Not all beta-blockers are the same. Even though they all work by blocking adrenaline, the differences between them can mean the difference between better control of your heart condition and unwanted side effects. If you’ve been prescribed a beta-blocker, knowing why your doctor picked one over another isn’t just helpful-it’s critical.
What Beta-Blockers Actually Do
Beta-blockers stop adrenaline and noradrenaline from binding to beta receptors in your heart and blood vessels. This slows your heart rate, lowers blood pressure, and reduces how hard your heart has to pump. That’s why they’re used for heart attacks, heart failure, high blood pressure, and irregular heartbeats.
But here’s the thing: blocking adrenaline doesn’t just affect your heart. These receptors are also in your lungs, blood vessels, and even your brain. So the type of beta-blocker you take determines whether you get the benefits without the side effects.
The Three Generations of Beta-Blockers
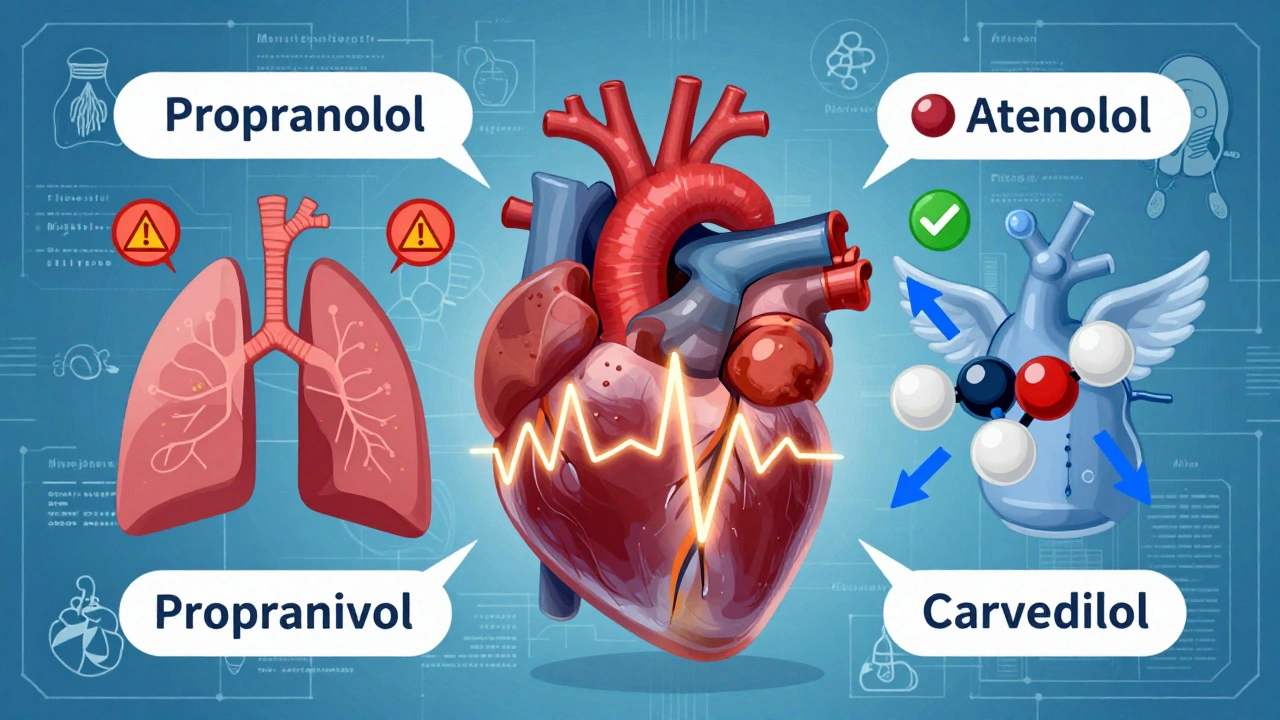
Beta-blockers are grouped into three generations based on what they target and how they work.
First-generation drugs like propranolol block both beta-1 and beta-2 receptors. That means they hit your heart, but also your lungs. For someone with asthma or COPD, this can trigger breathing problems. Propranolol is still used for migraines and tremors, but it’s rarely the first choice for heart conditions today.
Second-generation beta-blockers-like atenolol, metoprolol, and bisoprolol-are more selective. They mainly target beta-1 receptors in the heart. That makes them safer for people with lung issues. But even among these, there are differences. Metoprolol comes in two forms: immediate-release (taken twice a day) and extended-release (once daily). The extended version is preferred because it keeps levels steady and reduces side effects like fatigue and dizziness.
Third-generation beta-blockers-carvedilol and nebivolol-do more than just block adrenaline. Carvedilol also blocks alpha receptors, which helps relax blood vessels. Nebivolol boosts nitric oxide, a natural chemical that dilates arteries. Both lead to better blood flow and less strain on the heart.
Why Heart Failure Patients Need Specific Types
If you have heart failure with reduced ejection fraction (HFrEF), not just any beta-blocker will do. Only three have been proven to lower your risk of dying: carvedilol, bisoprolol, and metoprolol succinate (the extended-release form).
