Every time you pick up a new prescription, you get a small paper insert - the Medication Guide. It’s not just a formality. For high-risk drugs, this guide could be the difference between staying safe and ending up in the hospital. The FDA requires these guides for about 150 medications that carry serious, preventable dangers. But most people skim them or ignore them entirely. That’s a mistake. If you’re taking a drug like warfarin, clozapine, or an SSRI antidepressant, this guide holds life-saving details you can’t afford to miss.
What Makes a Medication Guide Different?
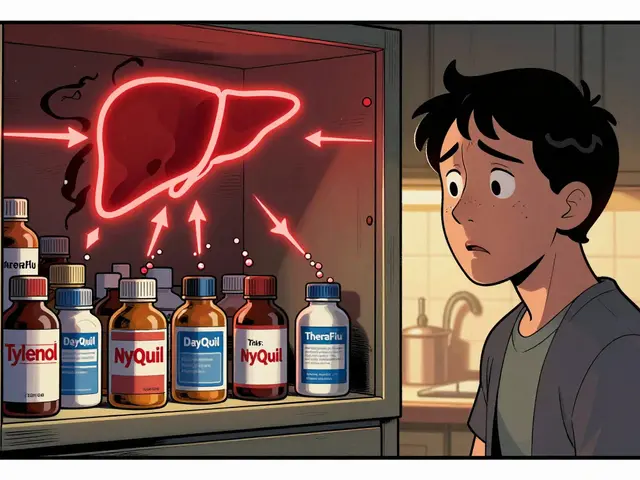
Not all drug paperwork is the same. There’s the tiny leaflet inside the box, the big booklet your doctor gives you, and then there’s the Medication Guide. This one is special. It’s only required when the FDA says the risks are serious enough that patients need to understand them clearly. Think blood clots, liver damage, sudden mood changes, or dangerous drops in white blood cells. These aren’t side effects you can just “tough out.” They need active monitoring - and you’re the one who has to notice the warning signs.Unlike general instructions, Medication Guides are written at a 6th- to 8th-grade reading level. They use plain language. No jargon. No Latin terms. If it says “can cause serious liver damage,” that’s not a suggestion. That’s a red flag. And the FDA makes sure it’s bolded, easy to find, and in at least 10-point font. They even require updates within 30 days if new safety info comes out. In 2022 alone, 92% of these guides were revised. So if you’ve read one before, check again before your next refill.
Where to Find the Real Risk Information
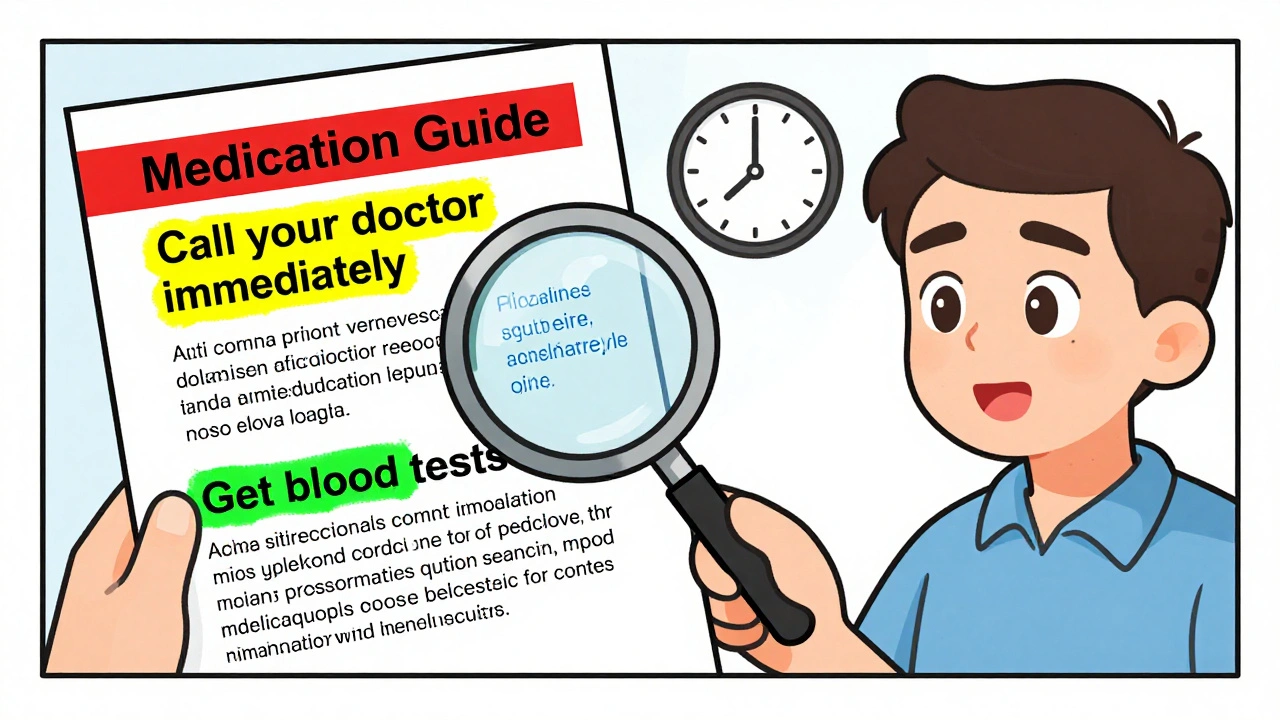
Don’t start at the beginning. Skip the “What is this drug?” part. Go straight to the section titled: “What is the most important information I should know about [drug name]?” This is where the FDA forces manufacturers to put the biggest dangers. This is often called the “black box” warning in plain text. For example, the clozapine guide says: “About 1 in 200 people taking clozapine may develop a condition called agranulocytosis.” That’s not vague. That’s specific. It tells you the exact risk level - and why weekly blood tests are non-negotiable for the first six months.Next, flip