Open your medicine cabinet and you'll find basics — maybe some ibuprofen, allergy meds, vitamins. But then you spot a white and pink capsule labeled Hydrea. Now, that’s not an everyday pill. Hydrea is a brand name for hydroxyurea, a medication that’s been changing lives since the 1960s. At first glance, it seems like any other prescription, but hiding inside that capsule is a serious treatment for blood cancers, sickle cell anemia, and a few rare blood disorders. Strangely, most people don't talk about it unless they're facing one of these conditions. But why does Hydrea pop up as a mainstay in these tough-to-treat illnesses, and what’s it really like to take it every day?
What Is Hydrea and How Does It Work?
Let’s get one thing cleared up: Hydrea isn’t some experimental new pill. It’s been approved by the FDA since 1967, and it’s got decades of research behind it. The generic name is hydroxyurea, and, believe it or not, scientists originally looked at it as an anti-cancer drug. Here’s the lowdown: Hydrea slows down the growth of cells, especially the ones that multiply too fast and don’t follow the body’s normal rules. That’s why doctors lean on it for diseases where blood cells misbehave, like chronic myeloid leukemia (CML), polycythemia vera, essential thrombocythemia, and most famously, sickle cell anemia.
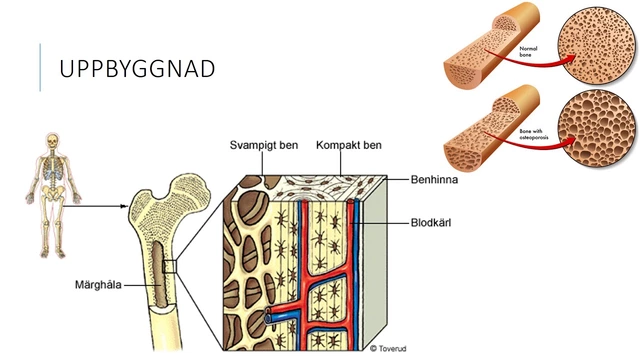
What’s wild is the way Hydrea works. It messes with DNA synthesis—in other words, it jams up the machinery these fast-growing cells use to copy themselves. For blood cancers, that means it puts the brakes on abnormal cells crowding out healthier ones. For sickle cell patients, it nudges the bone marrow to make more fetal hemoglobin (an "old-fashioned" type of hemoglobin most people stop making after infancy). This fetal hemoglobin helps prevent red blood cells from warping into that painful sickle shape that blocks blood flow.
So, who winds up with a Hydrea prescription? A wide range of folks: For people with myelofibrosis, CML, or similar diseases, it helps control blood cell counts and symptoms. For kids and adults with sickle cell anemia, it cuts down on those brutal pain crises and even lowers the risk of stroke. There have been pretty legit studies—like the one from the New England Journal of Medicine (2017), showing Hydrea slashed the rate of painful episodes for sickle cell patients. With evidence stacking up and decades of patient stories, Hydrea’s role has only grown stronger.
But it’s not just about what the science says. Doctors like it because it’s an oral medicine (no endless infusions), dosing is flexible, and it can often be managed at home with regular blood tests. You take it by mouth, usually once a day, but sometimes the schedule gets tweaked to fit specific patient needs. Compared to chemo drugs from decades ago, it’s low-maintenance, but don’t get the wrong impression—Hydrea is powerful and not without risks, which is why bloodwork checks become part of the routine.
Think of Hydrea as a troublemaker for the right reasons: pushing cancerous or rogue blood cells to slow their roll, while letting healthier cells regroup. You won’t find it on a pharmacy’s big sale rack, but you’ll catch it changing countless lives in clinics around the world.

