Warfarin Alcohol Risk Calculator
Understand Your Risk
This tool helps determine if your alcohol consumption exceeds safe limits while on warfarin. Based on NIAAA guidelines and clinical studies showing increased bleeding risk.
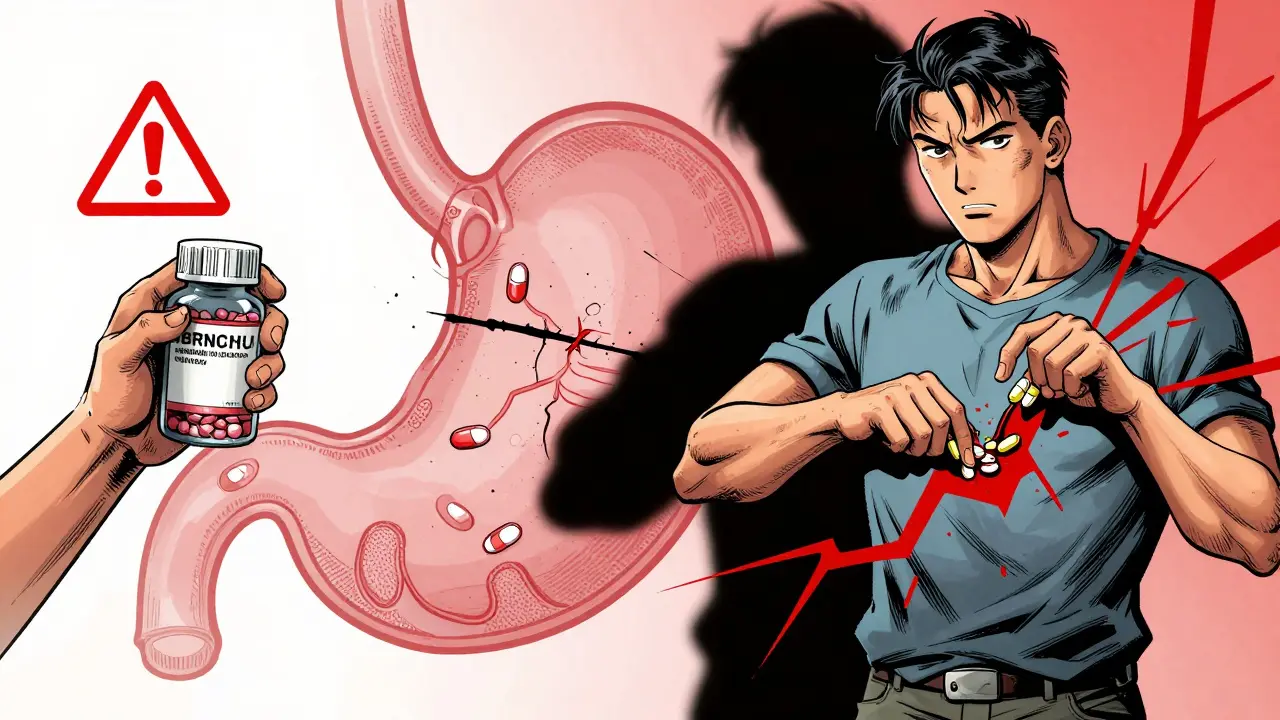
If you're on warfarin, drinking alcohol isn't just a social choice-it's a medical decision with real consequences. Binge drinking while taking this blood thinner can send your INR levels into dangerous territory, increasing your risk of internal bleeding, stroke, or even death. This isn't a hypothetical warning. It’s backed by years of clinical data, hospital records, and patient outcomes. And yet, many people still think, "I only drink on weekends," or "I’ve been on this medicine for years, I know my body." Warfarin is one of the most commonly prescribed anticoagulants in the world. It’s used to prevent clots in people with atrial fibrillation, artificial heart valves, deep vein thrombosis, or pulmonary embolism. Its effectiveness depends on keeping your INR (International Normalized Ratio) between 2.0 and 3.0. Too low, and you’re at risk of clotting. Too high, and you’re at risk of bleeding. Even a small shift outside that range can be dangerous. Now add alcohol-especially binge drinking-to the mix. And things get unpredictable. The National Institute on Alcohol Abuse and Alcoholism defines binge drinking as five or more drinks for men, or four or more for women, within about two hours. That’s not a few beers over dinner. That’s a rapid spike in blood alcohol levels. And for someone on warfarin, that spike can trigger a cascade of biochemical chaos. Here’s how it works. Warfarin is broken down in your liver by enzymes called CYP2C9 and CYP3A4. Alcohol competes for the same enzymes. When you drink heavily in a short time, those enzymes get overwhelmed. Warfarin doesn’t get metabolized as quickly. It builds up in your bloodstream. Your INR shoots up. Your blood thins too much. You’re now at risk of bleeding out from a minor fall, a nosebleed that won’t stop, or even a headache that turns into a brain hemorrhage. But here’s the twist: it’s not always immediate. After a binge, your liver can start producing more of those enzymes to clear the alcohol. That means in the days after drinking, warfarin gets broken down too fast. Your INR drops. Now you’re at risk of a clot forming. This rollercoaster-INR up, then down, then up again-is why doctors call it "unpredictable." It’s not just risky. It’s impossible to manage. A 2015 study from the University of Michigan tracked over 1,200 warfarin patients and found that those who binge drank had a 2.3 times higher risk of major bleeding. For people who’d been on warfarin more than a year? That risk jumped to 3.1 times higher. Why? Because long-term alcohol use damages the liver, which is already working hard to produce clotting factors. Add warfarin, and the system starts to fail. And it gets worse if you have certain genetic variants. About 10% of people carry a CYP2C9*2 or CYP2C9*3 gene mutation. These variants slow warfarin metabolism by 30% to 90%. For someone with this mutation who binges, the risk of bleeding skyrockets-up to 4.2 times higher. That’s not a small risk. That’s a medical emergency waiting to happen. The NHS, the British Heart Foundation, and the American Heart Association all agree: if you’re on warfarin, binge drinking is off-limits. The NHS says it plainly: "Drinking heavily, especially binge drinking lots of alcohol in one go, is dangerous while taking warfarin. The alcohol can increase the risk of bleeding." The British Heart Foundation adds a practical guideline: if you drink at all, stick to no more than 14 units a week-and never consume them all in one sitting. One unit is roughly half a pint of beer, a small glass of wine, or a single shot of spirits. That’s not a lot. And it’s not a suggestion-it’s a safety rule. The University of Iowa Health Care is even more direct: "No more than two drinks a day for men, one for women. And never binge." But here’s the reality: most people don’t track their drinks. A "glass" of wine at dinner might be a full 250ml pour-almost two units. A "shot" of whiskey might be 50ml, not 25ml. A "beer" might be a large 600ml bottle, not a standard 330ml one. Without knowing exactly what you’re consuming, you’re guessing-and guessing with warfarin is dangerous. And it’s not just about INR. Alcohol can also damage your stomach lining, cause ulcers, and irritate your esophagus. Combine that with a thinning blood effect from warfarin, and even a small tear can lead to massive internal bleeding. That’s why warning signs like black, tar-like stools, bright red vomit, or urine that looks like cola aren’t just "weird symptoms." They’re red flags for life-threatening bleeding. The FDA removed warfarin’s black box warning about alcohol in 2010 because, at the time, the evidence wasn’t considered strong enough. But since then, multiple studies-including the 2015 Sung study and the 2017 Blood journal review-have proven otherwise. In 2022, the American College of Physicians formally petitioned the FDA to reinstate the warning. The evidence is now overwhelming. What should you do? If you’re on warfarin and you drink:
