When a pharmacist hands you a pill bottle labeled with your name and a prescription for combination drug substitution, you might assume it’s just a cheaper version of what your doctor ordered. But in reality, swapping one combination medication for another isn’t as simple as switching brands of aspirin. These multi-drug pills-like ATRIPLA, which combines three antiretrovirals, or the combo of pembrolizumab and lenvatinib used in cancer care-are designed as precise, tested units. And replacing them without careful oversight can be risky, legally murky, and sometimes dangerous.
What Exactly Is a Combination Drug?
A combination drug isn’t just two pills in one bottle. It’s a single dosage form-tablet, capsule, or injectable-that contains two or more active ingredients meant to work together. These aren’t random mixes. They’re carefully developed to improve adherence, reduce side effects, or enhance effectiveness. For example, a heart patient might take a pill that combines a blood pressure drug with a cholesterol-lowering statin. Instead of swallowing four pills a day, they take one. That’s the goal: simplicity. But here’s the catch: each ingredient in that pill has its own dosing, absorption rate, and interaction profile. Change even one component, and the whole system can shift. The FDA defines these as combination products when they include drugs, biologics, or devices in one package. That means regulatory rules get complicated fast.Why Can’t Pharmacists Just Swap Them Like Regular Generics?
Generic substitution is straightforward when it’s one drug. If your doctor prescribes Lipitor (atorvastatin), a pharmacist can legally give you a generic version with the same active ingredient, same dose, same form. It’s been proven equivalent. But with combination drugs, that rule breaks down. Let’s say your prescription is for a pill with Drug A and Drug B. The pharmacy doesn’t have that exact combo. They have a pill with Drug A, Drug B, and Drug C. Or worse-they have a pill with Drug A and Drug D instead of Drug B. Is that okay? Under most state laws, no. Pharmacists can’t substitute a combination product unless the alternative contains exactly the same active ingredients in the same amounts. That’s called pharmaceutical equivalence. Even if Drug D is clinically similar to Drug B, adding or removing an ingredient changes the product’s regulatory status. You’re no longer substituting-you’re prescribing. The Alberta College of Pharmacy puts it plainly: substituting a single drug with a combination product is initiating new therapy. That requires a doctor’s approval. Pharmacists aren’t licensed to do that on their own.The Legal Patchwork Across States
There’s no federal law governing substitution of combination products. Instead, 50 states have their own rules-and they don’t match up. Some allow pharmacists to swap generic versions of a combination drug if they’re identical in composition. Others don’t allow any substitution at all unless the prescriber checks a box saying “dispense as written.” Texas requires pharmacists to notify patients and document every substitution. California lets pharmacists substitute if the product is on an approved list. In contrast, New York treats combination products as non-substitutable unless the prescriber explicitly allows it. This creates real problems. A patient moves from Florida to Colorado. Their prescription for a heart combo pill gets filled in their new state-but the pharmacy can’t find an exact match. Do they call the doctor? Wait days? Or risk giving the wrong combo? Many pharmacists say they’ve had to refuse substitution out of fear of liability. A 2022 survey by the National Community Pharmacists Association found that 68% of independent pharmacists ran into substitution dilemmas at least once a month. Nearly half said they’d refused a substitution because they weren’t sure if it was legal.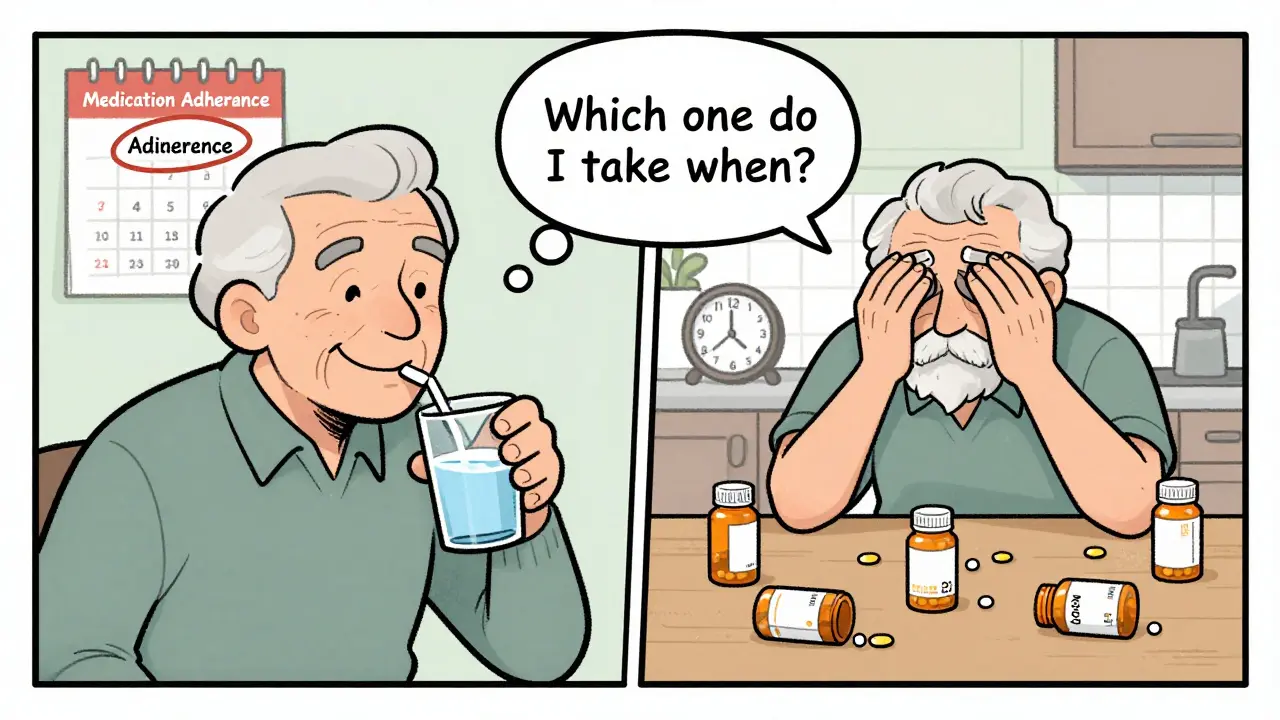
Therapeutic Substitution: When ‘Similar’ Isn’t Good Enough
