Imagine lying in a quiet room, wired up with sensors, trying to sleep while someone watches you from another room. It sounds strange, but for hundreds of thousands of people each year, this is how doctors find out why they’re exhausted, snoring loudly, or waking up gasping for air. That process is called polysomnography-a full-night sleep study that records your body’s activity while you sleep. It’s not just about checking for sleep apnea. It’s the most detailed way doctors can understand what’s really happening during your sleep.
What Exactly Is a Polysomnography Test?
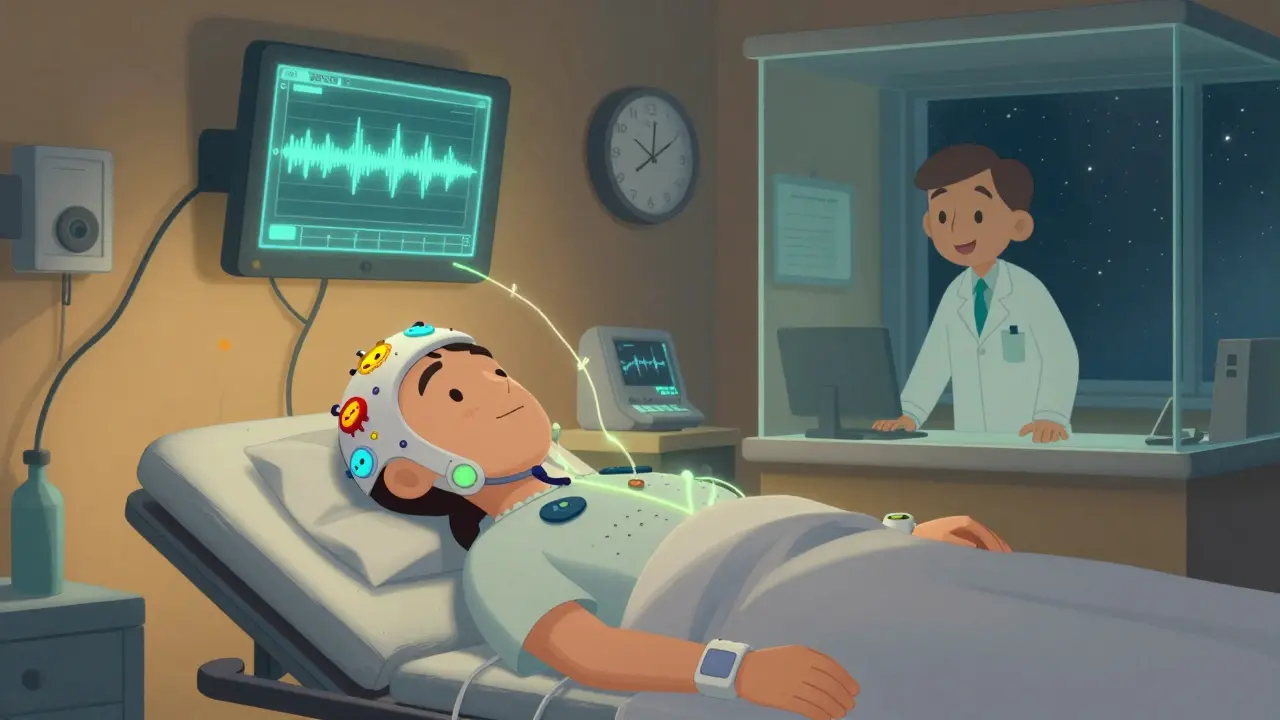
Polysomnography, often called PSG, isn’t a single test. It’s a full-body monitoring system that tracks at least seven key functions while you sleep. The name comes from Greek roots: poly (many), somno (sleep), and graphy (recording). That’s exactly what it does-records many things at once. You’ll have electrodes stuck to your scalp to measure brain waves (EEG), sensors near your eyes to track eye movement (EOG), and small patches on your chin and legs to record muscle activity (EMG). These help doctors see which sleep stage you’re in-whether you’re in deep, restorative sleep or in REM, the stage where dreams happen. Your heart rhythm is monitored with an ECG, breathing effort is measured with belts around your chest and belly, and airflow is tracked through your nose using tiny tubes. A finger clip checks your blood oxygen levels, and a camera records any unusual movements or sounds. This isn’t just a breathing test. Many people think sleep studies only check for sleep apnea. But polysomnography can uncover narcolepsy, restless legs syndrome, night terrors, sleepwalking, and even seizures that happen only at night. Without this full picture, doctors can’t tell the difference between, say, a person who stops breathing because their airway collapses (obstructive apnea) versus someone whose brain simply stops telling their body to breathe (central apnea). That distinction changes everything in treatment.How Is the Test Done? What Happens the Night of the Study?