- Absolutely avoid binge drinking. Never have more than two drinks in one sitting.
- Don’t save up your weekly alcohol allowance for one night. Spread it out. And even then, stick to one drink per day for women, two for men.
- Get your INR checked within 72 hours after any alcohol consumption, especially if you drank more than usual.
- Tell your anticoagulation clinic or pharmacist every time you drink-even if you think it’s "just one."
- Know the signs of bleeding: unusual bruising, nosebleeds that won’t stop, blood in urine or stool, severe headaches, dizziness, or weakness.











13 Comments
bro i just had 3 beers last friday and my INR went from 2.4 to 4.1 the next day… my pharma told me to hold warfarin for 2 days and i thought they were overreacting. turns out i was 12 hours away from a nosebleed that wouldn’t stop. never again. 🤢
so let me get this straight - you're telling me i can't have my weekly 12-pack and expect my blood to behave? what a joke. everyone knows alcohol is just water with extra steps. if your liver can't handle it, maybe you shouldn't be on warfarin.
it’s not about moderation. it’s about the illusion of control. we tell ourselves we’re the exception - "i know my body," "i’ve been fine for years." but the liver doesn’t care about your story. it just metabolizes. and when it’s overwhelmed? your INR becomes a roulette wheel. and you’re the one spinning.
as someone who lost her father to a spontaneous intracranial hemorrhage while on warfarin - he had "just one drink" at his grandson’s birthday - i can tell you this isn’t theoretical. it’s a quiet killer. please, if you’re reading this: don’t gamble with your life. one night of celebration isn’t worth a lifetime of silence.
the real issue here is access. not everyone has a pharmacist who checks in, or a clinic that tracks their drinking. if you’re low-income, rural, or undocumented - you’re flying blind. this advice is great, but it assumes resources that don’t exist for millions. we need systemic support, not just warnings.
yo so cyp2c9 polymorphisms are a thing? i had genetic testing done last year and i’m cyp2c9*3/*3. so basically my liver is a snail. i drink one glass of wine and my inr spikes like a rocket. doc told me to just skip it. i did. no regrets. also, doac’s are way better if you’re gonna drink even a little. no more finger pricks.
you got this 💪 seriously - if you're on warfarin and you want to live to see your kids graduate, cut the binges. it’s not about being perfect, it’s about being present. i started using a drink tracker app and it changed my life. you can too!! 🥂🚫
oh wow. so the government finally noticed that alcohol + blood thinners = bad? took them long enough. guess they were too busy banning glitter and soda in schools. meanwhile, my uncle had a stroke after "just one beer" at his retirement party. they didn’t even ask him if he drank. classic.
the "two drinks a day" guideline is laughable. you think people actually measure their pours? a "glass" of wine in the US is 7oz. that’s 2.3 units. you’re not telling people to drink responsibly - you’re telling them to become lab technicians.
i’ve been on warfarin for 8 years. i have one drink every other night - just a glass of wine. never binged. never had an issue. my INR’s always stable. i think the fear here is overblown for people who actually monitor themselves. not everyone’s a ticking bomb.
so you’re saying i can’t have a celebratory whiskey after my wife’s cancer remission? because apparently my joy is a medical hazard now? great. next they’ll ban hugs and laughter. this isn’t medicine - it’s moral policing wrapped in science.
the real tragedy isn’t the alcohol - it’s the lack of education. i work in a GP clinic. half my patients think "warfarin" is a brand of painkillers. they don’t know what INR means. they don’t know what a unit is. this post is brilliant, but it’s preaching to the choir. we need public health campaigns, not Reddit threads.
...and yet, here we are. another person on Reddit who "knows their body"... while ignoring every clinical guideline since 2010. i swear, if i had a dollar for every time someone said "but i’ve been fine for 15 years"... i could buy a whole pharmacy. your liver doesn’t have a loyalty card.