More than 40% of adults in the U.S. take at least one medication that can react dangerously with alcohol. That’s not a small risk-it’s a silent danger hiding in plain sight. You might think having a glass of wine with your pills is harmless, especially if you’ve done it before without issue. But the truth is, even one drink can turn a safe medication into a serious threat. This isn’t about scare tactics. It’s about facts, timing, and knowing exactly what’s happening inside your body when alcohol meets your medicine.
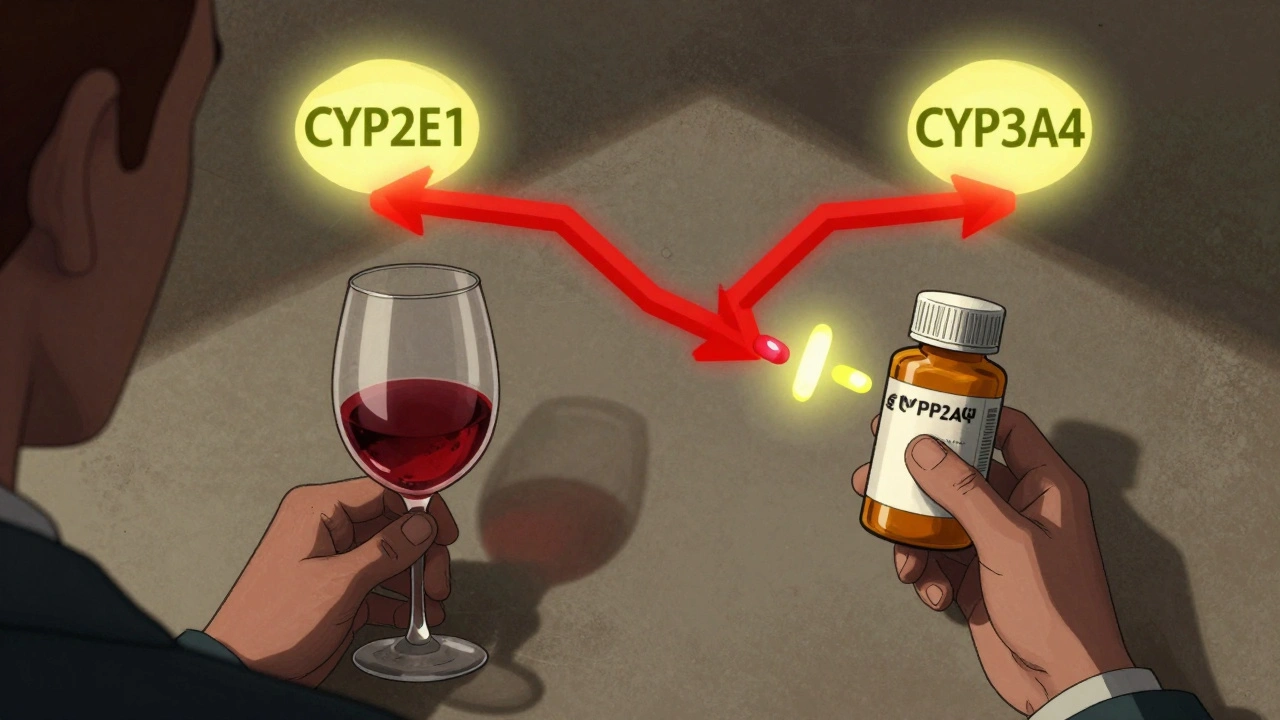
How Alcohol Changes How Your Medication Works
Alcohol doesn’t just make you feel drunk. It changes how your liver processes medications. Your liver uses enzymes-mainly CYP2E1, CYP3A4, and CYP1A2-to break down both alcohol and most prescription drugs. When you drink, these enzymes get busy with alcohol first. That means your medication doesn’t get broken down as fast. It builds up in your bloodstream, sometimes to dangerous levels.For example, if you take diazepam (Valium) and have even one beer, the drug’s half-life can stretch from 20-100 hours to 35-150 hours. That means it stays in your system way longer than expected. You might feel dizzy, sleepy, or confused hours after you thought the effects had worn off. In extreme cases, this can lead to slowed breathing or even respiratory failure.