Why? Because they don’t just slow the heart-they help the heart heal. Carvedilol reduces oxidative stress by 30-40% in heart tissue, according to animal studies. Nebivolol has antioxidant and anti-fibrotic effects that prevent scar tissue from forming in the heart muscle. These aren’t minor perks. In the US Carvedilol Heart Failure Study, patients taking carvedilol had a 35% lower risk of death compared to those on placebo.
That’s why guidelines from the European Society of Cardiology and the American College of Cardiology say: if you have heart failure, you need one of these three. Not propranolol. Not atenolol. These older drugs don’t offer the same survival benefit.

Side Effects Vary Wildly Between Drugs
Side effects aren’t the same across all beta-blockers. Many people assume fatigue, cold hands, or depression are just part of the package. But that’s not true.
On patient review sites, propranolol has a 6.2/10 average rating. Nearly 40% of users report moderate to severe side effects: sleep issues, depression, or trouble exercising. That’s because it crosses the blood-brain barrier and affects the central nervous system.
Compare that to bisoprolol, rated 7.1/10. Only 18% report sleep problems, and just 11% feel depressed. It doesn’t cross into the brain as easily, so it’s gentler on mood and energy.
Another big difference: sexual function. Men on traditional beta-blockers often report erectile dysfunction. But in Reddit communities, 65% of men over 50 taking nebivolol said their sexual function improved or stayed the same. That’s because nebivolol increases nitric oxide-which also helps with blood flow to the genitals.
And let’s talk about cold hands. About 30% of people on propranolol or atenolol report this. But with carvedilol and nebivolol, it’s far less common. Why? Their vasodilating effect keeps blood flowing to the extremities.
Why Dosing and Formulation Matter
Metoprolol tartrate and metoprolol succinate are the same drug-but not interchangeable. Tartrate is taken twice daily. Succinate is once daily. The extended-release version gives steadier levels, fewer peaks and crashes, and better tolerance.
Carvedilol requires slow titration. You start at 3.125 mg twice daily and increase slowly over 8-12 weeks. Rushing this can cause dizziness or low blood pressure. But bisoprolol can be increased faster-often over 4-8 weeks.
That’s why your doctor doesn’t just pick a drug. They pick a regimen. And if you’re struggling with side effects, it might not be the drug-it’s the dose or how fast you got there.
What to Avoid
If you have asthma or COPD, avoid nonselective beta-blockers like propranolol and sotalol. Even cardioselective ones carry some risk. Always tell your doctor about breathing issues before starting any beta-blocker.
Never stop a beta-blocker cold turkey. The FDA warns that sudden withdrawal can spike your heart attack risk by 300% in the first two days. If you need to stop, your doctor will taper you down over weeks.
Also, avoid combining nonselective beta-blockers with rescue inhalers like albuterol. Beta-blockers can block the effect of these inhalers by up to 50%, making an asthma attack harder to treat.

What’s New in 2025
The beta-blocker field is evolving. In 2023, the FDA approved entricarone, a new drug that combines beta-3 agonism with beta-1 blockade for heart failure with preserved ejection fraction (HFpEF). Early results show a 22% drop in hospitalizations.
By 2024, combination pills like nebivolol/valsartan will be available-merging a beta-blocker with an ARB to simplify treatment for high blood pressure and heart failure.
Even more exciting: the GENETIC-BB trial is testing whether your genes can predict which beta-blocker will work best for you. That could mean personalized prescriptions instead of trial and error.
How to Talk to Your Doctor
If you’re on a beta-blocker and not feeling well, ask these questions:
- Is this the right type for my condition?
- Could switching to a third-generation agent help my side effects?
- Is there a once-daily version available?
- Should I be tested for lung issues before continuing?
Don’t assume fatigue or cold hands are normal. Many patients feel better after switching from propranolol to bisoprolol or carvedilol.
And if you’re on one of the older drugs for high blood pressure alone-ask if you still need it. Since 2023, major guidelines no longer recommend beta-blockers as first-line for uncomplicated hypertension. ACE inhibitors, ARBs, or calcium channel blockers often work better with fewer side effects.
Bottom Line: It’s Not One Size Fits All
Beta-blockers aren’t interchangeable. Your heart failure, lung health, age, and even your sex can change which one is right for you. Propranolol might be fine for migraines. Carvedilol might save your life in heart failure. Nebivolol might help your blood pressure and your sex life.
The key is matching the drug to the person-not just the diagnosis. If you’re unsure why you’re on a certain beta-blocker, ask for the reasoning. You deserve a treatment that works, not just one that’s been around the longest.
Can I take beta-blockers if I have asthma?
It depends. Nonselective beta-blockers like propranolol can trigger severe breathing problems and should be avoided. Cardioselective beta-blockers like bisoprolol or metoprolol are safer, but still carry some risk. Always tell your doctor about asthma or COPD before starting. In some cases, a third-generation agent like nebivolol may be preferred due to its minimal impact on airways. Never use rescue inhalers like albuterol while on nonselective beta-blockers-they may not work properly.
