have no choice. But we also know which brands work. My aunt takes only Teva’s metoprolol. Why? Because she tried three others and two made her dizzy. So now she only gets the one with the red cap. It’s not about brand loyalty-it’s about survival. And honestly? If the FDA lets companies skip food-effect studies for complex generics, that’s a red flag. Blood pressure meds aren’t aspirin. They need real-world testing.
Let’s be precise: bioequivalence does not imply pharmacodynamic equivalence. The 80–125% AUC/Cmax window is a statistical artifact designed for regulatory expediency, not clinical omniscience. When you introduce inter-individual variability-particularly in elderly patients with polypharmacy, renal insufficiency, or altered gastric motility-the margin of error becomes clinically significant. Furthermore, the FDA’s inspection compliance rate of 52.7% for unannounced audits suggests systemic fragility. To claim generics are ‘just as safe’ is to conflate regulatory approval with therapeutic fidelity. The data is not as clean as you’re implying.
My dad’s on generic warfarin and he’s fine-so I get why people say it’s okay. But I also saw my neighbor’s mom go to the ER after switching to a new generic ARB. She didn’t know the pill looked different. She thought it was a mistake. So she skipped doses. That’s the real problem-not the drug, but the lack of communication. If your pharmacist sits down with you for 5 minutes and says, ‘Hey, this is the same medicine, just a different look,’ it cuts the panic in half. Simple. Human. Effective. Why isn’t this standard?
How utterly predictable. The same people who champion ‘affordable healthcare’ suddenly become panic-stricken when the price drops below $10. This is the same logic that made people fear GMOs, vaccines, and microwave ovens. You don’t get to cherry-pick science based on your emotional comfort. The FDA doesn’t approve drugs based on how they *feel*. They approve them based on data. And the data is clear: 92% of the time, generics perform identically. If you’re one of the 8%, then fine-stay on brand. But don’t weaponize your personal anecdote to scare everyone else into paying more.
My cousin’s a pharmacist in Mumbai-he says the real issue isn’t generics. It’s the *switching*. One week it’s Teva, next week it’s Sun Pharma, then back to Mylan. Patients get confused. They think the medicine is changing. They stop. They panic. The solution? One generic brand per patient, per drug, forever. If they need to switch, the pharmacist should log it, explain it, and follow up. No one’s doing that. And that’s on the system-not the drug. We need to treat patients like humans, not inventory.
Just wanted to say-I switched to a generic metoprolol last year. No problems. But I kept the old bottle. I noticed the new one was a different shape, so I asked my pharmacist. She told me it was made by Teva now, not Mylan. She even printed out a little sheet with the differences. I didn’t even know that was a thing. It made me feel way more in control. Maybe we need a ‘generic switch card’-like a little insert that says: ‘This is the same drug. Here’s what changed.’ Simple. Helpful. No drama.
Let me be crystal clear: if you’re taking a generic statin and your LDL hasn’t dropped by 50% in 30 days, you’re being duped. The FDA’s 80–125% bioequivalence standard is a joke. Real science requires 95–105%. Any deviation above 5% is a pharmacological gamble. And don’t get me started on nitrosamine contamination. You think 96 nanograms is safe? That’s like saying ‘a single drop of poison in an Olympic pool’ is fine. It’s not. It’s negligence. And anyone who says generics are ‘just as good’ hasn’t read the actual lab reports. I have. And I’m not impressed.