On the flip side, if you drink alcohol regularly over weeks or months, your liver starts making more of these enzymes. That speeds up how fast your body breaks down the medication. Suddenly, your antidepressant or blood pressure pill doesn’t work as well. You might think your treatment has stopped working-when really, it’s the alcohol doing the damage.
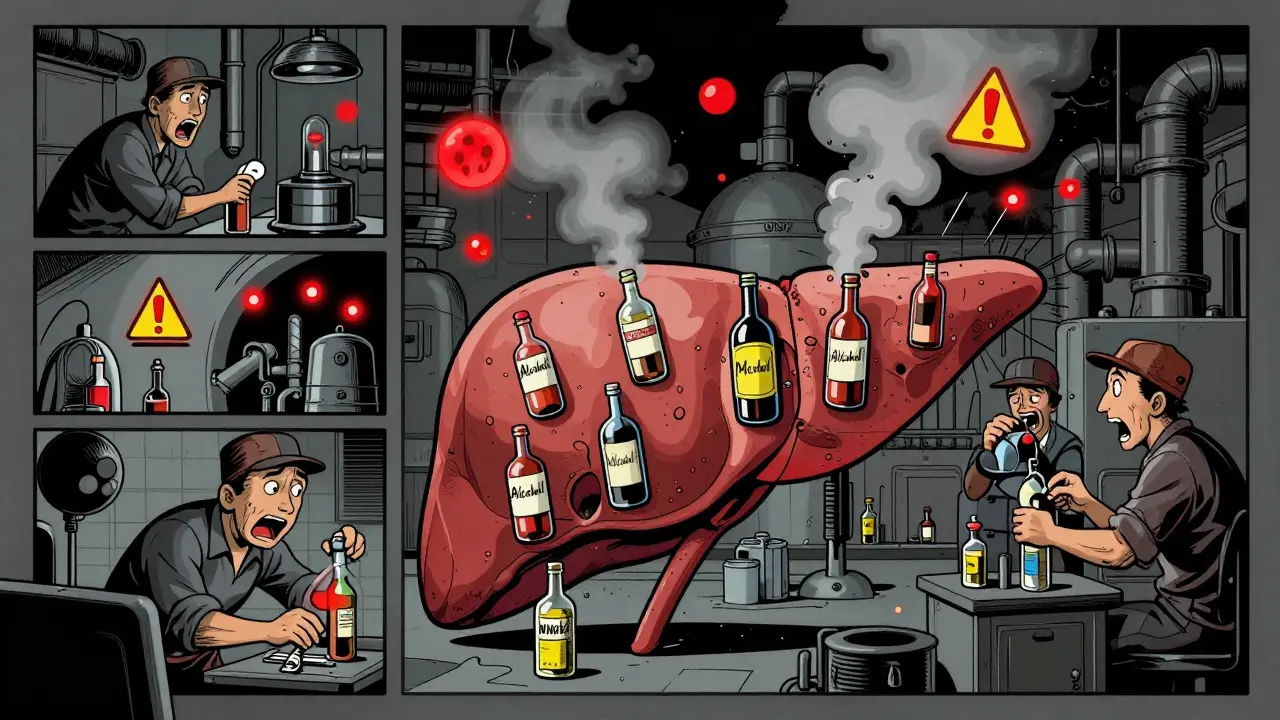
High-Risk Medications You Should Avoid With Alcohol
Some medications are simply not safe with any amount of alcohol. These aren’t just warnings-they’re red flags backed by hospital data.- Metronidazole (Flagyl): One drink can trigger a reaction called disulfiram-like syndrome. You’ll feel flushing, nausea, vomiting, a racing heart, and possibly chest pain. In 92% of cases, this happens even with just one standard drink. ER visits from this combo are common.
