When your child’s asthma inhaler suddenly looks different - maybe it’s a different color, size, or even tastes a little off - it’s easy to assume it’s the same medicine. But in many cases, it’s not. Insurance companies and pharmacies are switching brand-name medications for cheaper generic versions more often than ever, and pediatric medication switches are happening without enough warning, education, or safety checks for kids.
This isn’t just about saving money. For children, especially those with chronic conditions like asthma, epilepsy, or heart disease, even small changes in medication can lead to serious health risks. The FDA says generics are "bioequivalent" to brand-name drugs, meaning they contain the same active ingredient and work the same way in adults. But children aren’t small adults. Their bodies process drugs differently, and the rules made for grown-ups don’t always fit them.
Why Generic Switches Are Riskier for Kids
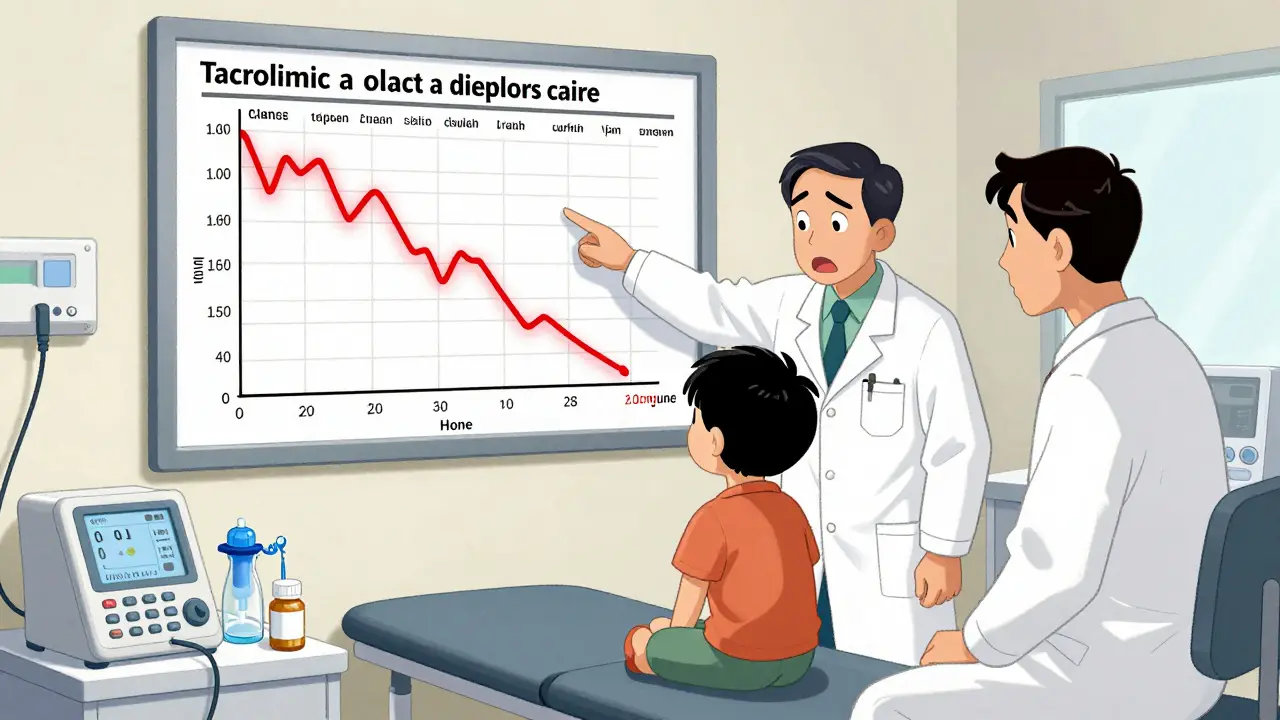
Generic drugs must be 80% to 125% as effective as the brand-name version in terms of how much medicine enters the bloodstream. That’s a wide range - and for some medications, it’s dangerous. Drugs like phenytoin (for seizures), tacrolimus (for transplant patients), and warfarin (a blood thinner) have a narrow therapeutic index. That means the difference between a dose that works and one that causes harm is tiny. A 14% drop in blood levels after switching to generic tacrolimus, as seen in a 2015 study of pediatric heart transplant patients, can increase the risk of organ rejection.
