When your nose won’t stop running, your eyes itch, and you feel like you’re constantly sneezing - it’s not just a cold. It’s allergic rhinitis. And if you’re dealing with this year after year, you’re not alone. In the U.S., nearly 20 million adults and 7 million kids have been diagnosed with hay fever, according to the American College of Allergy, Asthma & Immunology. But here’s the thing: most people treat it wrong. They grab an antihistamine from the drugstore, hope it works, and give up when it doesn’t. That’s because allergic rhinitis isn’t one-size-fits-all. Seasonal allergies and year-round allergies need different strategies - and knowing the difference can change everything.
Seasonal vs. Perennial: Know Your Trigger
Not all allergic rhinitis is the same. Seasonal allergic rhinitis flares up during specific times of the year - usually spring, summer, or early fall - when pollen counts spike. Tree pollen hits in March and April, grass pollen peaks in May and June, and ragweed takes over in late summer. If you start sneezing every April and feel better by October, you’re likely dealing with seasonal triggers.
Perennial allergic rhinitis, on the other hand, sticks around all year. You don’t need sunshine to feel it. Dust mites hiding in your mattress, pet dander clinging to your couch, mold growing in your bathroom, or even cockroach droppings in your kitchen can keep your nose running in December. These allergens are always there, so your symptoms never really go away.
The difference matters because your treatment should match your trigger. A medicine that works for pollen might do nothing for dust mites. And if you’re treating seasonal allergies like they’re perennial, you’re wasting time and money.
The Gold Standard: Intranasal Corticosteroids
If you’ve got moderate to severe symptoms - think blocked nose, trouble sleeping, constant fatigue - the most effective treatment isn’t the antihistamine you see on TV. It’s an intranasal corticosteroid. These sprays, like fluticasone (Flonase), mometasone (Nasonex), or budesonide (Rhinocort), work by calming inflammation deep in your nasal passages. They’re not decongestants. They don’t give you instant relief. But over a few days, they reduce swelling, stop runny noses, and ease congestion better than anything else.
Studies show they’re 30-50% more effective than oral antihistamines for nasal blockage. One trial with over 800 patients found mometasone reduced symptoms by 27% more than placebo. And unlike decongestant sprays, you can use them long-term without risking rebound congestion.
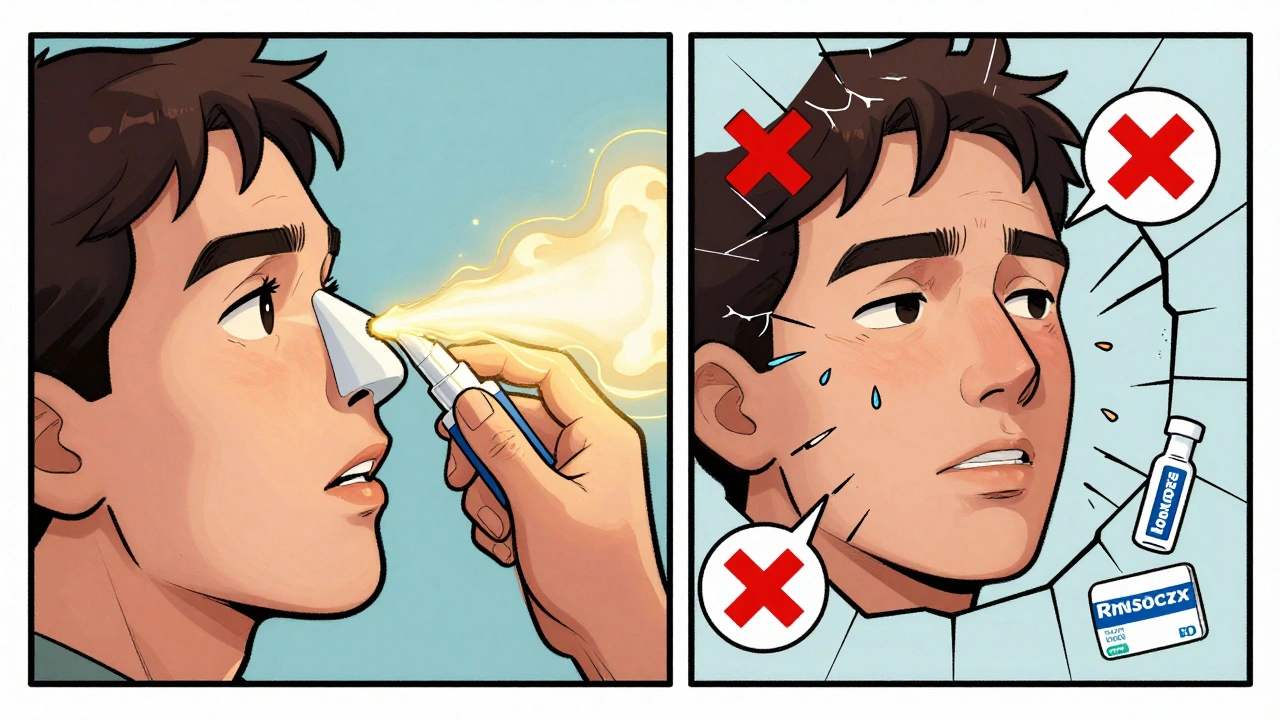
But here’s the catch: you have to use them every day. Not just when you feel bad. Not just during pollen season. Daily use builds up their effect. If you skip a few days, you lose the benefit. And most people don’t use them right. A study found 60-70% of users point the spray straight back into their septum - the wall between their nostrils. That doesn’t help. It can even cause nosebleeds.
