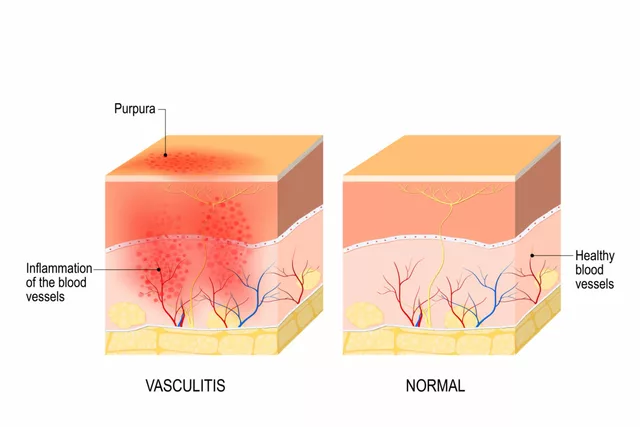
When your skin is red, itchy, and flaring up despite moisturizers and over-the-counter creams, you might wonder if a stronger option like methylprednisolone could help. It’s not a first-line fix, but for severe cases of dermatitis-especially when other treatments fail-it’s a tool doctors turn to. The question isn’t whether it works, but when, how, and at what cost.
What Is Methylprednisolone?
Methylprednisolone is a synthetic corticosteroid, part of the same family as prednisone and hydrocortisone. It works by calming down the immune system’s overreaction that causes inflammation in conditions like atopic dermatitis, contact dermatitis, and seborrheic dermatitis. Unlike topical creams you slap on, methylprednisolone is usually taken orally as a tablet or given as an injection, making it a systemic treatment. That means it affects your whole body, not just the patch of skin that’s angry.
It’s not a cure. It doesn’t fix the root cause-whether that’s genetics, allergens, or environmental triggers. But it shuts down the inflammation fast. In clinical trials, patients with moderate to severe atopic dermatitis saw significant improvement in itching and redness within 48 to 72 hours of starting oral methylprednisolone. One 2023 study in the Journal of the American Academy of Dermatology found that 78% of patients had at least a 50% reduction in EASI (Eczema Area and Severity Index) scores after seven days of treatment.
When Is It Used for Dermatitis?
Doctors don’t hand out methylprednisolone like candy. It’s reserved for flare-ups that are:
- Widespread-covering large areas of the body, not just a small patch
- Resistant to topical steroids, calcineurin inhibitors, or phototherapy
- Causing severe discomfort, sleep loss, or signs of infection from scratching
- Interfering with daily life-school, work, or social activities
For example, someone with chronic hand eczema that won’t respond to twice-daily clobetasol might get a short 5-day course of methylprednisolone to reset the inflammation. Or a child with a sudden, severe flare after exposure to poison ivy might get a single dose to stop the swelling before it spreads.
It’s rarely used for mild or localized cases. If a cream works, you stick with it. Oral steroids like methylprednisolone come with risks that outweigh the benefits for small, manageable flare-ups.
How Is It Dosed?
Dosing depends on body weight, severity, and patient age. For adults, a typical starting dose is 16 to 48 mg per day, taken as a single morning dose to mimic the body’s natural cortisol rhythm. For kids, it’s usually 0.3 to 0.6 mg per kg of body weight, capped at 40 mg daily.
The course is always short-usually 5 to 14 days. No one takes methylprednisolone for months unless they have a life-threatening autoimmune condition. Dermatitis flare-ups are temporary, so treatment is temporary too.
Doctors often use a tapering schedule. For instance, you might take 40 mg on day one, 32 mg on day two, then drop by 8 mg every two days until you’re off. This helps prevent rebound flares and reduces the risk of adrenal suppression.

How Fast Does It Work?
People often notice relief within 24 to 48 hours. Itching usually drops first-sometimes dramatically. Redness and swelling follow. In one case study from a Perth dermatology clinic in early 2025, a 34-year-old woman with widespread nummular eczema went from scratching all night to sleeping through the night after just two days on 24 mg of methylprednisolone.