- Benzodiazepines (alprazolam, lorazepam, clonazepam): These are sedatives. Alcohol is a sedative. Together, they multiply their effects. Studies show GABA receptor activity increases by 400%, leading to extreme drowsiness, loss of coordination, and stopped breathing at blood alcohol levels as low as 0.05%-that’s less than one drink for most people.
- Opioids (oxycodone, hydrocodone, morphine): Alcohol makes opioids 8 times more likely to cause fatal respiratory depression. The CDC calls this one of the deadliest combinations.
- Antidepressants (SSRIs like fluoxetine, sertraline): While not always deadly, alcohol can make depression worse, increase dizziness, and extend how long you feel drunk. One study found it adds over 3 hours to intoxication time.
- Antihistamines (diphenhydramine, hydroxyzine): Found in sleep aids and allergy meds, these already make you sleepy. Add alcohol, and that sleepiness becomes dangerous. You might fall asleep while driving or not wake up if you stop breathing.
- Acetaminophen (Tylenol): Even moderate drinking (2-3 drinks a day) with daily acetaminophen use increases liver damage risk by 18%. The liver can’t handle both at once. In 2023, liver failure from this combo was reported in 18% of cases among regular drinkers.
- NSAIDs (ibuprofen, naproxen): These already irritate your stomach lining. Alcohol does too. Together, they can cause bleeding ulcers. Risk goes up 300-500% with regular use.
What About Over-the-Counter Drugs?
Many people don’t realize that OTC meds can be just as risky. A cold medicine with diphenhydramine? A sleep aid with melatonin and alcohol? A pain reliever with ibuprofen after a few beers? These are all common choices-and all dangerous.The FDA’s Adverse Event Reporting System shows over 12,000 cases in the last five years where OTC meds mixed with alcohol led to emergency room visits. Most involved sleep aids, pain relievers, or allergy meds. The problem? Labels rarely warn you clearly. Only 42% of prescription bottles have alcohol interaction warnings-and even fewer OTC labels do.
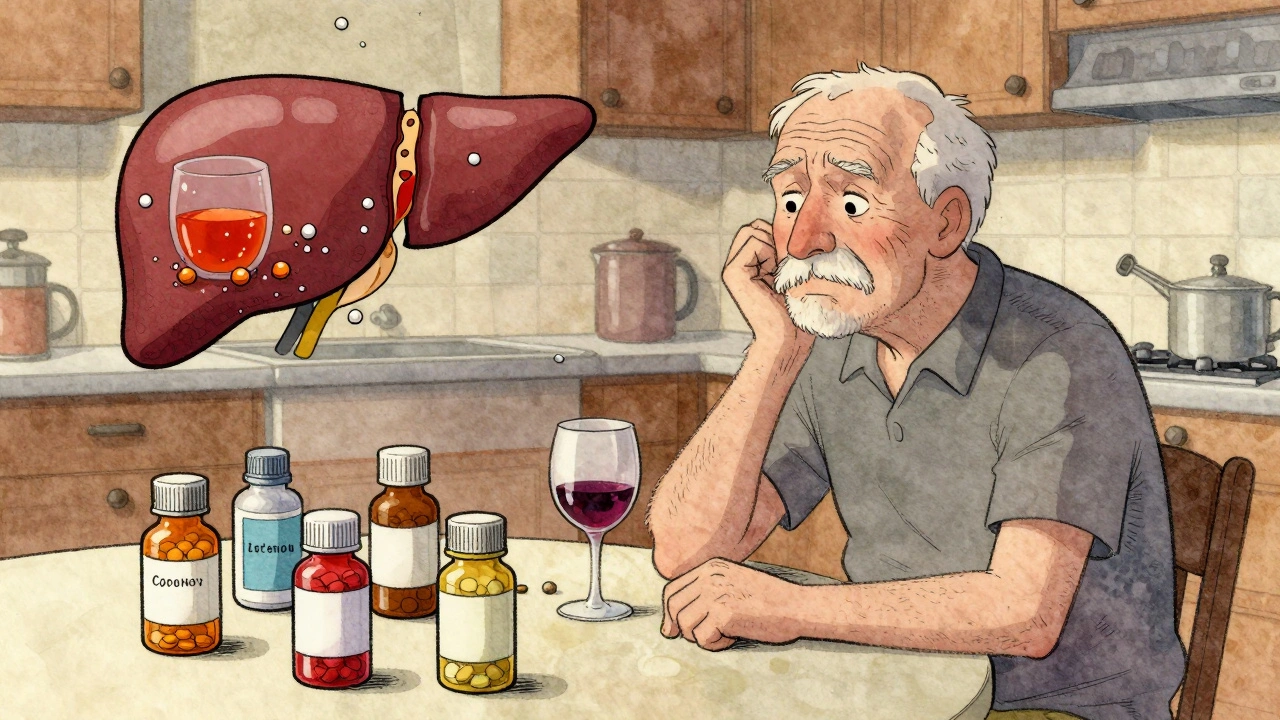
Why Older Adults Are at Higher Risk