Proper technique? Aim the spray toward your ear, not your brain. Tilt your head slightly forward. Breathe in gently as you spray. Don’t sniff hard. Wait 15 minutes before blowing your nose. Do this right, and you’ll get the full effect. Do it wrong, and you’re wasting a $40 prescription.
Oral Antihistamines: Fast, But Limited
Antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) are the go-to for many because they’re easy. No spray. No technique. Just swallow a pill. And they work fast - usually within an hour. They’re great for sneezing, itching, and runny nose. But they don’t touch congestion. That’s the big gap.
Second-generation antihistamines (the ones listed above) are preferred because they cause less drowsiness than older versions like diphenhydramine (Benadryl). Still, about 5-10% of users feel a little sleepy. That’s far better than the 15-30% with first-gen drugs, but it’s not zero.
If your main problem is itching eyes and sneezing fits - especially during pollen season - these are a solid first step. But if your nose is stuffed up and you can’t breathe at night? You need more. Combine them with an intranasal corticosteroid if symptoms are moderate to severe. That’s what doctors recommend.
Decongestants: Use With Caution
Decongestants give quick relief - but they’re a trap. Oral decongestants like pseudoephedrine (Sudafed) can unblock your nose in hours. But they’re not meant for daily use. After 3-7 days, they can cause rebound congestion. Your nose gets used to them, then gets worse when you stop. That’s called rhinitis medicamentosa. You end up needing more just to feel normal.
Nasal spray decongestants like oxymetazoline (Afrin) are even riskier. Use them for more than three days in a row, and you’re asking for dependency. I’ve seen patients who’ve been stuck on Afrin for months, their noses swollen shut without it. Don’t go there.
Reserve decongestants for short-term emergencies - like before a flight or a big meeting. Not for daily life.
Immunotherapy: The Only Real Cure
If you’ve tried everything and still suffer, immunotherapy might be your best shot. It’s the only treatment that changes how your immune system responds to allergens. It doesn’t just mask symptoms - it rewires your body’s reaction.
There are two types: allergy shots (subcutaneous immunotherapy, or SCIT) and allergy tablets (sublingual immunotherapy, or SLIT). Shots are given weekly at first, then monthly. They’re effective - 35-45% symptom reduction - but require frequent visits. SLIT tablets, like Oralair or Grastek, dissolve under your tongue. You take them daily at home. They’re less effective than shots (30-40% reduction), but way more convenient.
Here’s the kicker: you need to start SLIT at least four months before pollen season. And you have to stick with it for three to five years. Most people quit within the first year. Why? Oral itching. About two-thirds of users feel their tongue tingle or itch. It’s not dangerous, but it’s annoying. And you can’t eat or drink for five minutes after taking the tablet.
Still, 85% of patients prefer SLIT over shots. And for kids? The data is even stronger. One study showed kids with allergic rhinitis who got immunotherapy were 67% less likely to develop asthma later. That’s huge.
Side effects? Rare, but real. Severe reactions happen in 1.2% of SLIT users and 0.2% of shot users. That’s why the first dose of SLIT is always given in a doctor’s office - with epinephrine on hand.