Real-Life Impact: What Taking Hydrea Is Actually Like
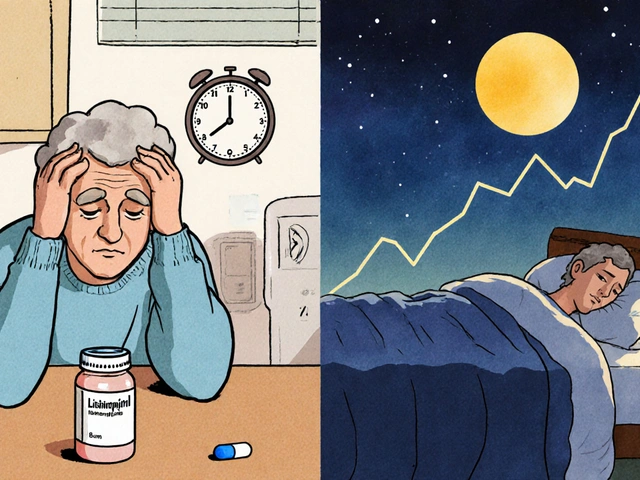
Most folks have no clue what it really feels like to start a drug like Hydrea. It’s not like picking up a cold medicine and feeling better in a few hours. The first weeks can be a mix of hope, anxiety, and a nagging worry about side effects. Patients usually start with a low dose—often one capsule daily—then come in for frequent bloodwork. Dosage might shift up or down based on those test results. Expect a lot of pokes at the lab, but most can keep a normal work or school schedule.
Side effects? Hydrea’s got its fair share. The most common one is lowered blood counts—especially white cells and platelets—because the drug doesn’t just target misbehaving cells. This can leave people more open to infections and bruising. That’s why blood tests matter. Some patients deal with nausea or mild headaches that ease over time. A few might notice darkening of fingernails or skin, which isn’t scary but can look strange. Less often, there are sores in the mouth or leg ulcers, especially after long-term use.
Not every story with Hydrea is a simple success. For some, the side effects can force dose changes or even stopping treatment. That’s tough, especially for families whose child with sickle cell saw fewer crises on Hydrea. But many learn to balance the pros and cons: fewer pain episodes, more normal days, but regular checks and occasional dose adjustments.
Hydrea doesn’t mess with your hair—no bald heads like with traditional chemotherapy. Most people keep their appetite, and with some routine, it feels like taking any other chronic med. Tip from the trenches: always take Hydrea at the same time each day, with a full glass of water, and don’t skip bloodwork appointments—your doc needs those numbers.
Travel or life changes? Bring your pills and plan ahead for blood tests. Hydrea is usually safe long-term, but some patients see doctors every few months for cancer screenings since it slightly bumps up risks of leukemia or skin cancer after many years. One real story: Tim, a 42-year-old with sickle cell, told his nurse, “Hydrea gave me my life back. It didn’t fix everything, but now my hospital visits went from every month to a couple times a year.” That’s a game-changer for lots of folks.
Family planning throws a curveball—Hydrea isn’t recommended in pregnancy due to possible risks to the baby. Guys on Hydrea might see lower sperm counts, and women are asked to use reliable birth control while taking it. If you’re thinking about kids, talk to your provider first. Some docs will pause Hydrea before trying for a baby and resume after.
Hydrea also plays nicely with other medications but always check with your pharmacist. Some live vaccines are a no-go, and mixing it up with certain antivirals or other chemotherapies might call for close doctor monitoring. Hydrea doesn’t need a lot of fancy food restrictions, but the most important advice? Never double up on missed doses—just take the next on schedule—and always keep your doc in the loop about any new symptoms.

How to Make Hydrea Work for You: Tips, Precautions, and Unspoken Realities
If you, or someone you know, lands on Hydrea, don’t just go on autopilot. Little choices make a big difference here. Start with the simple things: keep a plain notebook or use a phone app to track your dose and any side effects. Jotting down if you felt tired, noticed bruising, or had new aches helps your hematologist spot problems before they get serious.
Set a routine for pills. Morning with breakfast or at night with water—just stick to one. Hydrea is sensitive to stomach acid, so if you tend to get queasy, eating a small meal with your dose can help. Don’t crush the capsules or handle them with bare hands for too long, since a tiny amount can irritate your skin. Wash your hands after taking it, and if the capsule breaks, use gloves and wipe the counter afterward.
