When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. You don’t want to wonder if it’s weaker, less pure, or unsafe. The truth is, the FDA doesn’t just approve generic drugs based on a paper review. It ensures generic drug quality during manufacturing with a system built on inspection, data, and strict rules that apply to every step of production - from raw ingredients to the sealed bottle on your shelf.
Why Generic Drugs Must Meet the Same Standards
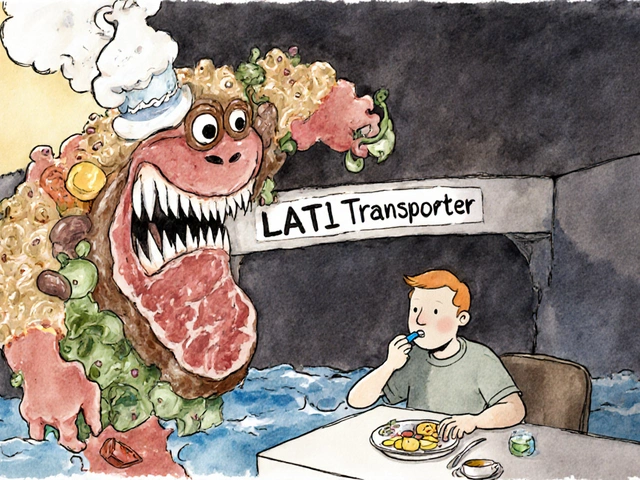
Generic drugs aren’t copies. They’re exact matches in active ingredient, strength, dosage form, and how they’re absorbed by your body. The FDA requires them to be bioequivalent - meaning they deliver the same amount of medicine into your bloodstream at the same rate as the brand-name drug. But that’s only half the story. The other half? How they’re made.Back in the 1960s, the FDA tested over 4,600 drugs and found that 8% of them weren’t delivering the right dose - some were too strong, others too weak. That’s when the agency shifted from checking pills at the end of the line to controlling how they’re made from the start. Today, that approach is called Current Good Manufacturing Practices, or cGMP. It’s not optional. It’s the law.
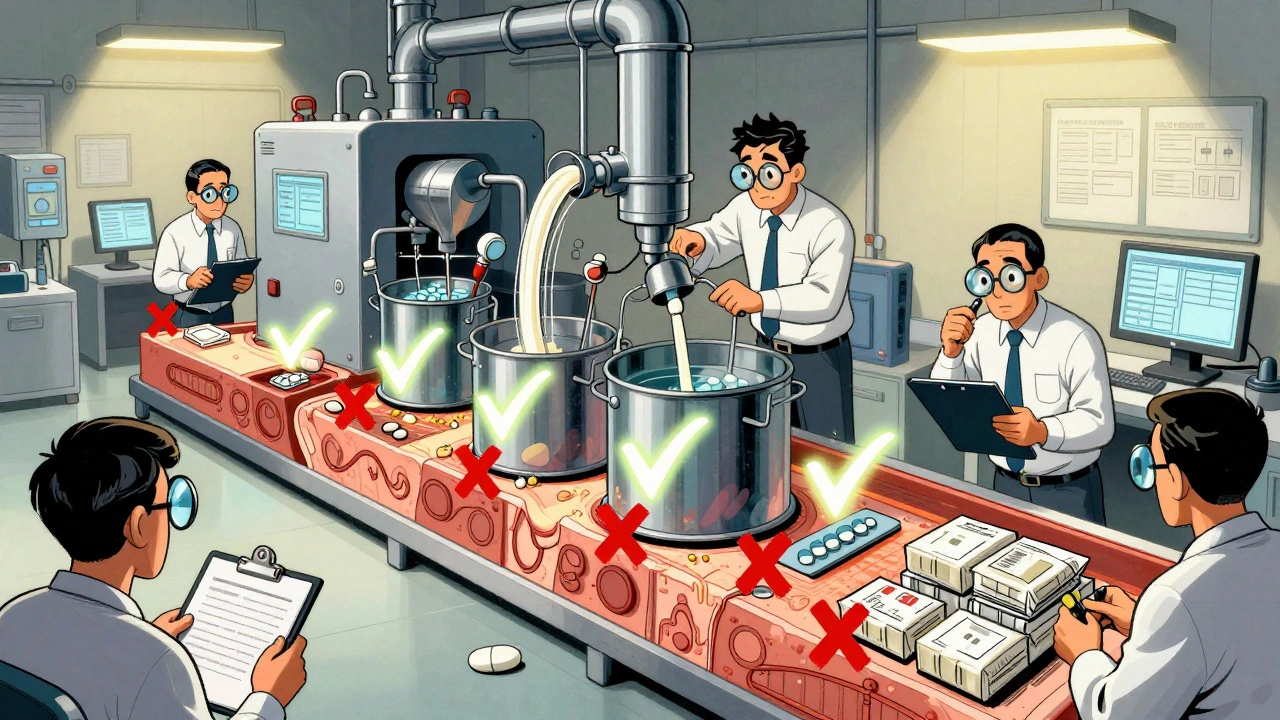
The Five Pillars of FDA Quality Control
The FDA’s system rests on five non-negotiable pillars, each enforced through detailed regulations under Title 21 of the Code of Federal Regulations.- Control of Materials: Every ingredient - from the active drug to the dye in the coating - must be tested and traced. Manufacturers must prove where it came from, how it was stored, and that it hasn’t degraded. No guesswork. No shortcuts.