to: “What are the possible or reasonably likely serious side effects of [drug name]?” This section doesn’t just list symptoms. It tells you what to do. The tofacitinib guide says: “Get your blood tested regularly to check for changes in blood cell counts.” The warfarin guide doesn’t say “watch for bleeding.” It says: “Call your doctor immediately if you notice unusual bruising, nosebleeds that won’t stop, or red or black stools.” That’s not advice. That’s a checklist.
Link the Side Effects to the Monitoring Schedule
Here’s where most people fail. They read the side effects, then move on. But the real power is in connecting the dots between the warning and the monitoring plan. Look at the section: “How should I take [drug name]?” This isn’t just about dosage. It’s your monitoring schedule.For abiraterone (Zytiga), it says: “Your healthcare provider should perform blood tests before you start and every 3 months while taking this medicine.” For SSRIs like sertraline or fluoxetine, it says: “Pay close attention to any changes, especially sudden changes, in mood, behavior, thoughts, or feelings. This is very important when an antidepressant is started or when the dose is changed.” That’s not vague. That’s time-sensitive. The risk peaks in the first 4-6 weeks. If you’re not watching yourself during that window, you’re flying blind.
Combine the two sections. If the guide says “can cause liver damage,” then look for: “Get liver function tests every 2 months.” If it says “may lower white blood cells,” find: “Weekly blood counts for the first 6 months.” If you don’t see monitoring instructions tied to a risk, ask your pharmacist. That’s not normal. It’s a red flag.
Watch for These 7 Red Flag Phrases
You don’t need to read every word. Look for these exact phrases - they’re your signal to stop and pay attention:- “Get blood tests regularly”
- “Call your doctor immediately if”
- “Do not stop taking without talking to your doctor”
- “Avoid sunlight exposure”
- “Do not drink alcohol”
- “May impair driving ability”
- “Keep all scheduled appointments”
These aren’t suggestions. They’re rules. A 2021 FDA study found that patients who followed these instructions had 32% fewer adverse events. That’s a huge difference. And it’s not because they’re smarter. It’s because they paid attention.