But here’s the catch: it doesn’t last. Once you stop, the inflammation can come back, sometimes worse than before. That’s why tapering and follow-up care matter. After the steroid course, most patients are switched back to topical treatments, moisturizers, and trigger avoidance.
Side Effects and Risks
Short-term use is generally safe for healthy adults, but it’s not harmless. Common side effects include:
- Increased appetite and weight gain
- Mood swings or trouble sleeping
- Higher blood sugar (especially risky for diabetics)
- Upset stomach or nausea
- Fluid retention and swelling in the ankles
Longer use-even beyond two weeks-can lead to more serious issues like osteoporosis, cataracts, high blood pressure, and weakened immune response. That’s why it’s never prescribed for ongoing maintenance.
People with certain conditions should avoid it: active infections (like chickenpox or TB), uncontrolled diabetes, glaucoma, or a history of peptic ulcers. Pregnant women should only use it if benefits clearly outweigh risks, and even then, at the lowest possible dose.
Alternatives to Methylprednisolone
There are other options, especially as newer treatments become available:
- Topical calcineurin inhibitors (tacrolimus, pimecrolimus): Good for sensitive areas like the face and neck. No steroid side effects.
- Phosphodiesterase-4 inhibitors (crisaborole): A non-steroid ointment for mild to moderate eczema.
- Biologics (dupilumab, tralokinumab): Injected monthly for moderate to severe atopic dermatitis. They target specific parts of the immune system and are safe for long-term use.
- JAK inhibitors (upadacitinib, abrocitinib): Oral pills that block inflammation pathways. Used when biologics don’t work.
Biologics and JAK inhibitors are now preferred for chronic cases because they’re targeted, safer long-term, and don’t cause systemic side effects. But they’re expensive and require a specialist referral. Methylprednisolone still has a place for quick, affordable relief while waiting for those treatments to kick in.

What Happens After Stopping?
Stopping methylprednisolone is where many people slip up. You feel better, so you stop early-or skip the taper. Then the rash comes roaring back. This is called rebound dermatitis.
To prevent it, doctors pair the steroid course with a solid aftercare plan:
- Start or increase moisturizing-use fragrance-free emollients at least twice daily.
- Return to topical steroids if needed, but at lower strength (e.g., hydrocortisone 1% instead of clobetasol).
- Identify and avoid triggers: harsh soaps, wool, stress, sweat, certain foods if allergies are suspected.
- Consider wet wrap therapy for stubborn patches.
- Follow up with a dermatologist within 2 weeks to adjust your long-term plan.
Without this plan, you might end up cycling back to steroids again and again. That’s a dangerous path.
Real-World Use in Australia
In Australia, methylprednisolone is listed on the Pharmaceutical Benefits Scheme (PBS), so it’s affordable for most patients with a prescription. But GPs are cautious. Many now refer patients to dermatologists sooner rather than later, especially for persistent cases. Public hospitals in Perth and Brisbane report a 20% drop in oral steroid prescriptions for dermatitis over the last two years-largely because biologics are now more accessible under Medicare.
Still, methylprednisolone remains a go-to for emergency flare-ups. One GP in Fremantle told me last month: “I’ll give it for a week if someone’s skin is splitting open and they can’t work. But then I hand them off to the skin clinic. It’s a bridge, not a home.”
Bottom Line: When It Helps-and When It Doesn’t
Methylprednisolone works fast. It’s powerful. It can give you back your sleep, your confidence, your ability to live normally during a bad flare. But it’s not a long-term solution. It’s a reset button, not a new normal.
If your dermatitis is mild, stick with moisturizers and topical treatments. If it’s chronic and worsening, talk to a dermatologist about biologics or JAK inhibitors. Use methylprednisolone only when:
- The flare is severe and widespread
- Other treatments have failed
- You need fast relief to get through a critical period
- You’re under medical supervision with a clear exit plan
Don’t self-prescribe. Don’t borrow pills from someone else. Don’t stretch the course. It’s not worth the risk.
Can methylprednisolone cure dermatitis?