Environmental Control: The Silent Weapon
Medicines help. But if you keep breathing in allergens, you’re fighting a losing battle. Real relief comes from reducing exposure.
For dust mites: wash bedding weekly in water hotter than 130°F (54°C). Use allergen-proof covers on your mattress and pillows. They cut exposure by 83%. Keep indoor humidity below 50% with a dehumidifier. Dust mites can’t survive in dry air.
For pet dander: keep pets out of the bedroom. Use a HEPA air filter in your main living area. Bathe your dog or cat weekly. It reduces airborne dander by up to 80%.
For mold: fix leaks. Clean bathrooms with bleach or vinegar. Don’t let damp towels sit around. Mold grows fast in Perth’s humid winters.
For pollen: check daily counts. When levels hit 9.7 grains per cubic meter, keep windows closed. Wear wraparound sunglasses outside - they reduce eye symptoms by 35%. Shower and change clothes after being outdoors. Pollen clings to hair and clothes. You’re bringing it inside without realizing it.

New Options: Biologics and Combination Sprays
Things are changing fast. In October 2023, the FDA approved tezepelumab, the first biologic for allergic rhinitis. It blocks a protein called TSLP that triggers the allergic cascade. In trials, it cut symptoms by 42% compared to placebo. It’s not yet widely available, but it’s coming.
Another breakthrough? Combination nasal sprays. Fluticasone and azelastine together (brand name Dymista) deliver both anti-inflammatory and antihistamine effects in one spray. It works faster than corticosteroids alone - relief in 30 minutes - and is 15-20% more effective. If your symptoms are stubborn, this might be worth asking your doctor about.
Apps like Pollen Sense are also helping. People who used them alongside meds saw 28% better symptom control. They alert you when pollen is high, so you can plan ahead - take your meds before going out, avoid jogging at dawn, or close windows.
Why Most People Fail
Here’s the uncomfortable truth: 60% of people with allergic rhinitis start with OTC meds and wait over three years before seeing a specialist. By then, their symptoms are worse, their sleep is ruined, and their productivity is down.
Why? Because they think it’s just a nuisance. But allergic rhinitis isn’t just a runny nose. It’s linked to poor sleep, reduced school and work performance, and even asthma development. It’s a chronic disease - and it deserves real management.
Adherence is the biggest problem. People stop using nasal sprays because they don’t feel instant results. They think antihistamines are enough. They don’t know how to use the spray. They give up on immunotherapy because of oral itching.
But here’s what works: a plan. Know your trigger. Use the right medicine. Use it correctly. Control your environment. Stick with it. If you’re still struggling, see an allergist. Don’t wait.
What to Do Next
Start by tracking your symptoms. When do they get worse? What’s in your environment? Keep a simple log for two weeks. Then, talk to your doctor. Don’t just ask for a prescription. Ask:
- Is this seasonal or perennial?
- Should I try an intranasal corticosteroid?
- How do I use it correctly?
- Do I need allergy testing?
- Is immunotherapy right for me?
Don’t settle for temporary fixes. Allergic rhinitis doesn’t have to control your life. With the right approach, you can breathe easier - every day, all year.
Can allergic rhinitis turn into asthma?
Yes, especially in children. Studies show that kids with untreated allergic rhinitis are more likely to develop asthma later. The inflammation in the nose can spread to the lungs. Immunotherapy can reduce this risk by up to 67% over three years. Managing rhinitis early is one of the best ways to prevent asthma progression.
Are natural remedies like honey or saline rinses effective?
Saline nasal rinses are proven to help. Using a neti pot or squeeze bottle with sterile water twice a day can flush out allergens and reduce symptoms by 30-50% when combined with medication. Honey? No. There’s no solid evidence that local honey reduces pollen allergies. It’s a myth. Stick with science-backed methods.
Do antihistamines lose effectiveness over time?
No, second-generation antihistamines like cetirizine or loratadine don’t lose their effect with long-term use. If they stop working, it’s likely because your exposure to allergens increased, or your symptoms worsened - not because your body got used to the drug. Switching brands won’t help. You may need to add a nasal spray or see an allergist.
Is it safe to use nasal steroids for years?
Yes. Intranasal corticosteroids are designed for long-term use. At standard doses, less than 1% of the medication enters your bloodstream. Side effects like nosebleeds or dryness are rare and usually mild. There’s no evidence they cause weight gain, bone loss, or hormonal issues - unlike oral steroids. They’re among the safest long-term medications available.
