Quick Takeaways
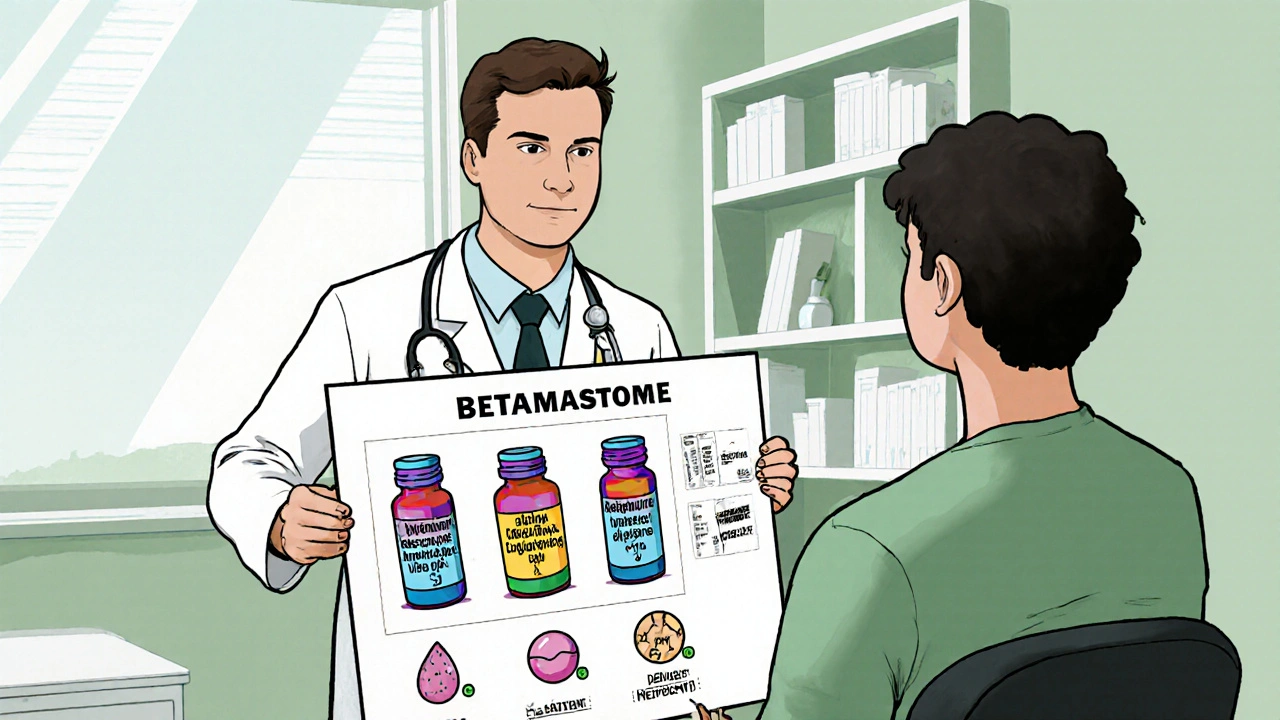
- betamethasone is one of the most potent topical and systemic corticosteroids available.
- Potency, duration of action, and formulation differ markedly from prednisone, dexamethasone, hydrocortisone and methylprednisolone.
- Higher potency means faster symptom relief but also a greater risk of systemic side effects.
- Choosing the right steroid hinges on the condition, treatment length, and patient‑specific factors such as age and comorbidities.
- Always follow a prescriber’s guidance; abrupt discontinuation can trigger adrenal insufficiency.
What is Betamethasone?
Betamethasone is a synthetic glucocorticoid medication that mimics the body’s natural cortisol hormone. It binds to glucocorticoid receptors, suppresses inflammatory gene expression, and reduces immune cell activity. First approved in the 1960s, it quickly became a go‑to drug for conditions ranging from severe eczema to fetal lung maturation.
How do corticosteroids work?
Corticosteroids belong to the broader class of Corticosteroid hormones. They act on the Immune system by turning off pro‑inflammatory cytokines (like IL‑1, TNF‑α) and increasing anti‑inflammatory proteins. The result is less swelling, redness, and pain.