You’ll arrive at a sleep center-usually a quiet, hotel-like room-about an hour before your normal bedtime. A trained sleep technologist will spend 30 to 45 minutes attaching all the sensors. It sounds intense, but it’s painless. No needles. No shocks. Just sticky patches and soft belts. The room is kept cool, around 21°C, to help you sleep better. You can bring your own pillow, pajamas, and even a book. Most centers let you watch TV or read until you’re ready to sleep. Once you’re settled, the technologist leaves the room but watches you live from a nearby control room. They can talk to you through an intercom if you need to use the bathroom or feel uncomfortable. You don’t have to sleep perfectly. Most people get at least a few hours of real sleep during the test. Even if you’re awake more than usual, the data is still useful. The goal isn’t to get a full eight hours-it’s to capture enough of your natural sleep patterns to spot problems. Studies show that about 85% of people get enough sleep for a clear diagnosis, even in a lab setting. Some centers now use wireless sensors. Instead of 20+ wires tangled around you, you might only have five or six small patches. That’s a big improvement from just five years ago. Still, the first few minutes feel weird. You might fidget, adjust your head, or worry you won’t fall asleep. That’s normal. Technologists hear that all the time-and they’ve got tricks to help you relax.What Does the Data Show? Understanding Your Results
After your sleep study, the raw data-over a thousand pages of numbers and waveforms-is reviewed by a board-certified sleep doctor. This isn’t automated. It takes 2 to 3 hours of careful analysis to interpret everything. The doctor looks at your sleep architecture: how long you spent in each stage of sleep. Healthy adults cycle through NREM and REM every 90 minutes. If you’re skipping REM, or entering it too early (like in narcolepsy), that shows up clearly. They also count how many times your breathing stopped or slowed. Each pause lasting 10 seconds or more is called an apnea. If you have five or more per hour, that’s considered sleep apnea. The more frequent they are, the worse the condition. Oxygen drops are another red flag. If your blood oxygen level falls below 90% during breathing pauses, it’s a sign your body is struggling. Repeated drops can strain your heart and raise your risk of high blood pressure or stroke. Leg movements, snoring volume, and body position are also analyzed. For example, if you only snore when lying on your back, a simple change in sleep position might help. If you kick your legs every 20 seconds, you might have restless legs syndrome. The final report gives you numbers: your Apnea-Hypopnea Index (AHI), your average oxygen level, how long you spent in deep sleep, and whether you had abnormal behaviors. It’s not just a yes/no answer. It’s a full sleep profile.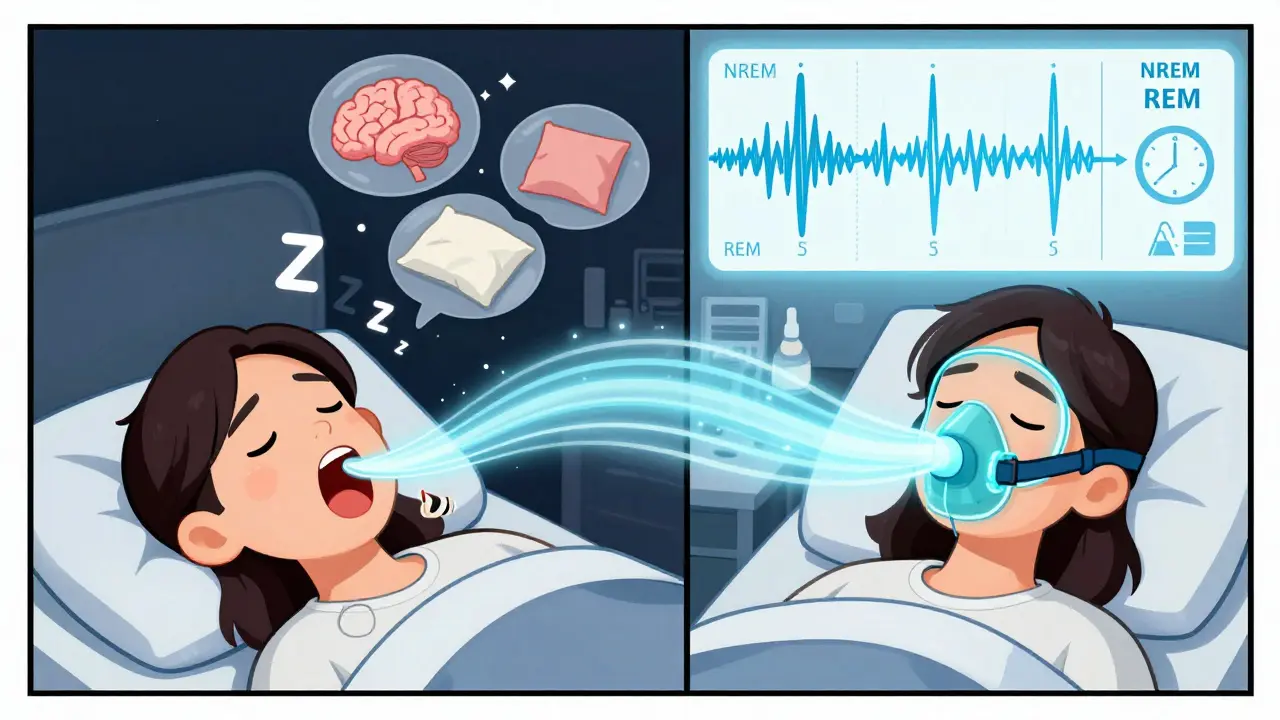
Polysomnography vs. Home Sleep Tests: Why the Difference Matters
Home sleep tests are cheaper and easier. You get a small device to wear overnight, usually measuring just airflow, oxygen, and breathing effort. But they miss a lot. They can’t tell if you’re in REM sleep. They can’t detect narcolepsy. They can’t spot sleepwalking or seizures. And they fail about 15-20% of the time because the sensors fall off or you don’t wear them right. In-lab polysomnography fails less than 5% of the time. It’s the only test that gives doctors the full picture. If you have symptoms like daytime fatigue, sudden sleep attacks, or unusual nighttime behaviors-not just snoring-your doctor should recommend a full PSG, not a home test. Insurance usually requires a polysomnography for conditions beyond simple obstructive sleep apnea. Medicare and most private insurers cover it if your symptoms match clinical guidelines: loud snoring, witnessed breathing pauses, excessive daytime sleepiness, or unexplained fatigue.What Happens After the Test?