Use the Traffic Light System to Make It Stick
Here’s a trick used by pharmacists across Australia and the U.S.: the traffic light system. Grab a highlighter or pen. Color-code the guide:- Green: Normal side effects - mild nausea, dry mouth, drowsiness. These are common and usually harmless.
- Yellow: Warning signs - mild bruising, slight dizziness, mood swings. These mean you need to monitor. Call your doctor within 24 hours if they get worse.
- Red: Emergency symptoms - bleeding that won’t stop, confusion, chest pain, fever with sore throat, yellowing skin. These mean go to the ER. Now.
Pharmacist Sarah Chen in Perth says this simple method boosts compliance from 45% to 82%. Why? Because it turns abstract warnings into clear actions. You don’t have to remember what “agranulocytosis” means. You just need to know: red = go to hospital.
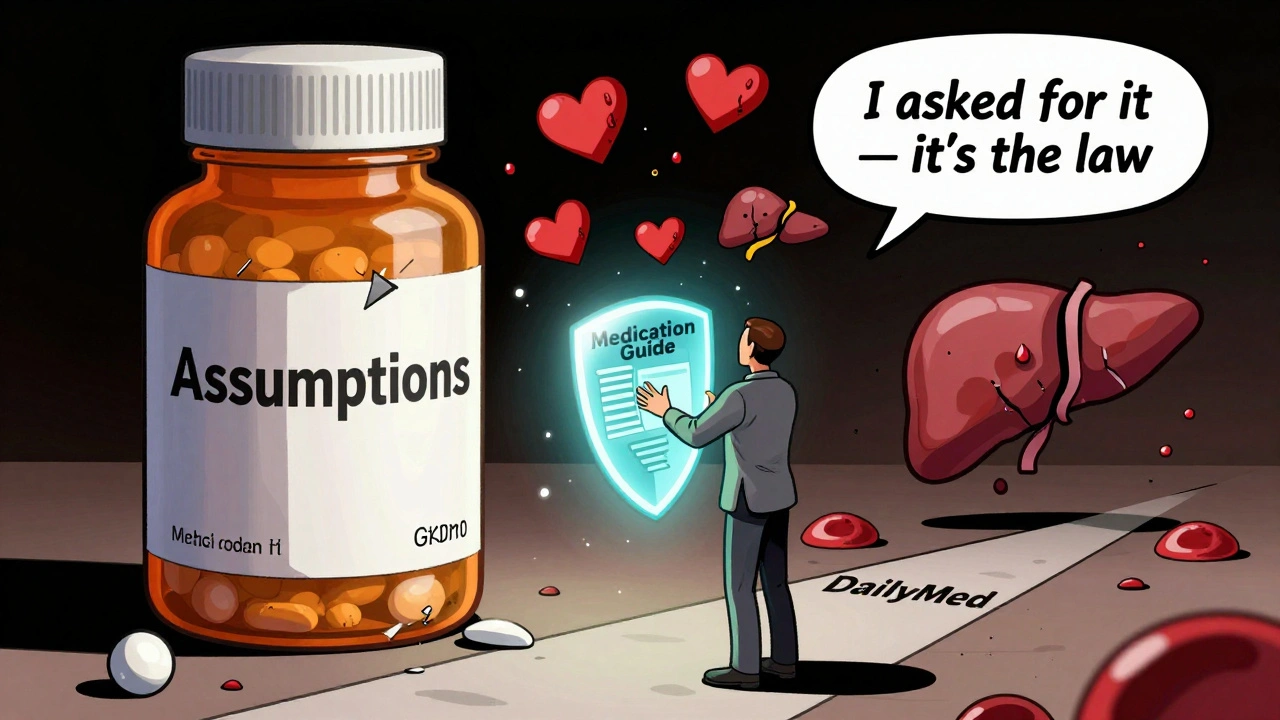
What to Do If You Can’t Find the Guide
The FDA says a Medication Guide must be given to you every time you fill a prescription. But a 2022 audit found 41% of independent pharmacies in the U.S. didn’t consistently hand them out. That’s not okay. If you don’t get one, ask for it. Say: “I need the Medication Guide for this drug - it’s required by law.”If they don’t have it, go to DailyMed (dailymed.nlm.nih.gov), the NIH’s official database. Search by drug name. Download the current version. Print it. Bring it to your next appointment. You’re not being difficult. You’re being smart.