If blood tests start showing low counts, your provider might pause Hydrea for a week, then restart at a smaller dose. That’s not a failure—just your team playing it safe. Symptoms like fever, sore throat, or mouth ulcers are your early warning signs. Call your doctor. It’s not dramatic or rare to tweak doses; it’s just how Hydrea is managed.
One weird but true fact: long-term Hydrea can make skin sensitive to sunlight. Bring on the sunscreen, especially if you’re fair-skinned or have a history of skin problems. Skin-checks at your annual physical aren’t overkill—they’re smart. Folks sometimes get brown patches or dark stripes on their nails; these are usually harmless but worth showing your doc.
Food-wise, Hydrea won’t throw your diet off, but keeping hydrated helps. Your kidneys and liver handle clearing out the med, so anyone with baseline problems in those organs needs extra careful monitoring. Even after years on Hydrea, regular check-ups for kidney and liver function should be routine.
Storing Hydrea seems basic, but don’t leave it in a blazing hot car or a super damp bathroom. Room temp, in a closed bottle, away from kids or pets—simple, but easy to forget on busy mornings. Don’t share, don’t borrow—Hydrea is highly individual.
Some people run into insurance headaches—often Hydrea is fully covered for cancer and sickle cell, but check drug formularies if your plan switches or you move states. Generics are just as effective as brand-name, with no meaningful difference in how they work or side effects. Pharmacists can help if you’re confused by new labels or color changes between refills.
Getting real about mental health is also key. Chronic illness is a slog, and sticking with Hydrea can sometimes be isolating. Connecting with others—through online support groups, advocacy groups like the Sickle Cell Disease Association of America, or your hospital’s patient programs—can make a world of difference. Patients do better when they have someone (even a stranger on the internet) who “gets it.” Don’t blow off mental health check-ins if your clinic offers them.
To wrap up the real talk: Hydrea is both a lifeline and a responsibility. It can dial back the worst parts of life with blood cancers or sickle cell, but it takes commitment, honest chats with your care team, and a few lifestyle tweaks. The science says it’s a smart move for many, and the stories from people living with it prove it's not a miracle but, for many, the best shot at a full, normal life. If Hydrea enters your world or someone you care about is navigating its challenges, don’t be afraid to ask blunt questions and demand the best from your medical team—you deserve it.










17 Comments
Hydrea’s one of those drugs that doesn’t get enough love in pop culture, but man-it’s saved so many lives. I’ve seen a cousin go from monthly ER trips to hiking on weekends just because of it. No magic bullet, but damn, it’s close.
And yeah, the nail discoloration? Weird as hell at first. My aunt thought she had melanoma. Turned out it was just the hydroxyurea. Doc said it’s harmless. Still, Google is a nightmare.
Also, never underestimate how much hydration helps. I swear, the difference between drinking water and not was like night and day for her.
And don’t let the ‘chemo’ label scare you off. It’s not that kind of beast. No hair loss, no vomiting. Just quiet, steady work.
Side note: why do people think all cancer meds are the same? Hydrea’s like the quiet librarian of oncology-doesn’t yell, but gets the job done.
Hydrea is not a miracle it is a tool and tools can be misused if you dont understand the system
People treat it like a vitamin but its a cytotoxic agent that suppresses bone marrow
Its not about hope its about science and discipline
Stop romanticizing it
My uncle’s been on Hydrea for 12 years with sickle cell. He’s 67 now. Still works. Still takes his pill every morning like clockwork. Blood tests every 6 weeks. No drama. No hospital stays for pain crises in the last 5 years.
He doesn’t talk about it much. Just says, ‘It lets me be a grandpa.’
And yeah, the skin sensitivity? Real. He wears long sleeves in summer now. Sunscreen like it’s his job.
