Hydrea Uses, Side Effects, and Real Patient Experiences
Clear answers about Hydrea—what it is, why doctors use it, what to expect, and critical patient tips for dealing with side effects or therapy changes.
If you’ve heard the name hydroxyurea and wonder what it actually does, you’re not alone. This drug shows up a lot when people talk about sickle‑cell disease or certain blood cancers. Below we break down why doctors prescribe it, how to take it safely, and what side effects you might see.
Hydroxyurea belongs to a class called antimetabolites. In plain terms, it slows down the growth of abnormal cells in the bone marrow. For sickle‑cell patients, this slowdown means fewer sickled red blood cells and less painful crises. For cancers like chronic myeloid leukemia or some types of melanoma, it helps keep tumor cells from multiplying.
The drug also boosts a molecule called fetal hemoglobin. More fetal hemoglobin makes red blood cells more flexible, which is why people with sickle‑cell disease often feel better on hydroxyurea. The effect isn’t instant—you usually need a few weeks of regular dosing before you notice fewer pain episodes.
Like any medication, hydroxyurea can cause side effects. The most common ones are low blood counts, which show up as fatigue or easy bruising. Your doctor will order blood tests every few weeks to make sure numbers stay in a safe range.
Other possible issues include nausea, mild skin rash, and occasional hair thinning. If you get a fever or notice unusual bleeding, call your healthcare provider right away—these could signal a more serious drop in white cells or platelets.
Staying hydrated, eating balanced meals, and avoiding alcohol can help reduce some of the discomfort. Many patients find that taking the pill with food eases stomach upset.
Remember, you don’t have to stop the medication on your own if side effects appear. Your doctor can adjust the dose or suggest supportive treatments to keep you on track.
Hydroxyurea is usually taken once a day as a capsule, but dosing varies based on weight, disease severity, and lab results. Never skip doses without checking with your provider; missing days can cause blood counts to swing unpredictably.
When starting hydroxyurea, keep a simple log of how you feel each week—note any pain episodes, energy levels, or new symptoms. This record helps the doctor fine‑tune the dose quickly.
If you’re pregnant or planning to become pregnant, discuss alternatives with your physician. Hydroxyurea can affect fetal development, so it’s typically avoided during pregnancy unless benefits clearly outweigh risks.
Overall, hydroxyurea offers a real quality‑of‑life boost for many patients when used correctly. The key is regular monitoring, open communication with your healthcare team, and staying informed about what to expect.
Got more questions? Talk to your doctor or pharmacist—they can explain the exact dose you need, how often labs should be done, and any lifestyle tweaks that help you stay comfortable while on hydroxyurea.
Clear answers about Hydrea—what it is, why doctors use it, what to expect, and critical patient tips for dealing with side effects or therapy changes.

Discover how to safely buy cheap generic Lamictal (lamotrigine) online, compare prices, avoid scams, and understand dosage, side effects, and pharmacy credentials.
Learn how to safely buy cheap generic tetracycline online, check pharmacy legitimacy, understand dosage, side effects, and avoid scams.
Dealing with a decrease in sexual desire in a relationship can be challenging. It's important to communicate openly with your partner about your feelings and concerns. Try introducing new elements into your intimate moments to reignite the passion and excitement. Seek professional help, like a sex therapist, if necessary. Also, maintaining a healthy lifestyle can greatly impact your libido.

Team-based care improves generic prescribing by combining doctors, pharmacists, and nurses to reduce costs, prevent errors, and boost medication adherence. Learn how this model works and why it’s changing patient outcomes.
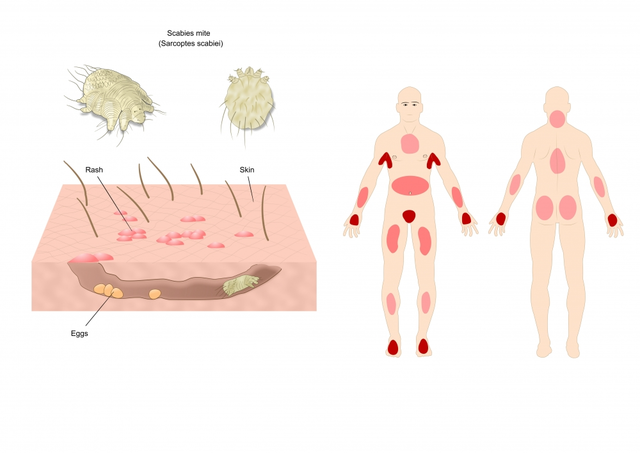
In my recent research, I've discovered a fascinating connection between Sarcoptes scabiei, the microscopic mite responsible for scabies, and other skin conditions. It turns out that the presence of these mites can exacerbate existing skin conditions like eczema and psoriasis, leading to a more severe manifestation of symptoms. Furthermore, the intense itching caused by scabies can result in secondary bacterial infections if not treated promptly. It's crucial to consult a doctor if you suspect a scabies infestation, as early treatment can prevent complications and alleviate discomfort. Don't hesitate to reach out to a healthcare professional if you're experiencing persistent skin issues; it might just be the key to finding relief.