Some people think, “If Drug B and Drug D both lower blood pressure, why not swap them?” That’s therapeutic substitution-replacing one drug with another that does the same job. But for combination products, this is where things get dangerous. The European Medicines Agency warns against therapeutic substitution for drugs with narrow therapeutic indexes-where tiny dose changes cause big side effects. Think blood thinners, seizure meds, or heart rhythm drugs. Many combination pills contain these. Swap one ingredient, and you could trigger a stroke, arrhythmia, or overdose. Even if the drugs are similar, their interaction with the other component might be different. For example, a combo pill with a diuretic and a beta-blocker might be designed so the diuretic offsets the beta-blocker’s side effect. Replace the beta-blocker with another one, and that balance breaks. The patient might get dizzy, fatigued, or worse. The Therapeutic Substitution Consensus Group, made up of European experts in pharmacology and ethics, says economic pressure shouldn’t drive these swaps. “When switches are made purely to save money,” they warn, “patient safety can suffer.”Cost Savings vs. Patient Risk
It’s easy to see why substitution is tempting. Combination drugs are expensive. A single pill with three drugs can cost $500 a month. Generic single-drug versions might cost $10 each. If you could buy three generics separately, you’d save hundreds. But here’s the problem: those generics aren’t packaged together. You’d have to take them at different times, remember different schedules, and risk interactions you didn’t plan for. Plus, many patients-especially older adults with memory issues-won’t take them correctly. Studies show adherence drops by 30% when pill burden increases. The Institute for Clinical and Economic Review estimates that smart substitution could cut medication costs by 15-25% for chronic conditions. But the American Heart Association counters that inappropriate swaps could lead to adverse events in up to 8% of patients, especially seniors with multiple conditions. Meanwhile, the Medicare Part D redesign encourages substitution where safe. But “where safe” isn’t defined. That leaves pharmacists guessing.What’s Changing? New Guidelines and Legal Battles
The FDA noticed the confusion. In September 2022, they released draft guidance on how to prove therapeutic equivalence for fixed-dose combinations. That’s a step toward clearer rules. In March 2023, the National Association of Boards of Pharmacy proposed a new model law that divides combination products into two categories: simple (two established drugs) and complex (novel mechanisms or narrow therapeutic index). Under this proposal, simple combos could be substituted more freely-like generics. Complex ones? Not without a doctor’s OK. It’s a practical split that matches real-world risk. Legal cases are pushing change too. In Smith v. CVS Caremark (2022), a court ruled that pharmacists cannot substitute a combination product containing extra active ingredients not prescribed. That decision reinforced that substitution isn’t permission to modify a prescription-it’s permission to swap identical products. The European Commission has made harmonizing substitution rules for combination medicines a top priority. In the U.S., some states are following suit. But progress is slow.
What Should Patients Do?
If you’re on a combination drug:- Ask your doctor if your pill is a fixed-dose combination and why it was chosen.
- Don’t assume a cheaper version is safe. Ask your pharmacist if the substitute has the exact same ingredients.
- If your pharmacy says they can’t fill your prescription exactly, insist they contact your prescriber. Don’t settle for a different combo.
- Keep a list of all your meds-especially combo pills-and bring it to every appointment.
What Should Pharmacists Do?
Pharmacists are on the front lines. Here’s what they need to do:- Know your state’s substitution laws-don’t guess.
- When in doubt, don’t substitute. Call the prescriber.
- Document every decision. If you refuse substitution, write why.
- Use the FDA’s list of approved combination products and their equivalents. Don’t rely on vendor claims.
What’s Next?