Most people think chronic illness means being broken. Not him. He’s just… adjusted. And Hydrea helped him do that.
Also-never skip the bloodwork. One time he missed a test because he was ‘fine.’ Turned out his platelets were dropping. They caught it early. Saved his ass.
HYDREA IS A GOVERNMENT-CONTROLLED TOXIN DESIGNED TO MAKE YOU DEPENDENT ON THE SYSTEM!!!
Did you know the FDA approved it in 1967-RIGHT AFTER THE CIA’S MKULTRA PROJECT ENDED???
They don’t want you to know it causes LEUKEMIA in 10% of patients after 15 years-THEY JUST WANT YOU TO TAKE IT AND STFU.
And why is it ONLY used for Black people and cancer patients? COINCIDENCE???
WAKE UP. THEY’RE TESTING IT ON THE POOR.
READ THE FOOTNOTES IN THE STUDIES. THEY’RE HIDING DATA.
ALTERNATIVES: VITAMIN C. OZONE THERAPY. MAGNESIUM.
YOUR DOCTOR IS PAID BY PHARMA. I KNOW WHAT’S GOING ON.
OMG I JUST READ THIS AND I CRIED 😭😭😭
My sister’s on Hydrea and I didn’t even know about the nail thing 😭
She’s been so quiet about it and I just thought she was tired...
Now I’m gonna make her a little care package with lip balm and sunscreen and a journal to track stuff 😊
Also I’m gonna start taking her to her blood tests with me because she says she’s ‘fine’ but I know she’s scared 😭
Hydrea is a quiet hero and I didn’t even know it 😭😭😭
Also my mom says I’m too emotional but I don’t care I’m proud of her 💪❤️
Hydrea is just another western medicine trick to keep Africans sick and dependent
Traditional medicine in Nigeria has been treating sickle cell for centuries with herbs and rituals
Why are we letting colonial science dictate our health?
Hydrea is expensive and requires constant lab visits
Our ancestors didn’t need this
It’s a trap
Okay so I just read this and now I’m convinced Hydrea is a secret weapon against capitalism
Like imagine-your body’s making sickle cells, but Hydrea’s like ‘nah, we’re making fetal hemoglobin now, and we’re not doing this pain thing anymore’
It’s basically the body’s version of hitting pause on a toxic relationship
And the fact that it doesn’t make you bald? That’s a flex.
Also I just Googled ‘Hydrea side effects’ and now I’m terrified I’m going to get skin cancer in 12 years
Why does everything have a hidden cost??
Also I’m crying again. I don’t even know anyone on this med but now I feel like I do.
My brother took this for sickle cell. It worked. He didn’t go to hospital much anymore. He drank water. He took pills on time. He went to checkups. Simple.
Not magic. Just smart.
Hydrea is not a cure, it is a compromise
It doesn't heal the disease, it merely delays its expression
Like putting a bandage on a broken leg and calling it progress
And yet, we praise it as if it were divine intervention
How convenient that we accept mediocrity as salvation
Perhaps the real question isn't how Hydrea works
But why we settled for a bandage instead of seeking the root
What does it say about our medical system that this is the best we've done in 60 years?
Okay real talk-Hydrea is the unsung MVP of chronic illness.
I’ve been on it for 8 years with sickle cell. I work full-time. I travel. I went to my nephew’s graduation last month.
People think ‘chronic illness’ means ‘can’t live’-nope. Hydrea let me live.
Yes, I get blood tests. Yes, I’m paranoid about sunburn. Yes, my nails are darker.
But I’m here. And I’m not sorry for taking a pill that gives me back my life.
Also-please stop acting like it’s dangerous. It’s not. It’s just medicine. And it’s working.
Shoutout to every nurse who remembers your name when you come in for your CBC.