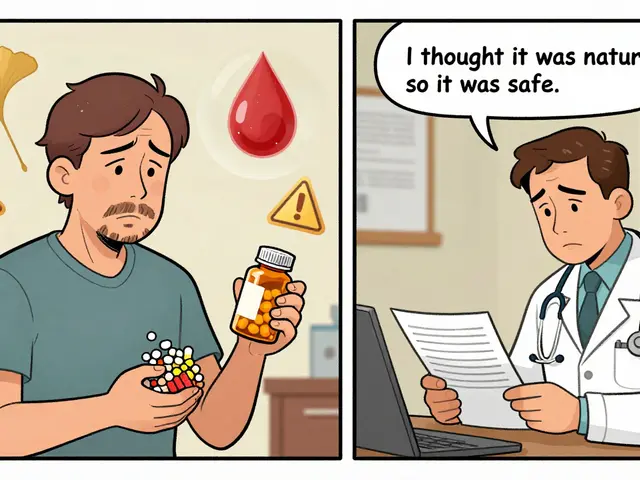
Even when the active ingredient is identical, the inactive ingredients - the fillers, dyes, flavors, and binders - can vary between brands. These don’t treat the disease, but they can affect how the drug is absorbed. In rare cases, a child might react to a new dye or flavoring in a generic version. One parent reported her toddler developed a rash after switching from brand-name omeprazole to a generic version for reflux. The doctor didn’t connect it until she mentioned the change.
Developmental Differences Matter
Children’s bodies change fast. A 3-month-old baby metabolizes drugs differently than a 5-year-old or a teenager. For example, the liver enzyme CYP2C19, which breaks down omeprazole, isn’t fully developed in infants under 6 months. A generic version that works perfectly in an adult might not work at all in a baby - even if it’s labeled the same. The FDA admits it doesn’t have enough data on how generics behave in kids under 2. Yet, insurers still switch prescriptions without checking.
Medications for asthma, ADHD, and seizures are often given in liquid form or through inhalers. When a generic version uses a different device - say, a different spacer or nebulizer cup - the child might not get the full dose. Studies show technique errors can cut drug delivery by 50% to 80%. If a child’s inhaler changes from a blue canister to a green one, and the family doesn’t realize the technique needs adjusting, the child could be under-treated.
Switches Hurt Adherence
Parents don’t always know they’re being switched. Pharmacists aren’t required to tell them in most states. In 19 states, pharmacists must substitute generics automatically. In only 7 states and Washington, D.C., do they need the parent’s consent. That means a parent might walk into the pharmacy for their child’s daily asthma medication and walk out with something completely different - no explanation, no warning.
When that happens, confusion follows. One mother told her pediatrician her 7-year-old’s asthma was getting worse. She didn’t realize the inhaler had changed. The new one had a different mouthpiece, a different color, and a different instruction sheet. Her son stopped using it because he didn’t trust it. Adherence drops by 15% to 20% after a switch, according to research from Children’s Hospital of Philadelphia. That’s not just about forgetfulness - it’s about fear, confusion, and lack of trust.
What Medications Are Most Risky to Switch?
The FDA and the American Academy of Pediatrics list specific drug classes where switching should be handled with extreme caution:
- AEDs (anti-epileptic drugs) - Phenytoin, valproate, carbamazepine. Small changes can trigger seizures.
- Immunosuppressants - Tacrolimus, cyclosporine. Used after organ transplants. Even slight drops in blood levels can lead to rejection.
- Psychiatric medications - SSRIs, stimulants like methylphenidate. Mood and behavior can shift unexpectedly.
- Cardiac drugs - Digoxin, amiodarone. Heart rhythm is sensitive to tiny changes.