You’ll get your results in about one to two weeks. Your doctor will sit down with you and explain what the numbers mean. If you have sleep apnea, they might suggest a CPAP machine. Sometimes, they’ll do a split-night study: the first half diagnoses apnea, and if it’s severe, they’ll start CPAP titration right then. That means you get therapy the same night-no second visit needed. If the study shows narcolepsy, you’ll likely need a second test called the Multiple Sleep Latency Test (MSLT), done the next day. That’s when you take five naps at two-hour intervals to see how fast you fall asleep and whether you enter REM too quickly. For sleepwalking or night terrors, video recordings from the study help confirm if it’s a parasomnia or something more serious like epilepsy. In those cases, you might be referred to a neurologist. The key is this: polysomnography doesn’t just give you a diagnosis. It gives you a roadmap. It tells you what’s wrong, how bad it is, and what steps to take next.Who Should Get a Polysomnography Test?
You don’t need to be a snoring, fatigued middle-aged man to qualify. Sleep disorders affect everyone. - If you’re constantly tired, even after a full night’s sleep- If your partner says you stop breathing at night
- If you wake up choking or gasping
- If you fall asleep during the day without warning
- If you have leg movements or jerking during sleep
- If you’ve been told you scream, walk, or act out dreams at night
- If you have high blood pressure, heart disease, or diabetes and can’t explain why
The American Academy of Sleep Medicine estimates over 1.5 million in-lab sleep studies are done each year in the U.S. alone-and that number is growing 8% annually. More people are waking up to the fact that poor sleep isn’t normal. It’s a medical issue.
Preparing for Your Sleep Study: Simple Tips That Make a Difference
You can’t control everything during the test, but you can control your prep. - Don’t drink coffee, tea, or soda after noon the day before. Caffeine can delay sleep and mess with your brain wave patterns.- Stick to your normal bedtime routine. Don’t try to “catch up” on sleep the night before. That skews results.
- Avoid naps the day of the test. Even a 20-minute nap can make it harder to fall asleep at night.
- Shower before you go. You can’t shower during the study, and clean skin helps sensors stick better.
- Bring comfortable clothes and anything that helps you sleep-pillow, blanket, book.
- Tell the technologist if you’re anxious. They’ve seen it before and can help you relax.
Most people are surprised by how easy it is. The wires feel odd at first, but after 10 minutes, you forget they’re there. And the peace of mind you get? Priceless.
What’s Next for Sleep Studies?
Technology is changing fast. Wireless sensors are becoming standard. AI tools now help analyze brain wave patterns faster and more accurately. Some labs are testing simplified versions of polysomnography for home use, but so far, nothing matches the accuracy of an in-lab study. The American Academy of Sleep Medicine updated its guidelines in 2020 to standardize how data is scored across clinics. That means if you get a PSG in Perth, Sydney, or New York, the interpretation will be consistent. Polysomnography won’t be replaced anytime soon. It’s still the gold standard. And for good reason: it doesn’t guess. It measures. It records. It shows you what’s really happening when you’re asleep.Is polysomnography painful?