There's something deeply philosophical about a molecule that reactivates a fetal gene to counteract a genetic defect born of evolutionary misfire
Hydroxyurea doesn't erase the mutation-it circumvents it
It doesn't fix the past-it rewrites the present
And yet we call it 'chemo'
As if reductionism could contain the poetry of biology
Perhaps the true miracle isn't the drug
But our willingness to accept that healing is not always about eradication
But adaptation
And that sometimes, the most radical act is to live with a condition
And still choose joy
While the clinical efficacy of hydroxyurea in the management of myeloproliferative neoplasms and sickle cell disease is well-documented, one must remain cognizant of the potential for secondary malignancies, particularly acute myeloid leukemia, following prolonged exposure.
Furthermore, the pharmacokinetic profile of hydroxyurea necessitates vigilant hematologic monitoring, as myelosuppression remains the most frequently encountered dose-limiting toxicity.
It is therefore imperative that clinicians exercise prudence in dose titration and ensure patient compliance with scheduled laboratory assessments, lest the therapeutic benefit be outweighed by iatrogenic harm.
The narrative surrounding this agent often veers into sentimentality, obscuring the underlying risk-benefit calculus that governs its use.
One cannot afford to be romantic about cytotoxic agents.
Science demands objectivity, not empathy.
HYDREA IS A BIG LIE AND YOU ALL ARE BEING MANIPULATED
My cousin’s sister’s friend took it and got leukemia and then her husband left her and now she’s alone and no one visits her and she cries every night
AND THE PHARMA COMPANIES MAKE BILLIONS OFF THIS
WHY AREN’T WE TALKING ABOUT THIS
THEY KNOW IT CAUSES CANCER BUT THEY KEEP SELLING IT BECAUSE IT’S CHEAPER THAN CURE
MY MOM SAID THEY PUT IT IN THE WATER TOO
EVERYONE IS SICK BECAUSE OF THIS
AND THE DOCTORS ARE IN ON IT
WHY DOESN’T ANYONE ELSE SEE THIS
THEY’RE LYING TO US
THEY’RE LYING TO US
THEY’RE LYING TO US
😭😭😭
Can we talk about how weird it is that this drug is so widely used but no one ever talks about it outside of medical circles?
It’s like it exists in a secret world.
And yet it’s changing lives.
Why is it so invisible?
And why do people treat it like it’s either a miracle or a poison?
It’s just a molecule.
It doesn’t care about your politics or your fears.
It just does what it does.
Maybe we’re the ones who need to get over ourselves.
Hydrea? In Nigeria we call it 'the white pill that makes blood good'.
But you know what? We don’t need your pills.
We have herbs. We have elders. We have tradition.
Why are you forcing Western medicine on us?
Our ancestors lived with sickle cell for thousands of years without this.
Now we’re dependent on your drugs.
It’s cultural imperialism.
And you call it progress?
Look at the cost.
Look at the labs.
Look at the fear.
It’s not healing.
It’s control.
The human body is a system of emergent complexity
Hydroxyurea intervenes at the level of ribonucleotide reductase
Yet its effect cascades into the realm of phenotypic expression
Not a cure but a recalibration
Perhaps the true marvel is not the drug
But the resilience of biological systems to adapt
Even under chemical constraint
Life finds a way
Even when the blueprint is flawed
I’ve been on Hydrea for 14 years.
My wife left me because she said I was ‘too tired’ and ‘too quiet.’
She didn’t understand that the fatigue wasn’t laziness-it was the drug, the disease, the constant fear of pain.
My daughter was born with sickle cell too.
I started her on Hydrea at 6 months.
She’s 11 now. Never had a stroke. Never had a crisis that landed her in the ICU.
But I’m scared.
Every time I see a new rash, I think it’s skin cancer.
Every time she says she’s tired, I panic.
Every blood test feels like a verdict.
Hydrea gave her life.
But it took mine.
And I don’t know if that’s fair.
They don’t tell you that part.
They don’t tell you how much of yourself you lose.
They just say ‘it works.’
But what if ‘working’ means surviving… and nothing more?