While all corticosteroids share this core mechanism, they vary in three key dimensions:
- Potency - how strong the anti‑inflammatory effect is compared with the reference compound hydrocortisone.
- Duration of action - short‑acting (hours) versus long‑acting (days).
- Formulation - oral tablets, injectables, creams, inhalers, or eye drops.
Comparing Potency: Betamethasone vs. Common Corticosteroids
Below is a snapshot of how betamethasone stacks up against four frequently prescribed steroids.
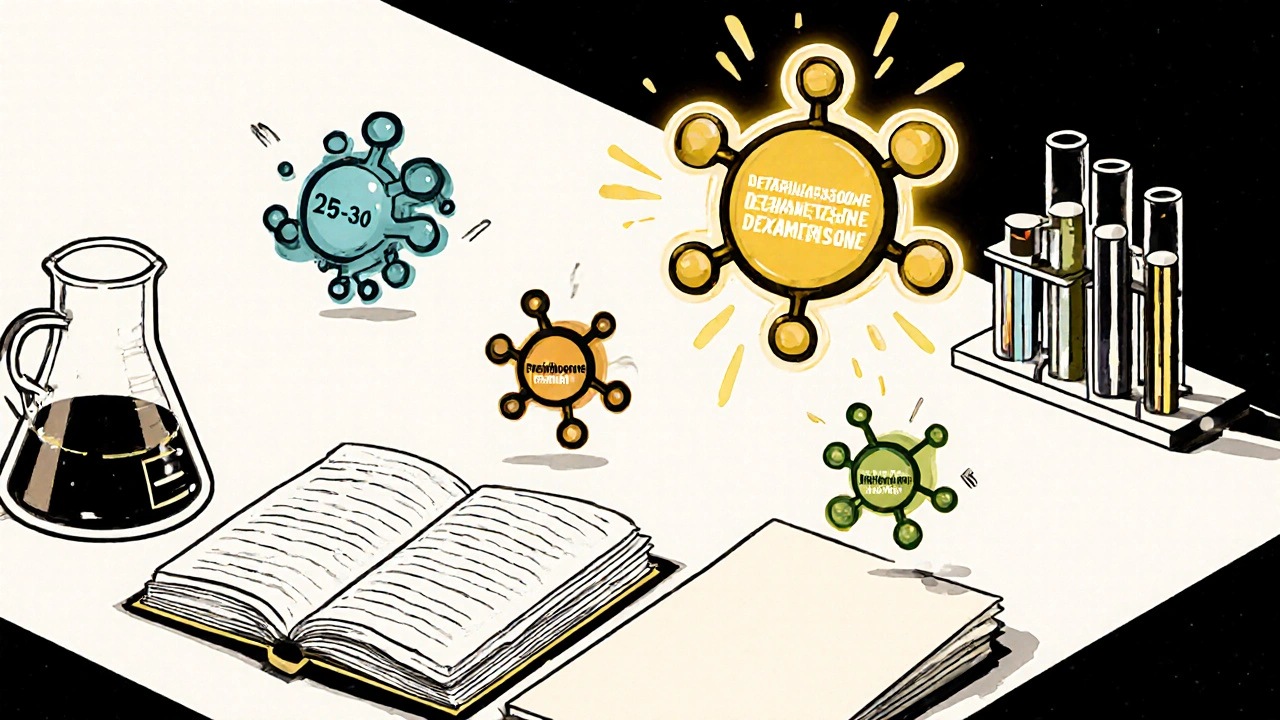
| Drug | Relative Potency* | Duration of Action | Typical Indications | Common Formulations |
|---|---|---|---|---|
| Betamethasone | 25-30× | Long‑acting (24-36 hrs) | Eczema, psoriasis, severe allergic reactions, fetal lung maturation | Topical cream/ointment, IM/IV injection, oral tablet |
| Prednisone | 4-5× | Intermediate (12-24 hrs) | Asthma, rheumatoid arthritis, lupus, COVID‑19 inflammation | Oral tablet, liquid |
| Dexamethasone | 25-30× | Long‑acting (36-48 hrs) | Cerebral edema, chemotherapy‑induced nausea, COVID‑19 severe cases | IV/IM injection, oral tablet, eye drops |
| Hydrocortisone | 1× (reference) | Short‑acting (8-12 hrs) | Adrenal insufficiency, mild dermatitis, allergic reactions | Topical cream, oral tablet, IV infusion |
| Methylprednisolone | 5× | Intermediate (12-24 hrs) | Multiple sclerosis relapse, severe asthma, rheumatic disease | Oral tablet, IV/IM injection |
*Potency is expressed relative to 20 mg of hydrocortisone. Higher numbers mean a stronger anti‑inflammatory effect per milligram.