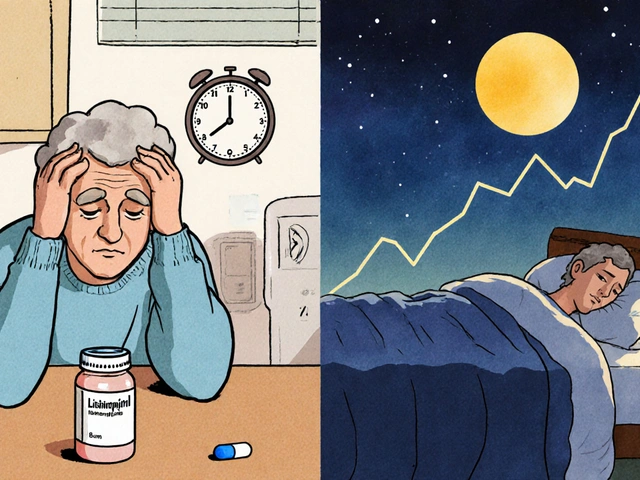
- Thyroid medications - Levothyroxine. A 10% change in absorption can cause fatigue, weight gain, or developmental delays in children.
Even common drugs like omeprazole (for reflux) or albuterol (for asthma) can cause problems when switched in infants or toddlers. If your child is on one of these, ask: "Was this switched? Is it safe?"
What Parents Can Do
You don’t have to accept a switch without a fight. Here’s what to do:
- Ask before the switch. When your child’s prescription is refilled, call the pharmacy and ask: "Is this the same brand? If not, why was it changed?"
- Check the label. Look at the name on the bottle. If it says "generic" or a different manufacturer (like Teva, Mylan, or Sandoz), it’s not the brand you know.
- Request a brand if needed. Your doctor can write "Dispense as Written" or "Do Not Substitute" on the prescription. This legally blocks automatic switching in most states.
- Watch for changes. Is your child acting differently? Is their symptom control worse? Did they start vomiting, having rashes, or refusing the medicine? These could be signs of a bad switch.
- Document everything. Keep a log: date of switch, what changed, symptoms before and after. This helps your doctor spot patterns.
Some insurers will cover the brand-name drug if you prove the generic isn’t working. Your doctor can write a letter of medical necessity. Don’t assume it’s too much work - it’s worth it.

What Providers and Pharmacies Should Do
Good doctors and pharmacists don’t just fill prescriptions - they protect kids. The American Academy of Pediatrics says pharmacists should:
- Notify caregivers before switching any chronic medication.
- Teach families how to use new devices (inhalers, nebulizers, droppers).
- Keep a list of children on high-risk medications and flag any switches.
- Coordinate with the prescribing doctor before changing anything.
Yet, a 2018 survey found only 37% of pharmacists routinely discussed switching risks with parents of kids on long-term meds. That’s not enough. If your pharmacist doesn’t offer this, ask for it. If they refuse, find one who will.
The Bigger Picture: Why This Keeps Happening
Insurance companies save billions by switching to generics. Between 2009 and 2019, generics saved the U.S. healthcare system $2.2 trillion. But those savings often come at the cost of children’s health. One insurer might switch a child’s asthma medication to save $10 a month - then switch again six months later when the deal expires. That’s called "formulary churn," and it’s common. Kids end up on three different inhalers in a year.
Regulators are starting to notice. California passed a law in 2022 requiring Medicaid plans to have pediatric review committees before changing medications for kids. The FDA has launched the Pediatric Formulation Initiative to improve child-friendly dosing. But until the FDA requires pediatric-specific bioequivalence testing - especially for drugs with narrow therapeutic windows - the risks will remain.
What’s Coming Next
The American Academy of Pediatrics is finalizing new guidelines for generic prescribing in children, expected in late 2024. These will give doctors clear rules on when to allow switches and when to push back. More states are likely to follow California’s lead and require consent or notification.
For now, the burden falls on parents. You know your child best. If something feels off after a switch, speak up. Don’t assume the doctor or pharmacist has your child’s best interest in mind - because too often, they’re working under rules designed for adults, not kids.