Or use your phone. Many guides now have QR codes on the packaging - especially for cancer drugs and blood thinners. Scan it. You’ll get the latest version, often with videos or animations explaining the risks.
Track It Like a Calendar
If your guide says “blood tests every 3 months,” don’t just hope you’ll remember. Write it down. Use your phone calendar. Set a reminder for the date your doctor needs to order the test. Or better yet - write it in your medication journal. A 2022 University of Michigan study found patients who did this had 68% fewer adverse events.For warfarin users, track your INR numbers. If your dose changes, the guide says to check more often. Mark those dates. If you miss a test, you’re increasing your risk of stroke or bleeding. No one else is going to remind you. It’s your job.
Don’t Rely on Memory - Re-Read Before Every Refill
Guides change. New risks pop up. The FDA updated 147 guides in 2022. That’s almost every single one. So even if you read it last month, read it again before your next refill. Spend two minutes. Look for new bolded warnings. Check if monitoring schedules changed. Did they add a new symptom? Did they shorten the testing window?The FDA recommends the 3-2-1 method: 3 minutes before your first dose, 2 minutes before each refill, 1 minute during treatment if something feels off. That’s less time than it takes to scroll through social media. But it could save your life.
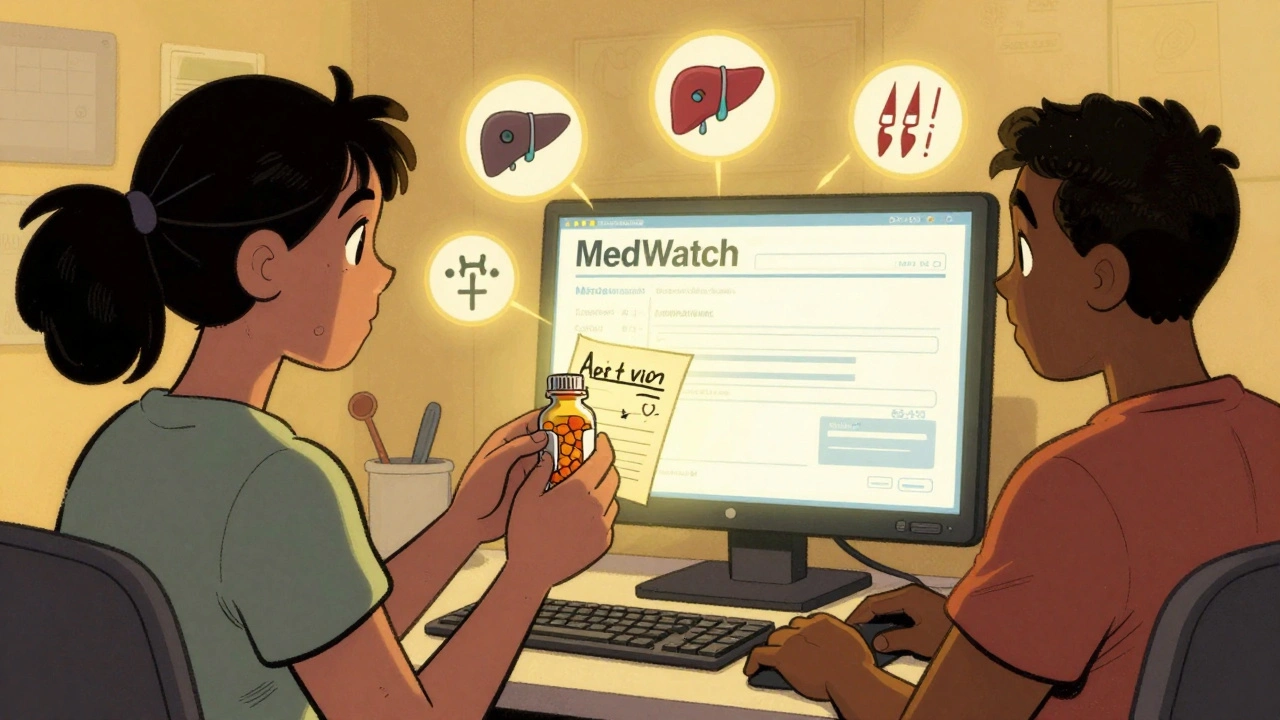
Why This Matters More Than You Think
This isn’t about being a good patient. It’s about survival. The FDA’s own data shows that when patients understand and follow the monitoring advice in these guides, hospital visits drop. Serious reactions drop. Deaths drop.And it’s getting more important. By 2025, Medication Guides will be required for over 120 drugs - up from 42 just a few years ago. Medicare will start penalizing pharmacies that don’t hand them out. Pharmacies are investing millions to make them clearer. AI tools are being tested to personalize them based on your age, weight, and other meds.