Why is carvedilol preferred for heart failure over metoprolol?
Carvedilol is preferred because it does more than block beta receptors-it also blocks alpha receptors, which helps relax blood vessels and reduce heart strain. Studies show it reduces mortality by 35% compared to placebo. It also has strong antioxidant properties that reduce heart tissue damage. While metoprolol succinate is also effective, carvedilol’s dual action gives it an edge in improving long-term outcomes, especially in moderate to severe heart failure.
Do beta-blockers cause depression?
Some beta-blockers can, but not all. Propranolol crosses into the brain and has been linked to depression in up to 19% of users. Newer agents like bisoprolol and nebivolol don’t cross the blood-brain barrier as easily, so depression rates are much lower-around 11%. If you’re feeling down after starting a beta-blocker, talk to your doctor. Switching to a more selective agent often helps.
Can beta-blockers help with erectile dysfunction?
Most traditional beta-blockers worsen erectile dysfunction. But nebivolol is an exception. It increases nitric oxide, which improves blood flow-not just to the heart, but to the genitals. Studies and patient reports show that 65% of men over 50 on nebivolol report improved or unchanged sexual function, compared to only 35% on older beta-blockers. If ED is a concern, ask if nebivolol is an option.
Why are beta-blockers no longer first-line for high blood pressure?
Because other drugs lower central aortic pressure more effectively and have fewer side effects. Beta-blockers reduce blood pressure mainly by slowing the heart and lowering cardiac output, but they don’t relax arteries as well as ACE inhibitors or calcium channel blockers. Studies show they lower central pressure by only 5-7 mmHg, while other drugs drop it by 10-12 mmHg. That’s why guidelines now recommend them only for patients with heart failure, post-heart attack, or arrhythmias-not for simple high blood pressure without other conditions.
Is it safe to stop beta-blockers suddenly?
No. Stopping abruptly can cause a rebound surge in adrenaline, increasing your risk of heart attack by 300% within the first 48 hours. Even if you feel fine, never stop on your own. Your doctor will slowly lower your dose over weeks to prevent dangerous spikes in heart rate and blood pressure. Always follow their tapering plan.
Which beta-blocker has the fewest side effects?
Bisoprolol and nebivolol generally have the lowest rates of side effects like fatigue, depression, and cold hands. Bisoprolol is highly selective for the heart and doesn’t cross into the brain much. Nebivolol adds vasodilation, which helps with circulation and reduces cold extremities. Both are better tolerated than propranolol or atenolol. Patient ratings consistently show higher satisfaction with these two.











9 Comments
I was on propranolol for migraines and it turned me into a zombie who couldn’t climb stairs without gasping. Switched to bisoprolol and suddenly I could breathe again and even go for walks. My doctor didn’t even explain the difference until I asked. Don’t let them just hand you the old stuff.
beta blockers are just another way pharma keeps people dependent on meds
My dad had heart failure and they put him on carvedilol. He was tired at first but after 6 weeks he started gardening again. He says it felt like his heart finally stopped fighting him. I wish more doctors talked about this kind of stuff before prescribing.
Let me guess the FDA approved entricarone because someone’s cousin works at a pharmaceutical board. They’ve been pushing beta-blockers for decades while ignoring lifestyle fixes. You think your heart failure is fixed because you’re on a pill? You’re just delaying the inevitable while paying $300 a month. Wake up. The real cure is diet, movement, and stress reduction - not another chemical bandaid wrapped in a clinical trial.
NEBIVOLOL CHANGED MY LIFE 😭 I was on metoprolol and my sex life was GONE. My wife thought I was cheating. Then I switched to nebivolol and boom - we’re back to Friday night movies and cuddling. Also my hands aren’t icy anymore. Why isn’t this the FIRST option???
I’ve been on atenolol for 12 years and I’m fine. Why are you all acting like this is some big revelation? I don’t need to hear about carvedilol or nitric oxide. I take my pill, I don’t feel bad, so stop trying to scare people.
It’s funny how we treat drugs like they’re magic wands. We don’t ask why the body needed adrenaline to begin with. We just suppress it. But what if the problem isn’t the adrenaline? What if it’s the inflammation, the chronic stress, the silence we live in? The beta-blocker is a temporary shield, not a solution. We treat symptoms like crimes instead of signals. And then we wonder why people stay sick.
Wait - you’re telling me that propranolol causes depression, and nebivolol improves sexual function? So… if you’re a man over 50 and you’re on propranolol, you’re not just at risk for heart issues - you’re at risk for being a sad, cold, impotent shell? And your doctor didn’t tell you this? That’s not just negligence - that’s medical malpractice. Someone should sue.
So if you have asthma, you can’t use any beta-blocker - but if you have heart failure, you must use one of three specific ones. So it’s safe for some, dangerous for others. That’s not science. That’s a lottery. And you’re telling me this is personalized medicine? What a joke.