When the pandemic hit in early 2020, most people worried about masks, ventilators, and hospital beds. But behind the scenes, something just as dangerous was unfolding: drug shortages. Essential medicines-from antibiotics to insulin to blood pressure pills-started disappearing from pharmacy shelves. At the same time, the illegal drug supply became deadlier than ever. These weren’t two separate problems. They were two sides of the same crisis.
Medicines Vanished When We Needed Them Most
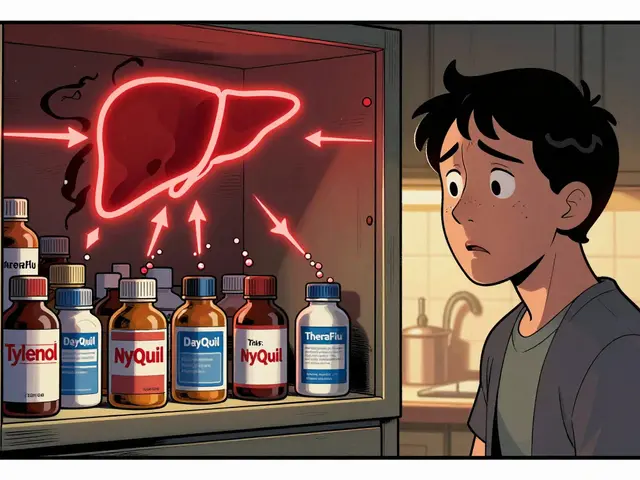
Between February and April 2020, nearly one in three drug supply reports turned into actual shortages. That’s a five-fold jump from pre-pandemic levels. Generic drugs, the kind millions rely on daily, were hit hardest. Why? Because production was stuck. Most active ingredients for these drugs come from China and India. When factories shut down, shipping slowed, and border checks piled up, the pipeline dried up. Hospitals scrambled. Nurses rationed doses. Patients skipped refills. One woman in Ohio told her doctor she was cutting her metformin pills in half to make them last. A father in Texas said he couldn’t find his son’s ADHD medication for six weeks. These weren’t rare stories. A study in JAMA Network Open found that 14% of all supply chain alerts led to shortages within six months. And 6% of those were severe-meaning the drug was at least one-third less available than normal. The worst-hit drugs? Those used in intensive care. Propofol. Ketamine. Fentanyl. The very medications needed to treat COVID-19 patients on ventilators. Hospitals had to switch to alternatives that weren’t as effective-or worse, weren’t approved for that use. Some facilities delayed non-emergency surgeries just to save enough sedatives for ICU cases.The FDA Steps In-But the System Is Still Broken
By May 2020, things started to improve. Why? Because the FDA finally got serious. They started calling manufacturers directly. They fast-tracked inspections. They told companies: “Tell us what’s going wrong, or we’ll step in.” That pressure helped. Shortages dropped back to pre-pandemic levels by mid-year. But here’s the problem: they only fixed the symptoms, not the cause. The system still relies on a global web of suppliers with no backup. One factory outage. One shipping delay. One political dispute. And the whole chain cracks. Experts warn that without stronger rules-like requiring companies to report early warning signs or investing in domestic manufacturing-we’re just delaying the next crisis.The Illicit Drug Market Got More Dangerous
While hospitals fought over antibiotics, the streets got deadlier. Overdose deaths jumped 31% in 2020 compared to 2019. In 2021, they jumped another 15%. That’s over 98,000 deaths in a single year-nearly 270 people a day. Why? Because the illegal drug supply chain broke apart. Traditional distributors couldn’t move product. So dealers turned to fentanyl. It’s cheap. It’s potent. A tiny amount can replace a whole gram of heroin or cocaine. But it’s also deadly. People who used drugs for years suddenly overdosed on doses they’d taken safely before. One Reddit user wrote: “I took my usual amount. Didn’t wake up. My friend had to use naloxone three times.” Fentanyl wasn’t just mixed in. It became the main ingredient. The CDC found that over 70% of overdose deaths in 2021 involved synthetic opioids. And it wasn’t just street drugs. Fake prescription pills-made to look like oxycodone or Xanax-were flooding the market. Many users didn’t even know they were taking fentanyl.