When should I see an allergist?
See one if your symptoms last more than three months a year, interfere with sleep or daily life, or don’t improve with OTC meds. Also, if you’re considering immunotherapy or have asthma or sinus infections along with your allergies. Allergists can test for specific triggers and create a personalized plan - not just hand you a prescription.












15 Comments
i just started using flonase last year and holy crap it changed my life. used to be miserable every april, now i can actually breathe at night. the trick is being consistent-i forget sometimes but when i don’t, it’s magic.
you people are so gullible. nasal steroids are just low-dose prednisone with a fancy name. the real solution is avoiding allergens entirely-which no one wants to do because it means giving up pets, windows, and outdoor life. capitalism sold you a spray and called it a cure.
saline rinses work better than most meds i swear. i do it twice a day with distilled water and a neti pot. no side effects no cost just clean sinuses. why are we still talking about drugs when the solution is in the sink
listen if you’re still using benadryl you’re living in 2005. second-gen antihistamines are non-negotiable. and if you think flonase is slow-try using it right. aim toward your ear not your brain. 60% of people spray it wrong. that’s why they think it doesn’t work. it’s not the medicine it’s the technique. fix that first.
the immunotherapy data is compelling but let’s not romanticize it. SLIT requires 3-5 years of daily oral itching and ritualistic avoidance of food for five minutes post-dose. most people quit because it’s not a treatment-it’s a lifestyle overhaul. and yet we call it a ‘cure’ like it’s a magic bullet. the real cure is systemic immune modulation through microbiome restoration-which pharma won’t patent. but here’s the epistemic rupture: we treat symptoms because we don’t have the infrastructure to treat causes. that’s not medical negligence-it’s capitalist epistemology.
why are we even talking about this like it’s complicated 🤡 just take zyrtec and shut the windows. done. i’ve had this since i was 7 and i’m 42 now. no sprays no shots no neti pots. just common sense and a little discipline. why does everyone need a 10-page essay to manage a runny nose
honey doesn't work
just tried the combination spray (dymista) last week. 30 min relief. mind blown. 🤯 i used to need 3 meds just to get through a workday. now it’s one spray. thank you science
i hate how everyone acts like this is just about sneezing. it’s not. it’s the sleepless nights. it’s the brain fog. it’s crying because you can’t breathe while your kid sleeps next to you. i’ve been on flonase for 11 years. i’m not ‘adherent’-i’m surviving. and yes i still get nosebleeds. yes i still feel like i’m drowning in my own sinuses. but i’m here. and i’m not giving up.
you have all missed the fundamental ontological crisis of modern allergic rhinitis: the anthropocene has weaponized pollen. climate change didn’t just raise temperatures-it restructured the very molecular architecture of allergens. ragweed now produces 300% more allergenic proteins than in 1990. we are not treating allergies-we are negotiating with ecological collapse. and yet you all still think a $40 spray is the answer. tragic.
did you know the FDA approves these sprays based on corporate-funded studies? the same companies that make the drugs also pay the researchers. and the nasal spray technique? it was designed to look complicated so you’d need to buy more. they profit from your ignorance. don’t be fooled.
While the pharmacological interventions described herein are statistically significant, one must not overlook the epistemological limitations of symptom-centric paradigms in immunological pathology. The reductionist model of allergic rhinitis as a discrete clinical entity obscures the broader neuroimmunological continuum that undergirds chronic inflammatory states. A truly rigorous approach necessitates a biopsychosocial framework that accounts for psychosocial stressors as modulators of mast cell degranulation. To prescribe solely based on allergen exposure is to commit the fallacy of misplaced concreteness.
omg i just realized i’ve been spraying flonase straight back too 😭 i’ve been doing it wrong for 3 years. thank you for that tip. going to try again tonight
if you’re not using a HEPA filter you’re wasting your time. period. my dog sheds like a furry tornado but the filter catches 99% of it. no more sneezing fits at 3am. also i got a dehumidifier. mold is a silent killer. 🏠💨
the real villain here isn’t pollen-it’s the american dream. you want to live in a house with windows? own a pet? go outside? sorry, your immune system is now a liability. we’ve engineered a world that makes you allergic to your own existence. the only cure is to move to a bio-dome in Antarctica. or at least stop pretending this is normal.