- Production and Process Controls: Every step in making the drug - mixing, granulating, compressing, coating - must follow a written procedure. Machines are monitored in real time. If a temperature spikes or a blend ratio drifts, the system flags it, and the batch is held until the cause is found and fixed.
- Quality Control and Laboratory Testing: Every batch is tested before release. The FDA requires labs to use validated methods that meet the ALCOA+ standard: data must be Attributable, Legible, Contemporaneously recorded, Original or true copy, Accurate, and also Complete, Consistent, Enduring, and Available. This isn’t paperwork for show. It’s how the FDA traces problems back to their source.
- Packaging, Labeling, and Distribution: Labels must match the approved version exactly. Packaging must protect the drug from moisture, light, and contamination. Even how the pills are shipped matters - temperature-sensitive drugs can’t be left in a hot warehouse.
- Documentation and Record Keeping: Every action, every test, every deviation is documented. These records aren’t stored in a drawer. They’re kept for years and can be pulled at any time during an inspection. If a record is missing, the FDA can shut down production.
Unannounced Inspections - No Warning, No Exceptions
The FDA doesn’t call ahead. Inspectors show up without notice at over 1,200 facilities worldwide each year - including factories in India, China, and the U.S. They don’t just walk through the plant. They sit in the lab, review raw data from machines, check training logs, and interview staff. They stay as long as needed. If they find a violation, they issue a Form 483. If it’s serious, the facility gets a warning letter or is barred from shipping drugs to the U.S.In 2022, 42% of the issues flagged by the FDA in Form 483s were about data integrity - missing entries, backdated records, or altered results. That’s not a technical glitch. It’s a violation of trust. And the FDA treats it like one.

How Generic Drug Applications Are Tested
Before a generic drug is approved, the manufacturer must submit an Abbreviated New Drug Application (ANDA). But the term “abbreviated” is misleading. The review process takes months - sometimes over a year - and includes three critical batches of the drug. One batch is used to make all strengths of the drug. The other two are used to test the lowest and highest strengths. This ensures consistency across the whole product line.And here’s something most people don’t know: the FDA doesn’t just trust what the company says. It can - and does - randomly buy generic drugs off the shelf and test them in its own labs. If the results don’t match the approved specifications, the FDA can pull the product from the market.
Global Standards - Why the FDA Is Different
Other agencies, like Europe’s EMA, have similar rules. But the FDA goes further. It conducts more unannounced inspections. Its documentation requirements are stricter. And it uses a risk-based system to target high-risk changes before they happen - like switching a supplier or changing a machine - instead of waiting for problems to show up in the final product.This isn’t just bureaucracy. It’s prevention. During the pandemic, when supply chains broke down, the FDA’s proactive monitoring helped avoid shortages of critical generics like antibiotics and blood pressure meds. That’s because they were already watching for potential bottlenecks.

Costs and Challenges for Manufacturers
Meeting FDA standards isn’t cheap. A new generic manufacturer typically spends $2 to $5 million just to set up a compliant facility before submitting its first application. Training staff, installing validated systems, and building documentation processes can take 18 to 24 months. Smaller companies often struggle with the paperwork burden - one executive told Pharmaceutical Technology that documentation eats up 30-40% of their development time.But the trade-off is clear: 90% of all prescriptions in the U.S. are filled with generics. And 98-99% of them work just as well as the brand-name version. That’s because the FDA’s system works. It’s not perfect - inspections are limited by staffing, and foreign facilities are harder to monitor - but the data shows results. In 2023, over 1,700 global facilities produced FDA-approved generics, and the vast majority passed inspection.
What’s Next for Generic Drug Quality?
The FDA is moving toward smarter manufacturing. Its Pharmaceutical Quality for the 21st Century initiative is testing new tech like continuous manufacturing - where drugs are made in one seamless process instead of in batches - and real-time release testing, where quality is confirmed as the drug is made, not after.Starting in 2025, new rules will require manufacturers to disclose the full source of their active ingredients. That means knowing exactly where the raw drug came from, down to the farm or lab. It’s another layer of transparency.
The Generic Drug User Fee Amendments (GDUFA) III, which started in 2022, gave the FDA an extra $650 million over five years to hire more inspectors and improve oversight. That money is already being used to expand remote inspections - 35% of inspections in 2022 were done partly online - which saves time and keeps the pipeline moving.
What This Means for You
You don’t need to be a scientist to understand this: the generic drug you take is held to the same standard as the expensive brand-name version. The FDA doesn’t cut corners. It doesn’t rely on trust. It checks. It inspects. It tests. It demands proof. And it acts when things go wrong.That’s why you can trust your generic blood pressure pill, your antibiotic, your cholesterol medicine. It’s not cheaper because it’s worse. It’s cheaper because the patent expired - not because the quality dropped.