When to Choose Betamethasone Over Others
Because betamethasone is so potent, it shines in situations where a rapid, dramatic reduction in inflammation is needed. Examples include:
- Severe plaque psoriasis that hasn’t responded to milder steroids.
- Acute dermatologic flare‑ups (e.g., contact dermatitis) requiring short‑term, high‑dose topical therapy.
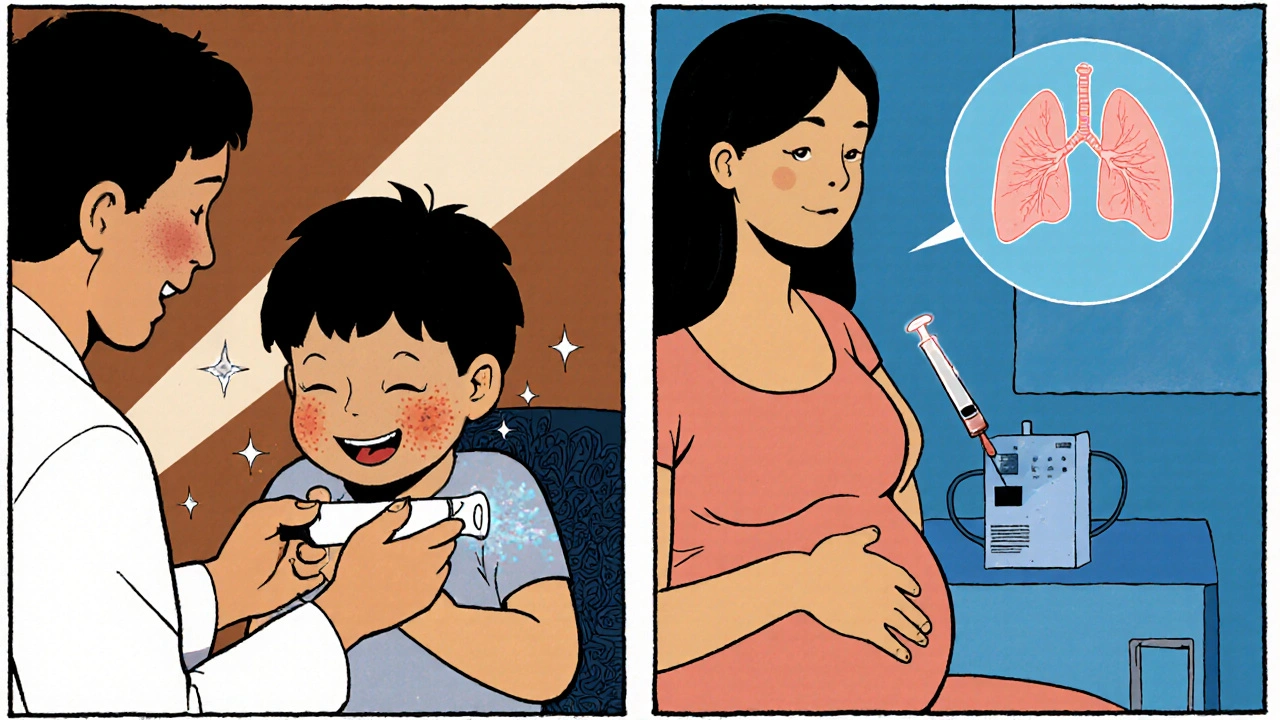
- Fetal lung maturation when preterm birth is imminent - a single dose can dramatically cut neonatal respiratory distress.