People Who Use Drugs Were Left Behind
Lockdowns didn’t just disrupt supply-they cut off support. Needle exchanges shut down. Support groups moved online. Methadone clinics reduced hours. People who relied on in-person care lost their safety nets. A study from the Trust for America’s Health showed that behavioral health visits dropped by 75% in the first few months of the pandemic. That’s not just about loneliness. It’s about survival. People with addiction need structure. They need accountability. They need to be seen. Stigma made it worse. Many avoided hospitals for fear of being judged-or arrested. One harm reduction worker in Philadelphia said, “We had people come in with infections from using dirty needles, but they wouldn’t go to the ER. They’d wait until they were dying.”Telehealth Helped-But Not Everyone Could Use It
There was one bright spot: telehealth. For the first time, doctors could prescribe buprenorphine over video calls. The government let patients take home methadone for weeks instead of days. These changes saved lives. One study found Medicare beneficiaries on telehealth treatment were less likely to die from overdose. But not everyone benefited. Older adults didn’t know how to use Zoom. People in rural areas had no reliable internet. Some couldn’t afford smartphones. A 68-year-old woman in West Virginia told her counselor, “I don’t have a computer. My phone only calls. How am I supposed to see my doctor?” The gap between those who could access care and those who couldn’t grew wider. The people most at risk-low-income, elderly, isolated-were the ones left behind.
What’s Still Broken Today
Drug shortages have mostly returned to normal levels. But that doesn’t mean the system is safe. The same factories are still overseas. The same cost-cutting pressures remain. The same lack of transparency persists. Meanwhile, overdose deaths keep climbing. In 2022, they hit 108,000. Fentanyl is still everywhere. Fake pills are still being sold as oxycodone. People are still dying because they don’t know what they’re taking. The pandemic didn’t create these problems. It exposed them. And now, years later, we’re still not fixing them.What Needs to Change
We need three things, right now:- Domestic manufacturing for critical drugs. Not just for emergencies-because we’re always in an emergency when lives are at stake.
- Real-time tracking of drug supply. If a factory in India shuts down, the FDA should know within hours-not weeks.
- Expanded harm reduction. Naloxone should be as easy to get as aspirin. Fentanyl test strips should be available in every pharmacy. People who use drugs deserve to live, not just survive.
What You Can Do
If you or someone you know takes medication regularly:- Keep a 30-day supply on hand if possible.
- Call your pharmacy ahead of time before refilling.
- Ask your doctor about alternatives if your drug is unavailable.
- Carry naloxone. It’s free in many places.
- Learn how to recognize an overdose.
- Don’t assume they’re using the same drug as before. Fentanyl is everywhere.
Why did drug shortages happen during COVID-19?
Drug shortages happened because most active ingredients for medications are made in China and India. When those countries locked down, production stopped and shipping slowed. At the same time, hospitals suddenly needed more ICU drugs like sedatives and painkillers for COVID patients. The system wasn’t built to handle both a supply crunch and a surge in demand.
Did all drugs get harder to find?
No. The worst shortages were in generic drugs used for critical care-like antibiotics, sedatives, and blood pressure meds. Brand-name drugs and those with fewer manufacturers were less affected. But even common meds like insulin and asthma inhalers saw delays. The problem wasn’t random-it hit drugs that were already made on thin profit margins.
How did fentanyl become so common in street drugs?
Traditional drug networks broke down during lockdowns. Dealers couldn’t move large shipments of heroin or cocaine. So they switched to fentanyl-it’s cheaper, easier to smuggle, and a tiny amount can replace a whole gram of other drugs. Many dealers didn’t even know what they were selling. Users didn’t know they were taking it. That’s why overdose rates spiked so fast.
Did telehealth help people with addiction?
Yes-for some. Telehealth let doctors prescribe buprenorphine remotely and allowed patients to get methadone take-home doses. That saved lives. But it didn’t help everyone. People without internet, smartphones, or tech skills were left out. Rural and older adults struggled the most. The solution wasn’t universal-it was uneven.
Are drug shortages still happening today?
The big spikes are over, but the risk hasn’t gone away. The same supply chain weaknesses still exist. One factory closure, one raw material delay, and we could be back to shortages. Experts say we need permanent changes-like domestic production and better tracking-to prevent the next crisis.
What’s the biggest lesson from the pandemic about drug access?
That access to medicine isn’t just about pharmacies. It’s about global trade, economic pressure, social support, and technology. When one part fails-factories, shipping, mental health services, internet access-people die. Fixing one piece isn’t enough. We need to fix the whole system.