If you’re over 65, your body handles alcohol and medicine differently. Liver blood flow drops by about 35% between ages 25 and 75. That means your liver processes both substances slower. Medications stick around longer. Alcohol hits harder.The American Geriatrics Society’s 2023 Beers Criteria lists 17 medications that are especially risky for seniors when combined with alcohol. These include sleep aids, muscle relaxants, and certain blood pressure drugs. Seniors are also more likely to take five or more medications at once. That’s called polypharmacy-and it multiplies the chances of a bad interaction.
And here’s the kicker: 50% more seniors who drink and take meds end up hospitalized than those who don’t. Yet only 28% of Medicare Annual Wellness Visits even ask about alcohol use.
What You Can Do: Practical Safety Steps
You don’t have to give up alcohol entirely-but you do need to be smart.- Know your meds. Check the label. Look for words like “avoid alcohol,” “may cause drowsiness,” or “do not drink.” If it’s not clear, ask your pharmacist.
- Wait 72 hours. For high-risk drugs like metronidazole, stop drinking at least three days before starting. This cuts your reaction risk from 92% to just 8%.
- Wait 2-3 hours after taking your pill. If you’re on a medication that’s not strictly forbidden, wait at least that long after taking it before drinking. That gives your body time to absorb and start processing the drug.
- Drink with food. Eating slows alcohol absorption by 25-30%. It won’t make it safe, but it reduces how fast it hits your system.
- Stick to one drink. For women: one standard drink (12 oz beer, 5 oz wine, 1.5 oz spirits). For men: two. More than that? The risks jump fast.
- Know your limits. A standard drink is not a pint of beer or a large glass of wine. Measure it. Use a shot glass for spirits. Pour wine into a measuring cup once to see what 5 oz looks like.
What No One Tells You About Warning Labels
You might assume your doctor or pharmacist warned you. But here’s the truth: 68% of patients say they were never told about alcohol risks. That’s not because providers are careless. It’s because the system doesn’t make it easy.Prescription labels are cluttered. Medication guides are written in medical jargon. Only 48% of patients understand what they read. Visual tools help. The Injury Matters Foundation’s color-coded chart-red for avoid, yellow for caution, green for safe-boosted patient understanding from 48% to 82% in clinical tests.
Pharmacists are your best ally. Walgreens data shows 89% of patients who got alcohol interaction counseling from a pharmacist changed their habits. That’s more than any doctor’s note or website article.