But none of that matters if you don’t read them. You’re not just taking a pill. You’re managing a risk. And the guide is your map.
What to Do Next
Here’s your simple action plan:- Find your current Medication Guide - if you don’t have it, download it from DailyMed.
- Open it to the “Most Important Information” section. Read it out loud.
- Find every mention of “test,” “monitor,” or “check.” Circle the time frames (weekly, monthly, etc.).
- Highlight any symptoms that say “call your doctor immediately.”
- Set calendar reminders for each required test.
- Before your next refill, reread it. Look for changes.
You don’t need to be a doctor. You just need to be careful. And that starts with reading the guide - not skipping it.
Are Medication Guides the same as the instructions that come with my pill bottle?
No. The small leaflet inside the bottle is usually just basic dosage instructions. Medication Guides are separate documents required by the FDA for drugs with serious, preventable risks. They’re longer, use plain language, and include specific monitoring instructions and emergency symptoms. You should get one every time you fill a prescription for a high-risk drug.
What if I don’t understand a word in the guide?
Don’t guess. Ask your pharmacist or doctor. Even if the guide is written at a 6th-8th grade level, some medical terms can still be confusing. For example, “agranulocytosis” sounds scary, but it just means your white blood cell count dropped dangerously low. Your pharmacist can explain it in plain terms and tell you what symptoms to watch for. There’s no shame in asking - it’s your safety.
Can I just rely on my doctor to tell me about the risks?
Doctors have limited time and may not remember every detail for every drug. A 2023 study showed that patients who read their Medication Guides caught 40% more potential risks than those who only relied on their doctor’s explanation. The guide is written by experts and reviewed by the FDA - it’s more complete than a quick verbal warning. Use it as your backup system.
Why do some guides seem easier to read than others?
Some guides are better designed than others. Guides for drugs like Humira or warfarin tend to be clearer because they’ve been updated many times and have feedback from patients. Cancer drug guides often feel overwhelming because they list dozens of rare side effects. Look for guides with specific numbers (“1 in 200 people”) and clear monitoring schedules - those are the best ones. If yours feels confusing, check DailyMed for the latest version or ask your pharmacist for a simplified summary.
What if I miss a blood test or monitoring appointment?
Don’t panic - but don’t ignore it either. Contact your doctor or pharmacist immediately. Some drugs, like clozapine or warfarin, can become dangerous if you miss even one test. Your provider may need to reschedule, adjust your dose, or temporarily stop the medication. Never keep taking the drug without the required monitoring. The guide says “do not stop without talking to your doctor” - that’s because stopping suddenly can be dangerous too. Always talk to your provider before making any changes.
Are Medication Guides only for prescription drugs?
Yes. Medication Guides are only required for prescription drugs with serious, preventable risks. Over-the-counter medicines, vitamins, and supplements don’t require them. But if you’re prescribed a drug that affects your blood, liver, brain, or immune system, you’ll get one. If you’re unsure, ask your pharmacist: “Is this drug on the FDA’s list for requiring a Medication Guide?”