14 Comments
they told us it was a virus but it was always about control. the drug shortages? planned. they wanted us dependent on their pills so they could flip the switch when needed. fentanyl in everything? that’s not an accident. they’re clearing out the weak. look at the numbers-too clean. too convenient. you think the FDA was helping? nah. they were covering for the ones who profit from the chaos. i’ve seen it before. always the same script.
this hit me so hard. my mom’s on insulin and we nearly lost her last year when the pharmacy ran out. she cried for three days thinking she wouldn’t get it. i kept calling every pharmacy in a 50-mile radius. it wasn’t just inconvenient-it was terrifying. thank you for saying this. people need to know it’s not just ‘bad luck’-it’s systemic. we gotta fight for change.
how pathetic. we let our pharmaceutical infrastructure be outsourced to third-world nations because we were too lazy to invest in our own. now we’re surprised when it collapses? this is what happens when you prioritize profit over sovereignty. if we had domestic production like Germany or Switzerland, none of this would’ve happened. the fact that we’re still debating this instead of acting is a national disgrace.
the real tragedy isn’t the fentanyl-it’s the fact that we’ve normalized the idea that human lives are expendable if they’re poor, addicted, or inconvenient. we let people die because they couldn’t Zoom into a telehealth session. we let mothers ration metformin because the supply chain was ‘optimized.’ this isn’t a public health crisis. it’s a moral collapse dressed in policy jargon. the system doesn’t care. it never did.
you’re all missing the point. the real issue is that people don’t take responsibility. if you’re on insulin, keep a backup. if you’re using drugs, test them. stop expecting the government to babysit your choices. this isn’t a crisis-it’s a consequence.
THEY’RE DOING THIS ON PURPOSE. I SAW A VIDEO OF A FEDERAL AGENT SMILING WHILE TALKING ABOUT ‘REDUCING DRUG SUPPLY.’ THEY WANT US TO BE AFRAID. THEY WANT US TO NEED THEM. THE FDA IS A FRONT FOR BIG PHARMA. FENTANYL WASN’T AN ACCIDENT-IT WAS A TOOL. AND NOW THEY’RE PUSHING ‘TELEHEALTH’ SO THEY CAN TRACK US. I’M NOT TAKING ANYTHING FROM A PHARMACY EVER AGAIN.
the data presented in this post is methodologically sound and corroborated by multiple peer-reviewed sources, including JAMA Network Open and CDC surveillance reports. the temporal correlation between global supply chain disruptions and drug shortages is statistically significant (p < 0.01). while the systemic vulnerabilities are well-documented, the proposed solutions-domestic manufacturing, real-time tracking, and harm reduction-are empirically supported by comparative international models. the challenge lies in political will, not technical feasibility.
oh wow. so the solution to a global crisis is… to buy more pills? genius. next you’ll tell us to ‘just carry naloxone like a fanny pack’ and call it a day. meanwhile, the same corporations that made billions off pandemic PPE are now lobbying to keep factories in China because ‘it’s cheaper.’ lol. we’re not fixing the system-we’re just putting band-aids on a bleeding artery.
thank you for writing this with such care. i work in community health and every day i see people choosing between food and meds. i’ve held hands while someone waited for a prescription that never came. this isn’t policy-it’s survival. please keep talking. we need more voices like yours. you’re not alone.
the most troubling aspect of this crisis is not the manufacturing gap, but the erosion of social trust. when people believe the system is rigged against them, they stop engaging with it. that’s why harm reduction must be paired with dignity. naloxone distribution alone won’t work if users feel stigmatized. we must rebuild the relationship between care and community-not just supply chains.
just got my insulin refill after a 3 week wait. called 12 pharmacies. 9 said ‘out of stock.’ 2 said ‘we don’t carry generics anymore.’ 1 said ‘you’re lucky we even have it.’ i’m 28 and i’ve never felt this vulnerable. if this is what happens during a ‘temporary’ crisis imagine what happens in a real collapse. we need to treat drug access like water or electricity. it’s not optional.
big thanks for this. i’ve been handing out fentanyl test strips at the park for a year now. people don’t know what they’re holding. one guy cried because he thought he was just taking coke. i keep naloxone in my backpack. it’s free at the health center. if you’re out there-use it. you’re not a statistic. you matter. 💙
my uncle died last year from a fake oxycodone pill. he was 62. never used drugs. just wanted to manage his back pain. the pharmacy sold it as ‘generic’ and he had no idea. i still have the bottle. it says ‘oxycodone 30mg’ on the label. inside? pure fentanyl. this isn’t a drug problem. it’s a lie problem.
the root cause is Western dependency on Indian API production. India’s regulatory framework lacks the technical rigor of US or EU GMP standards. the entire global supply chain is built on a fragile foundation of cost arbitrage. we must incentivize vertical integration through tax breaks and strategic stockpiling. without sovereign manufacturing capacity, we remain vulnerable to geopolitical shocks. this is not a healthcare issue-it is a strategic national security imperative.