Real Stories, Real Consequences
On Reddit, one user wrote: “Took one beer with my metronidazole and ended up in the ER with vomiting and a heart rate of 180.” Another said: “My pharmacist warned me about mixing hydroxyzine with wine. Saved me from a disaster at my sister’s wedding.”These aren’t rare. Drugs.com has over 78,000 user reports of bad reactions. The top three? Alprazolam, amitriptyline, and warfarin. Warfarin is especially tricky-alcohol can make it too strong (risk of bleeding) or too weak (risk of clots), depending on how much you drink and when.
What’s Changing in 2025
New rules are starting to take effect. As of January 2024, the FDA requires high-risk medications to include pictograms on labels showing alcohol interaction risks. Telehealth platforms now screen for alcohol use before prescribing. Medicare Part D plans must flag risky combinations in their systems by December 2024.And new tools are emerging. The NIAAA’s Alcohol-Medication Interaction Risk Calculator (AMIRC) lets you plug in your meds, drinking habits, age, and liver health to get a personalized risk score. Stanford’s EHR-integrated warning system cut unsafe combinations by 37% in just six months.
Final Thought: It’s Not About Perfection-It’s About Awareness
You don’t have to be perfect. But you do have to be informed. If you take any medication-even one you’ve been on for years-ask: Is alcohol safe with this? Don’t assume. Don’t guess. Ask your pharmacist. Check the label. Use a trusted tool like the NIAAA’s AMIRC or GoodRx’s interaction checker.Alcohol isn’t the enemy. But when it teams up with your medicine, it becomes a silent partner in risk. Knowing the facts gives you control. And control saves lives.






13 Comments
So let me get this right: I can’t have a glass of wine with my Zoloft… but I can have three glasses while scrolling through TikTok at 2 a.m.? 🤔
Knowledge is power. And power, when used wisely, saves lives. Let us all be mindful stewards of our health, and extend compassion to those who are learning.
You people are lazy. If you can't read a label you deserve to die
Y’all act like alcohol is the devil but i’ve been drinkin’ and takin’ ibuprofen since 2012 and still standin’! 🇺🇸
The real issue is not alcohol. It’s the systemic failure of pharmaceutical oversight and the commodification of patient care. You’re being manipulated.
Guys I just used the NIAAA calculator and it said I’m low risk! 🙌 I’m gonna have one beer with my metronidazole just to test it out 😅
Wait so you’re telling me I can’t have a beer after my Vicodin? Bro I’ve been doing this since college. You’re just scared of fun.
Did you know the government hides the truth about alcohol-med interactions because Big Pharma owns the FDA? 🚨 I saw a video where a whistleblower said they bury 90% of adverse events. 🤫💊 #CoverUp
It is imperative that patients engage in proactive dialogue with their pharmacists. The data demonstrates unequivocally that pharmacist-led counseling results in statistically significant behavioral change. I encourage all readers to schedule a medication review.
Man, I used to think having a glass of wine with my blood pressure med was fine-until my buddy got rushed to the ER after mixing Ambien and whiskey. Talk about a wake-up call. I’ve been sober for 14 months now, and honestly? I sleep better, think clearer, and my anxiety? Gone. Not because I’m perfect, but because I finally listened. You don’t have to quit everything overnight. Just start with one question: ‘Is this really worth it?’
Let’s be honest-this isn’t about education. It’s about control. The medical establishment wants you to fear alcohol because they profit from your dependence on pharmaceuticals. If you stopped drinking, you’d need fewer meds. And that’s not profitable. They’ll scare you with ER stats and half-lives, but they won’t tell you that alcohol reduces inflammation, improves insulin sensitivity, and helps with social bonding. The real danger is blind obedience to authority. Question everything.
I just lost my dad to a liver bleed from Tylenol and wine. I didn’t know it was dangerous. I wish someone had told me. Please, if you’re reading this-ask. Even if it feels silly. I wish I had.
Ask your pharmacist. Seriously. They’re the unsung heroes. And yes, you can still have a drink-just not with your metronidazole. 🙏