No, methylprednisolone does not cure dermatitis. It only reduces inflammation and symptoms temporarily. Dermatitis is a chronic condition often linked to genetics, immune dysfunction, or environmental triggers. Once you stop taking methylprednisolone, the underlying cause remains, and symptoms can return. Long-term management requires trigger avoidance, moisturizing, and often non-steroid treatments like biologics or topical calcineurin inhibitors.
How long does it take for methylprednisolone to work on skin inflammation?
Most people notice reduced itching within 24 to 48 hours. Redness and swelling usually improve noticeably by day 3 to 5. The fastest relief comes from oral tablets or injections-not topical creams. For severe flares, this speed is critical to prevent sleep loss, infection from scratching, or disruption to daily life.
Is methylprednisolone better than prednisone for dermatitis?
Methylprednisolone and prednisone are very similar in strength and use. Methylprednisolone is slightly more potent by weight-about 20% stronger. For example, 4 mg of methylprednisolone equals roughly 5 mg of prednisone. Both are used interchangeably for dermatitis. The choice often comes down to availability, cost, and doctor preference. Neither has a clear advantage in effectiveness for skin inflammation.
Can I use methylprednisolone with topical steroids?
Yes, but only under medical supervision. Oral methylprednisolone is used for systemic inflammation, while topical steroids target local areas. Using both together can increase the risk of side effects like skin thinning or adrenal suppression. Doctors may prescribe them together during a severe flare, but they’ll taper the oral dose first and keep topical use minimal and short-term.
What happens if I stop methylprednisolone too soon?
Stopping too early can cause a rebound flare-where the dermatitis comes back worse than before. This happens because the body hasn’t had time to restart its own cortisol production. Always follow your doctor’s tapering schedule. If you stop early because you feel better, talk to your doctor first. They may adjust your plan or extend the taper to prevent this.
Is methylprednisolone safe for children with eczema?
It can be, but only for short-term, severe flares and under strict supervision. Pediatric doses are based on weight, and treatment rarely lasts more than 7 to 10 days. Long-term use in children can affect growth and bone development. Most pediatric dermatologists prefer topical treatments or biologics like dupilumab for kids over 6 months old, reserving oral steroids for emergencies.
Can methylprednisolone cause skin thinning?
Oral methylprednisolone does not directly cause skin thinning like long-term use of strong topical steroids can. However, systemic corticosteroids can make skin more fragile overall, increasing bruising and slowing wound healing. This is a systemic effect, not localized. If you notice easy bruising or slow-healing cuts while on methylprednisolone, tell your doctor.





15 Comments
I was on methylprednisolone last winter for a brutal eczema flare-my hands were cracking and bleeding. Within 36 hours, the itching stopped like someone flipped a switch. I cried because I hadn’t slept through the night in weeks. It’s not magic, but it’s a lifesaver when you’re drowning in inflammation. Just don’t skip the taper. I did, and yeah, it came back worse. Lesson learned.
So many people think steroids are the enemy, but they’re just tools. Like a fire extinguisher-you don’t keep it on the wall forever, but when the house is burning, you grab it. Methylprednisolone is that extinguisher for severe dermatitis. The real win is using it to buy time so you can get to the real long-term solutions-biologics, trigger tracking, moisturizing rituals. Don’t fear the pill. Fear the cycle.
Okay so i just wanted to say that i had this same issue like last year and i was on methylprednisolone for like 10 days and it was a game changer honestly like i was scratching so bad i had scabs on my arms and legs and after the first day i could actually touch my clothes without crying and by day 3 i was sleeping like a baby like i forgot what silence felt like and yeah i know it’s not a cure but sometimes you just need a reset button you know? and also dont forget to drink water like a lot because i got super bloated and my ankles looked like balloons lol
How quaint. You’re all treating this like some kind of miracle drug. Methylprednisolone is a blunt instrument-like using a sledgehammer to fix a quartz clock. The real problem isn’t the inflammation; it’s the medical system’s lazy reliance on palliatives instead of root-cause diagnostics. Why not investigate gut microbiome imbalances, heavy metal toxicity, or even electromagnetic hypersensitivity? No, let’s just pump the patient full of synthetic cortisol and call it a day. Pathetic.