Conversely, for chronic low‑grade conditions, a weaker steroid like hydrocortisone or a short‑acting option such as prednisone may be safer, minimizing risks like skin thinning, cataracts, or adrenal suppression.
Formulation Matters: Topical vs. Systemic
Betamethasone is available in several forms, each with distinct absorption profiles.
- Topical creams/ointments (usually 0.05% or 0.1% concentration) stay largely on the skin but can penetrate deeper if applied to thin areas such as the eyelids.
- Intramuscular (IM) or intravenous (IV) injections deliver the drug directly into the bloodstream for systemic effects, useful for severe allergic reactions or autoimmune flare‑ups.
- Oral tablets are rarely used outside of specific obstetric protocols because systemic exposure raises the side‑effect bar.
Other corticosteroids also come in multiple forms, but potency and skin‑penetration differ. For instance, clobetasol propionate (another ultra‑potent topical) is roughly twice as strong as betamethasone cream, making it a better choice for very thick plaques.
Safety Profile: Risks to Watch
All steroids share a common set of potential adverse effects, but the likelihood scales with potency, dose, and treatment length.
| Potency Tier | Local (topical) | Systemic |
|---|---|---|
| Low (e.g., hydrocortisone) | Skin irritation, mild thinning | Rare HPA‑axis suppression |
| Medium (e.g., prednisone, methylprednisolone) | More noticeable thinning, stretch marks | Weight gain, glucose intolerance, mood changes |
| High (betamethasone, dexamethasone) | Severe atrophy, telangiectasia, risk of infection | Osteoporosis, cataracts, adrenal crisis on abrupt stop |
Specific warnings from the FDA include avoiding prolonged use on the face or intertriginous zones, and tapering the dose after more than two weeks of systemic therapy to prevent withdrawal.
Practical Tips for Patients and Clinicians
- Start low, go slow. For skin conditions, begin with a weaker steroid and step up only if needed.
- Limit duration. Topical betamethasone should rarely exceed two weeks on the same site.
- Use the right vehicle. Creams are better for moist areas; ointments work best on dry, scaly plaques.
- Monitor labs. For systemic use, check blood glucose, blood pressure, and bone density every 3-6 months.
- Educate about tapering. If therapy exceeds 14 days, a gradual dose reduction prevents adrenal insufficiency.
Bottom Line: Tailor the Steroid to the Situation
If you need a quick, powerful punch against inflammation and the treatment window is short, betamethasone is often the right tool. When therapy will be long‑term or the inflammation is mild, opting for a lower‑potency corticosteroid reduces the chance of lasting harm.
Frequently Asked Questions
Is betamethasone safe for children?
Yes, but only under strict medical supervision. Pediatric dosing is usually lower, and the treatment period is kept short to avoid growth suppression.
Can I use betamethasone cream on my face?
Generally avoid it. The skin on the face is thin, so a potent steroid can cause noticeable thinning, telangiectasia, and acne. If a facial steroid is required, a milder option like hydrocortisone 1% is preferred.
How does betamethasone differ from dexamethasone?
Both are ultra‑potent and long‑acting, but dexamethasone has a slightly longer half‑life and is more commonly used in neurological swelling and chemotherapy protocols. Betamethasone is favored for dermatologic and obstetric uses.
Do I need to taper off betamethasone after a short course?
If the course was under two weeks and only topical, tapering isn’t usually required. For systemic doses lasting longer than two weeks, a gradual reduction over several days to weeks is advised.
Are there any drug interactions with betamethasone?
Yes. Concurrent use of non‑steroidal anti‑inflammatories (NSAIDs) can increase ulcer risk, and certain antivirals (e.g., ritonavir) may raise steroid levels. Always share your full medication list with your prescriber.