By 2025, experts predict 35% of all new drug approvals will be combination products. That’s not a trend-it’s the future of treating chronic diseases like diabetes, heart failure, and HIV. But our substitution laws were built for single drugs in the 1980s. They’re outdated. The solution isn’t to ban substitution. It’s to update it. Clear rules. Better training. Federal guidance. And above all, respect for the fact that a combination pill isn’t just a bundle of drugs. It’s a carefully engineered treatment. Patients deserve access to affordable meds. But they also deserve safe ones. The challenge isn’t choosing between cost and care-it’s building a system that delivers both.Can a pharmacist substitute a combination drug without the doctor’s permission?
Only if the substitute contains the exact same active ingredients in the same amounts and dosage form. If the alternative includes additional drugs, removes one, or changes the formulation, it’s considered a new prescription. Pharmacists cannot legally make that change without explicit authorization from the prescriber. Many states require the original prescription to say "dispense as written" to prevent substitution.
Why can’t I just buy the individual drugs in the combo pill separately to save money?
While buying separate generics may cost less, it increases pill burden and reduces adherence. Many patients-especially older adults-forget to take multiple pills at different times. Combination pills are designed to improve compliance. Also, some combo drugs have specific release mechanisms (like extended-release coatings) that can’t be replicated by taking individual pills. Mixing and matching could lead to unsafe drug levels or missed doses.
Are all combination drugs non-substitutable?
No. Some combination products, especially those with two well-established generic drugs (like amlodipine and atorvastatin), may have FDA-approved generic equivalents. If the generic combo contains the exact same active ingredients, dosage, and formulation, substitution may be allowed under state law. But for newer, complex combinations-especially those with novel mechanisms or narrow therapeutic indexes-substitution is rarely permitted without prescriber approval.
What’s the difference between generic substitution and therapeutic substitution?
Generic substitution means replacing a brand-name drug with a generic version that has the exact same active ingredient. Therapeutic substitution means replacing one drug with a different drug that treats the same condition-like switching from lisinopril to losartan for high blood pressure. For combination drugs, therapeutic substitution is extremely risky because changing one component can disrupt the entire drug interaction. Most state laws allow generic substitution only, not therapeutic substitution, for combo products.
How do I know if my combination drug has a generic substitute?
Ask your pharmacist or check the FDA’s Orange Book, which lists approved drug products with therapeutic equivalence evaluations. Not all combination drugs have generics-even if each individual ingredient is available as a generic, the fixed-dose combination may not be approved as equivalent. Only FDA-approved generic versions can be legally substituted. Never assume a combo has a generic just because the parts are cheap.













10 Comments
Man, I've seen this play out in my clinic in Delhi - old folks trying to juggle 5 different pills just because the combo was 'too expensive.' One guy missed his dose for 3 days and ended up in ER. These combo pills? They're not just convenience - they're lifesavers for people who can't keep track of anything.
Yea but lemme tell u somethin - pharmacists in India swap combos all the time n nobody blinks. Why? Because the system's broken. If the brand costs $500 and the generics cost $15 total, people will take the generics even if they're not 'approved.' Safety? Nah. Survival comes first. The system should adapt to reality, not the other way around.
So let me get this straight - we're protecting patients from saving money? This is why America is collapsing.
They're just scared of liability. If you let pharmacists swap, you save billions. But nope - let’s make every patient call their doctor for a 5-cent change. This isn't healthcare, it's litigation theater.
Let’s be real - if you're on a combo pill with a narrow therapeutic index, you're not some DIY biohacker. You're a walking clinical trial. Swapping isn't 'cost-saving,' it's Russian roulette with your heart rhythm. The FDA’s draft guidance? Finally something that makes sense. Let’s classify, not generalize.
They dont want you to know this but the big pharma lobby owns every state board and the FDA too. They profit off these combo drugs because theyre expensive and hard to copy. Thats why they fight substitution so hard. Its not about safety its about profit. And theyll scare you with stroke stories to keep you paying 500 a month
OMG I JUST REALIZED THIS IS WHY MY GRANDMA HAD A STROKE 😭😭😭
She took her combo pill for 6 months then the pharmacy gave her a "cheaper version" and she didn't know it was different!! She thought it was the same!!
Now she's in a nursing home and I'm never trusting a pharmacist again. I'm bringing my own pills from the doctor's office in a Ziploc bag. I'm done.
THIS IS A SCAM. A BIG, FAT, MEDICAL SCAM.
And don't tell me "it's legal" - if it kills people, it's evil.
Someone needs to sue everyone. Like, now. 🚨💔
As someone from India, I see this every day... In the U.S., you have regulations, but in developing nations, we have desperation. People split pills. They mix generics. They take them at different times. They die quietly. Maybe the answer isn't more laws - maybe it's better access, not more bureaucracy. We need affordable combos, not legal gray zones.
Also, spelling: 'combination' has two 'n's. Just saying.
Interesting. I mean, intellectually, the regulatory complexity is fascinating - it's like pharmacological chess. But emotionally? It's a dystopian mess. We've turned healthcare into a compliance labyrinth while people die waiting for paperwork.
What if the real problem isn't substitution - but that we treat medicine like a product and not a relationship? We don't need more rules. We need more trust. Between doctors, pharmacists, and patients. Until then, we're just rearranging deck chairs on the Titanic.