There’s something almost poetic about corticosteroids-how they silence the body’s scream so quietly. You take a pill, and the storm inside your skin just… stops. For a moment, you remember what peace feels like. But then the silence becomes a ghost. The inflammation doesn’t vanish-it waits. And when it returns, it doesn’t knock. It kicks the door down. That’s the tragedy: we’re not curing anything. We’re just buying ourselves more time to face the truth-that our skin is a mirror, and the world we live in is breaking us.
Don’t forget: always take it with food. Always. I once took it on an empty stomach-big mistake. Stomach cramps, nausea, felt like I’d swallowed a cactus. Also, hydration is non-negotiable. And sleep? You’re gonna be wired. Don’t drink caffeine after noon. And please, for the love of all that’s holy, don’t stop early. Taper. Taper. Taper. Your adrenal glands will thank you. And your dermatologist. And your future self.
Everyone’s acting like this is some revolutionary breakthrough when it’s just another band-aid on a bullet wound. You think you’re fixing your skin? You’re just delaying the inevitable collapse of your immune system. And don’t even get me started on the biologics-they’re $20,000 a year and still don’t work for half the people. This whole system is a scam. You’re being sold a temporary fix while the real causes-pollution, processed food, stress-are ignored. Wake up.
I’ve had atopic dermatitis since I was 4. I’m 38 now. I’ve tried everything. Methylprednisolone? It worked. But what worked better was learning to sit with the itch. Not scratching. Not fighting. Just… being with it. The pill gave me space to do that. It didn’t cure me, but it gave me back the quiet I needed to heal in a different way. Sometimes the medicine isn’t the drug. It’s the pause it gives you.
Y’all are making this way too complicated. If your skin is on fire and you can’t sleep? Take the pill. If you’re not getting better with creams? Ask for the pill. If you’re embarrassed to leave the house? The pill helps. It’s not perfect. It’s not forever. But it’s not evil either. Just use it smart. Moisturize like your life depends on it. Avoid stress. And don’t be ashamed to need help. You’re not weak-you’re human.
You think you’re alone? I’ve been on this ride for 12 years. I’ve cried in dermatology waiting rooms. I’ve slept with ice packs on my arms. I’ve begged my mom to stop me from scratching. And yes-I took methylprednisolone. And yes-it saved me. But here’s the truth no one tells you: the real battle isn’t the rash. It’s the loneliness. The shame. The way people look at you like you’re contagious. The pill doesn’t fix that. But maybe… just maybe… if you survive the flare, you learn to speak up. And that’s the real cure.
Just wanted to say-this post is so helpful. I’ve been scared to ask my doctor about oral steroids because I thought they were ‘bad.’ But reading this? It made me feel like it’s okay to need help. I’ve got a flare right now and I’m going to book an appt tomorrow. No more guilt. No more waiting. My skin deserves relief. And so do I. 💪✨
Canada has better access to biologics than the U.S., and we’re still overprescribing steroids. The fact that you’re even asking this question means you’re not being referred to a specialist early enough. Methylprednisolone is a band-aid for a broken healthcare system. If you’re in the U.S., you’re getting nickel-and-dimed until you’re desperate. Then they hand you the steroid like it’s a reward for suffering long enough. It’s not medicine-it’s damage control.
Oh look, another American who thinks steroids are the answer. In Europe, we treat the root causes-diet, gut health, even psychological trauma. Here? You get a pill and a pat on the head. You think your skin’s the problem? It’s your diet. It’s your stress. It’s your over-sanitized, chemical-filled life. Methylprednisolone? It’s just another way to keep you docile while the real issues fester. You’re being sold a lie.
Did you know methylprednisolone is linked to 5G radiation exposure? 🤔 The pharmaceutical industry uses it to mask symptoms so we don’t notice the real problem: corporate surveillance in our skin cells. Also, the FDA banned it in 1998 but it’s still sold under ‘special dispensation’… and the moon landing was fake. Just saying. 🌕💉 #WakeUp
Methylprednisolone works. End of story. Stop overthinking it. If you need it, take it. If you don’t, don’t. Stop pretending it’s a moral dilemma. It’s a tool. Use it or don’t. But don’t turn a medical decision into a philosophy seminar.