13 Comments
Betamethasone truly shines when you need rapid relief, but it’s important to respect its potency. Its anti‑inflammatory power can calm severe eczema in just a few days, which is a blessing for many patients. However, that same strength can also thin the skin if you leave it on too long. I’ve seen people apply it to their face and end up with noticeable atrophy and telangiectasias. The key is to follow the “start low, go slow” principle that most dermatologists recommend. For systemic use, always have a clear tapering plan in place to avoid adrenal insufficiency. Short courses of topical betamethasone under two weeks usually don’t need a taper, but weekly check‑ins are still wise. If you’re using an oral tablet for fetal lung maturation, the dosing is a one‑time event, so the risk profile changes. Children can tolerate it, but pediatric dosing is lower and you must monitor growth parameters. Patients with diabetes should keep an eye on blood glucose because steroids can push numbers higher. Bone health is another concern for long‑term users; calcium and vitamin D supplementation can help mitigate osteoporosis. When you have a thick plaque psoriasis lesion, consider switching to clobetasol if betamethasone isn’t enough, as it’s even more potent. Conversely, for mild dermatitis, a low‑potency hydrocortisone will usually do the job with fewer side‑effects. Always store the medication at room temperature and keep the tube tightly capped to maintain stability. And remember, open communication with your prescriber is the best way to balance efficacy and safety.
Betamethasone is the alpha‑omega of glucocorticoids-potent, long‑acting, and with a side‑effect profile that screams ‘handle with care’ 😂. The pharmacokinetic half‑life dwarfs prednisone, making it the go‑to for acute flares, but you’ll also see HPA‑axis suppression quicker. If you can’t manage the risk, stick to hydrocortisone and quit the drama.
Betamethasone offers rapid control for severe inflammation, yet its potency demands careful monitoring; a brief course often suffices.
They don’t want you to know how powerful betamethasone really is; it’s the secret weapon hidden in every pharmacy. The pharma giants push milder steroids so they can sell more of the expensive version. Use it wisely, or you’ll be a pawn in their game.
Only real American doctors would trust betamethasone over foreign knock‑offs.
Ah, the nuanced dance of corticosteroid selection-one could craft an entire dissertation on relative receptor affinity, yet most clinicians reduce the conversation to a spreadsheet of potency numbers. By overlooking pharmacodynamics, they betray the very science they claim to uphold. Betamethasone’s long‑acting nature is lauded, but the same half‑life that provides convenience also prolongs systemic exposure, a fact conveniently omitted in promotional material. One must therefore interrogate the data sources, question the bias of industry‑funded trials, and remember that a “one‑size‑fits‑all” approach is simply a marketing ploy masquerading as clinical guidance.
Everyone’s raving about betamethasone’s potency, but the hype ignores the long‑term skin damage it can cause. I’d rather see a patient on a low‑dose regimen that manages symptoms without sacrificing tissue integrity.
It baffles me how some prescribe betamethasone without considering the ethical responsibility to minimize harm. The medical community should champion patient safety over quick fixes, especially when less potent alternatives exist.
For a patient with acute eczema on the elbows, start with a low‑potency steroid and only step up to betamethasone if there’s no improvement after a week. Keep the treatment area limited and monitor for skin thinning; a follow‑up visit in two weeks lets you reassess the need for stronger therapy.
You’ve got this! If you’re battling a flare, a short burst of betamethasone can be a game‑changer-just remember to taper off and give your skin a break. Celebrate the small victories of reduced redness and itching!
Betamethasone, while highly effective, requires diligent monitoring; please ensure regular blood work, skin assessments, and patient education!!! Ignoring these steps can lead to severe adverse events, such as adrenal crisis-an outcome no practitioner wants!!!
The article covers the basics well, yet it glosses over the cost implications of high‑potency steroids and the healthcare disparities they may exacerbate. A deeper dive into insurance coverage and patient access would strengthen the piece.
i think betamethasone is good but i also mind the side effects like sugar level rise and bone loss, so careful use is must.