Medication isn’t just chemistry. It’s trust. It’s routine. It’s a child’s ability to breathe, learn, play, and grow. Don’t let a cheaper pill compromise that.











10 Comments
Just had this happen with my 4-year-old’s albuterol inhaler 🤯 Switched to generic and she started coughing worse at night. Took me 3 weeks to connect the dots. Finally called the pharmacy - they said it was "standard practice." No warning. No explanation. I demanded the brand back. Worth every call. Don’t let them gaslight you. Your kid’s breathing is not a budget line item.
This is so important. I’m a pediatric nurse and I see this every week. Parents come in panicked because their child’s seizure pattern changed - and it was a generic switch they didn’t even know about. The system is broken. Doctors are overloaded, pharmacists are undertrained on pediatrics, and insurers don’t care as long as the numbers look good. We need mandatory parent notification. Period.
While the concerns raised are valid, it is critical to acknowledge that bioequivalence standards are rigorously tested and approved by the FDA. The claim that children are "not small adults" is accurate, yet the data on pediatric pharmacokinetics for generics is expanding. The issue is not the science - it’s the implementation. A systemic overhaul in communication protocols, not a rejection of generics, is the appropriate path forward.
My son’s levothyroxine got switched last year. He went from thriving to lethargic, gaining weight, zoning out in school. I didn’t think to question it until his teacher asked if he was okay. We switched back - and boom, he was himself again. I didn’t know you could legally demand the brand name. I’m telling everyone now. If your kid’s on meds that affect mood, energy, or development - don’t just accept the change. Ask. Push. Document. You’re their advocate.
my kid’s inhaler changed color and he refused to use it for two weeks. i thought he was being stubborn. turns out he was scared. we had to reteach him how to use it. no one told us it was different. just... changed. it’s not just about medicine. it’s about trust.
My daughter’s seizure meds switched to generic and she had three breakthrough seizures in a week. The pharmacy didn’t say a word. The doctor didn’t ask. We were lucky we caught it. Now I keep a printed list of every med she’s on - brand name, manufacturer, dose - taped to the fridge. If you’re on a high-risk med, treat the prescription like a security clearance. Don’t let anyone touch it without your say-so.
The FDA’s bioequivalence range of 80–125% is scientifically indefensible for narrow-therapeutic-index drugs in pediatric populations. The current regulatory framework is rooted in adult pharmacokinetic models and fails to account for developmental pharmacology. Until the FDA mandates pediatric-specific bioequivalence thresholds - particularly for antiepileptics, immunosuppressants, and cardiac agents - these switches constitute a de facto clinical experiment on vulnerable populations. Legislative action is overdue.
It’s funny how we trust a pill to fix a broken bone but hesitate to trust it when it’s changing the rhythm of a child’s heart. Medicine isn’t just chemistry - it’s ritual. It’s the same bottle, the same time, the same voice saying "here, sweetie, take this." When that changes, even if the active ingredient is the same, the child feels it. The system forgets that healing isn’t just about molecules - it’s about consistency, safety, and the quiet trust between a parent and their child’s medicine.
you think this is bad wait till you see what happens in india where generics are the only option and no one cares about kids. you americans think you have problems. we have 100% generic everything and still kids get better. stop being so dramatic. if your kid is not responding maybe you are a bad parent not the medicine
THIS IS WHY WE NEED TO STOP LETTING INSURANCE COMPANIES CONTROL MEDICAL DECISIONS!! THEY’RE NOT DOCTORS!! THEY’RE CORPORATE PROFITEERS!! THEY SWITCH MEDS TO SAVE $10 A MONTH WHILE KIDS SUFFER!! THIS ISN’T "SAVING MONEY" - IT’S CHILD NEGLECT BY ALGORITHM!! I’M CALLING MY REP TODAY AND DEMANDING A FEDERAL LAW THAT BANS GENERIC SWITCHES FOR KIDS WITHOUT PARENTAL CONSENT!! #STOPGENERICGAMBLING