No, polysomnography is not painful. Sensors are attached with adhesive patches and soft belts-you won’t feel any needles or electric shocks. Some people find the setup awkward or uncomfortable at first, but most adjust quickly. The goal is to make you as comfortable as possible so you can sleep naturally.
Can I use the bathroom during the study?
Yes, absolutely. If you need to use the bathroom, simply let the sleep technologist know through the intercom. They’ll disconnect the main cables temporarily so you can walk to the bathroom safely. This happens often and is completely normal.
How long does it take to get results?
It usually takes one to two weeks. The data must be reviewed by a board-certified sleep specialist, who analyzes hundreds of pages of brain waves, breathing patterns, and oxygen levels. This isn’t automated-each case requires careful human interpretation.
Will insurance cover a polysomnography test?
Most insurance plans, including Medicare, cover polysomnography if it’s ordered for a diagnosed sleep disorder with clear symptoms like snoring, witnessed apneas, or excessive daytime sleepiness. Prior authorization is often required, so check with your provider before the test.
Can a home sleep test replace a polysomnography?
Home sleep tests can screen for obstructive sleep apnea but can’t diagnose other disorders like narcolepsy, parasomnias, or central sleep apnea. They also have a higher failure rate. If you have complex symptoms, a full in-lab polysomnography is the only reliable option.
What if I can’t sleep during the study?
You don’t need a full eight hours. Even a few hours of sleep can provide enough data for diagnosis. Most people sleep enough to get accurate results. Sleep technologists are trained to help you relax and will adjust sensors if needed. Many patients say they slept better than expected.




15 Comments
This is why America's healthcare is broken. They charge you $2000 to watch you sleep? I could've just watched my dog sleep and got the same data. Wake up people, this is just corporate greed in a lab coat.
They're not just watching you sleep. They're recording your brainwaves. Do you know what that means? They're mapping your dreams. And who's to say they're not selling that data to the government? You think the CIA doesn't want to know when you're dreaming about your ex? This isn't medicine. It's surveillance.
So let me get this straight. You pay a fortune to lie in a room wired like a sci-fi experiment so some tech can watch you struggle to sleep? And you call this a 'diagnostic tool'? My cat sleeps better than this.
We think of sleep as a passive state, but it's the most active phase of our existence. The body repairs, the mind processes, the soul... I don't know if souls have EEG patterns, but I'd bet they do. This test doesn't just measure sleep-it measures the invisible architecture of being human.
It's not about the wires. It's about the data. If you're tired all day, this tells you why.
I went through this last year. Thought I'd hate it. Ended up sleeping better than I had in years. The room was nice, the tech was chill. It's not perfect, but it's the best tool we've got.
You Americans pay to get watched while sleeping? In India, we just drink turmeric milk and pray. If you're tired, it's your karma. No machines needed. This is what happens when you outsource your biology to corporations with clipboards.
I appreciate the thoroughness of this explanation. The clinical precision and attention to detail reflect the high standards of sleep medicine in the United States. It is commendable how such a complex physiological process is systematically evaluated with such care.
I had this done and honestly the hardest part was not being able to check my phone... I kept thinking about my inbox... and the sensors kept falling off... I mean like why do they put them on your legs? I just kept adjusting... and the tech kept coming back... I swear I didn't move that much...
The AHI threshold of 5 is outdated. Current literature supports 15 as the diagnostic cutoff for moderate OSA. You're misdiagnosing 40% of patients with this metric. And why are they still using analog EMG? The industry is stuck in 2008. The AI algorithms are ready-why are you still relying on human scorers with coffee-stained reports?
I did this last year and it changed my life. I had no idea I was stopping breathing 40 times an hour. Got my CPAP and now I feel like a new person. If you're tired all the time, just do it. No excuses. Your future self will thank you.
I used to think sleep studies were for old people. Then I started waking up at 3 a.m. gasping. Did the test. Turns out I had mild apnea. CPAP was awkward at first, but now I sleep like a baby. Don't ignore it. Your heart will thank you.
I can't believe people actually PAY for this! I mean, seriously? You're telling me you can't just... I don't know... sleep better? Or stop eating cheese before bed? Or go to bed earlier? Why do we need 20 wires and a camera? This is just another way to make money off of people who are too lazy to fix their own lives!
I'm a sleep tech. I've seen hundreds of these. The biggest myth? 'I can't sleep in a lab.' Most people sleep fine. Even if you're awake 30% of the night, we still get the data. Don't stress. Bring your pillow. Watch a show. You'll be fine. 💤
The clinical utility of polysomnography remains unparalleled in the differential diagnosis of sleep-wake disorders. While technological advancements continue to evolve, the gold standard remains anchored in the comprehensive, multi-parametric assessment of nocturnal physiology under controlled conditions. This methodology ensures diagnostic accuracy, which is paramount in the management of chronic conditions such as obstructive sleep apnea and narcolepsy.