When you see the FDA seal on a generic drug, know this: it didn’t happen by accident. It happened because someone, somewhere, followed every rule, recorded every number, and passed every inspection - all to make sure you got the right dose, the right way, every time.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also be bioequivalent - meaning they work the same way in your body. The FDA inspects the same manufacturing facilities and applies the same quality standards. There’s no difference in safety or effectiveness when both are made under FDA oversight.
Does the FDA test generic drugs after they’re on the market?
Yes. The FDA doesn’t just approve drugs - it monitors them after they’re sold. It buys generic drugs from pharmacies and tests them in its own labs. It also collects reports of side effects and quality problems through the Drug Quality Reporting System (DQRS). If a batch fails testing or shows safety issues, the FDA can issue a recall or block further shipments.
Why do some generic drugs look different from the brand name?
By law, generics can’t look exactly like the brand-name drug - that would violate trademark rules. So the color, shape, or inactive ingredients (like dyes or fillers) might be different. But the active ingredient - the part that treats your condition - is identical. These differences don’t affect how the drug works in your body.
Are generic drugs made in the same factories as brand-name drugs?
Yes. Many brand-name manufacturers also make generic versions of their own drugs, often in the same facility. Other generic companies operate their own plants, but they’re held to the same FDA standards. The FDA inspects all of them equally - whether they’re in the U.S., India, or China. Location doesn’t matter; compliance does.
What happens if a generic drug factory fails an FDA inspection?
If violations are found, the FDA issues a Form 483 listing the problems. Serious or repeated issues lead to a warning letter. The facility can’t ship drugs to the U.S. until it fixes the problems and proves compliance. In extreme cases - like falsified data or unsafe conditions - the FDA can block imports or ban the facility permanently. Over 1,700 facilities are inspected each year, and most come into compliance after being given a chance to fix issues.









9 Comments
So basically the FDA just trusts no one. Not the companies, not the data, not even the inspectors. And honestly? That’s the only way it should be. I’ve seen too many ‘trusted’ systems collapse because someone thought ‘it’s probably fine.’
When your life depends on a pill, you don’t want ‘probably.’ You want proof. Every time.
98-99% work fine? That’s not good enough. What about the 1-2% that don’t? Who pays when your blood pressure spikes because the generic didn’t dissolve right? No one. The system’s rigged to look like it’s working while people die quietly.
India makes 40% of the world’s generics… and you’re telling me the FDA trusts them? 😒
My cousin works in a pharma lab in Hyderabad. She says they ‘optimize’ the process to save time. Translation? They cut corners. The FDA doesn’t inspect every batch. They inspect the ones they *think* are clean.
And don’t even get me started on the ‘remote inspections’ 🤡
Generic drugs are a gamble. Don’t pretend otherwise.
While the concerns raised are valid, the FDA’s framework remains one of the most rigorous globally. The ALCOA+ standards alone ensure traceability that most nations cannot replicate. The $650 million investment under GDUFA III is not merely bureaucratic-it’s a safeguard for public health.
Manufacturers in India and China are held to the same standard as U.S. facilities. The data speaks: over 90% of generics pass inspection on first audit. This isn’t luck-it’s discipline.
For those who distrust foreign manufacturing, consider this: 70% of the active pharmaceutical ingredients in U.S. prescriptions originate overseas. The FDA’s system ensures that geography doesn’t compromise safety.
lol the FDA is just a propaganda arm for big pharma. They let all the bad stuff in because they’re paid off. You think they really inspect every lab in China? Nah. They just read the reports the companies write. Same with the ‘random testing’-they pick the easy ones.
And don’t even get me started on how they let these Indian companies get away with everything. We’re basically importing poison and calling it medicine.
I appreciate the depth here. It’s easy to assume generics are just cheap knockoffs, but the reality is far more complex-and reassuring.
The fact that the FDA tests drugs after they hit shelves, and that they can shut down entire facilities over missing records, shows they’re not just checking boxes.
It’s not perfect, but it’s the best system we have. And honestly? I’d rather have a system that’s overcautious than one that’s negligent.
Let me tell you something. In Nigeria, we get generics that make you sick. Not because they’re bad-but because they’re old. Expired. Stored in hot warehouses. No one checks. No one cares.
So when you say ‘the FDA ensures quality,’ you’re talking about America. Outside the U.S.? It’s a lottery. And people die.
The FDA is a bubble. Don’t confuse it with global truth.
India makes the best generics in the world. Period. The FDA is just jealous because we outproduce them. All this talk about ‘data integrity’? That’s just western paranoia. We follow the science, not the paperwork.
And guess what? Our drugs work better than yours. You just don’t want to admit it.
It is profoundly concerning that the public is led to believe that generic drug quality is equivalent to brand-name drugs, when in fact, the regulatory oversight is inherently reactive, not proactive. The notion that inspections are ‘unannounced’ is misleading; they are scheduled within a window of predictability. Furthermore, the reliance on manufacturer-submitted data-however ‘validated’-is a structural flaw. The FDA’s capacity to independently verify is constrained by budgetary and personnel limitations. One must ask: if this system were truly infallible, why do recalls occur? The answer lies not in compliance, but in the illusion of control.