9 Comments
OMG I just read this and I’m crying 😭 I’ve been on warfarin for 3 years and never knew to color-code the guide. I’ve been ignoring the ‘call your doctor immediately’ part like it was spam. This is literally life-saving info. Thank you for writing this.
While I appreciate the earnest intent behind this piece, I must respectfully note that the pedagogical efficacy of color-coding risk tiers-though intuitively appealing-is not yet substantiated by large-scale, peer-reviewed clinical trials. The FDA’s mandate for plain-language guides is commendable, yet the introduction of subjective visual heuristics may inadvertently dilute the precision of clinical directives. A more robust approach would integrate structured decision-support algorithms into digital copies of these guides, synchronized with EHRs. Until then, I urge readers to cross-reference with the official MedWatch database, not merely DailyMed.
YESSSSS this is everything!!! 🙌 I’m a nurse in Mumbai and I’ve been teaching my patients the traffic light system for years-green = chill, yellow = call me tomorrow, red = RUN TO HOSPITAL. Last month, a 72-year-old man on clozapine texted me ‘yellow-dizzy + sore throat’ and came in for a blood test. Turns out his ANC was 800. He’s alive because he knew what yellow meant. No one taught him Latin. He learned it through color. 🌈✨ Also-please, PLEASE ask for your guide every time. Pharmacies in India? Half the time they hand you a napkin with ‘take once daily’ on it. Fight for your life. You deserve better.
I’ve worked in UK pharmacies for 18 years. The Medication Guide is the only document patients actually read-when they’re forced to. We used to hide them behind the counter. Now we hand them out with a smile and say, ‘This is your survival manual.’ We’ve seen ER visits for SSRIs drop by 40% since we started asking, ‘Have you read the red section?’ It’s not about intelligence. It’s about access. And if your pharmacy doesn’t give it to you? Walk out. Find one that does.
I’m a single mom of three and I take three prescriptions. I don’t have time to read 12-page PDFs. But I DO have 90 seconds before I swallow my pill. So I open the guide on my phone, scroll to the ‘Most Important Info’ section, and read it out loud while I brush my teeth. I’ve caught two changes in my antidepressant’s warning since last month. My kids say I’m weird for yelling ‘RED FLAG!’ at the fridge. But I’m alive. And that’s the goal.
It is imperative that patients recognize the critical distinction between the Medication Guide and the Patient Information Leaflet (PIL). The former is a federally mandated, FDA-reviewed safety document; the latter is a manufacturer-supplied, often minimally regulated, dosage instruction sheet. Moreover, the 3-2-1 method-though intuitively sensible-is not an evidence-based protocol endorsed by the American College of Clinical Pharmacy. While the traffic-light system is anecdotally effective, its validity hinges on patient literacy, cognitive load, and cultural context. I recommend supplementing this approach with a printed, annotated checklist co-developed with your pharmacist.
Let’s be honest-this is performative patient empowerment. You’re not ‘saving lives’ by color-coding. You’re just making people feel like they’re doing something. Real medicine requires clinical judgment, not highlighters. And why are we trusting the FDA? They approved Vioxx. They approved opioids. The real problem? Doctors don’t have time to explain. So they offload responsibility onto patients who can’t even read the guide properly. This isn’t empowerment. It’s negligence dressed up as a TikTok hack. 🤡
I just want to say thank you to everyone who’s shared their stories here. I’m a veteran with PTSD and I’ve been on sertraline for 8 years. I never knew to look for the ‘sudden mood changes’ part until my sister printed the guide and put it on my fridge. I didn’t realize how much I’d been ignoring. This isn’t about being perfect. It’s about showing up-even if it’s just for two minutes. You’re not alone in this. Keep reading. Keep asking. Keep living.
u r right about the traffic light thing. i used it for my dad on abiraterone. he missed his 3 month test and i almost forgot too. but i had the color coded printout on the fridge. red was circled. i called the doc and they rescheduled same day. he’s ok now. thanks for the tip. btw i think the guide says every 2 months but i read it wrong. my bad. still works tho.