Every time you pick up a prescription, there’s a label that could save your life-or hurt you if you ignore it. It’s not just about how many pills to take or when. The real danger often hides in the fine print: drug interactions. These happen when your medication reacts badly with another drug, supplement, or even food. The result? Too much bleeding, a heart attack, or a medicine that stops working. In the U.S., over 2 million adverse drug events happen every year because of these interactions. About 100,000 of them land people in the hospital. And most of them? Totally preventable.
What’s on Your Prescription Label (And Where to Look)
Your prescription label isn’t random text. It’s built to strict federal rules. The FDA requires every label to have clear sections. The two most important ones for avoiding interactions are Warnings and Precautions (Section 5) and Drug Interactions (Section 7).
Section 5 is where the serious stuff lives. If your medicine can cause life-threatening reactions when mixed with another drug, it’s here. Phrases like “Avoid concomitant use with [Drug X]” or “May increase risk of bleeding” are red flags. These aren’t suggestions-they’re warnings you can’t afford to skip.
Section 7 is the full list. It’s longer, more detailed. It tells you what happens when you mix your drug with others, including over-the-counter painkillers, herbal supplements, or even grapefruit juice. You’ll see things like “Reduce dosage when used with [Drug Y]” or “Monitor for dizziness or low blood pressure.” This section doesn’t just say there’s a problem-it tells you exactly what to do about it.
Don’t forget OTC meds. Even if it’s just ibuprofen or allergy pills, the “Warnings” section on those bottles matters too. A 2023 study found 98% of common over-the-counter drugs list interaction risks-but only 57% of people actually read them.
What the Labels Don’t Tell You (And Why It Matters)
Here’s the uncomfortable truth: your prescription label won’t mention everything. It won’t list every supplement you take. And it definitely won’t warn you about the ginkgo biloba you started last month for memory, or the St. John’s wort for anxiety.
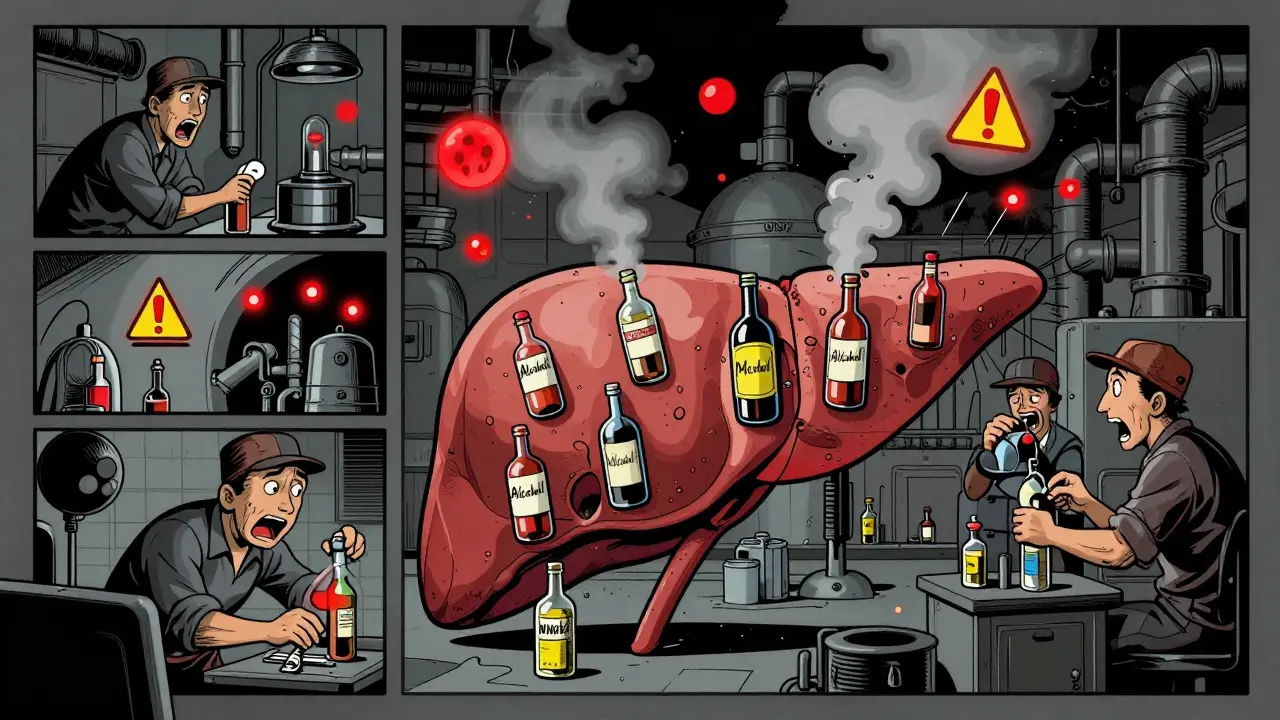
That’s a problem. Studies show herbal supplements cause 32% of serious drug interactions, yet they’re only mentioned in 17% of prescription labels. A patient on warfarin (a blood thinner) who also takes ginkgo biloba has a 5x higher risk of dangerous bleeding. But if they didn’t tell their doctor or pharmacist, the label won’t say a word.
Same goes for vitamins. High-dose vitamin K can make blood thinners useless. Calcium supplements can block antibiotics. Even magnesium can interfere with thyroid meds. These aren’t rare. They’re common-and silent.
That’s why you need to build your own list. Write down every pill, capsule, gummy, tea, or tincture you take. Include the dose and why you take it. Bring that list to every doctor’s visit and every pharmacy pickup. It’s the only way to fill the gaps the label leaves behind.
How to Actually Understand the Warnings
Let’s be honest: prescription labels are written for doctors, not patients. Words like “concomitant use,” “pharmacokinetic interaction,” or “CYP450 enzyme inhibition” sound like a foreign language. And that’s by design. But you don’t need to be a pharmacist to get the message.
Look for these three simple phrases:
- Avoid use with - means don’t mix them. Period.
- Monitor for - means watch for symptoms like dizziness, nausea, rash, or unusual bruising. Call your doctor if they happen.
- Reduce dosage - means you might need less of one or both drugs. Don’t change your dose yourself. Talk to your pharmacist first.
On Reddit’s r/Pharmacy, 78% of people said they ignored warnings because they didn’t understand them. One user wrote: “I saw ‘concomitant use’ and thought it meant ‘use together sometimes.’ I didn’t realize it meant ‘never.’” That’s the kind of mistake that ends in the ER.
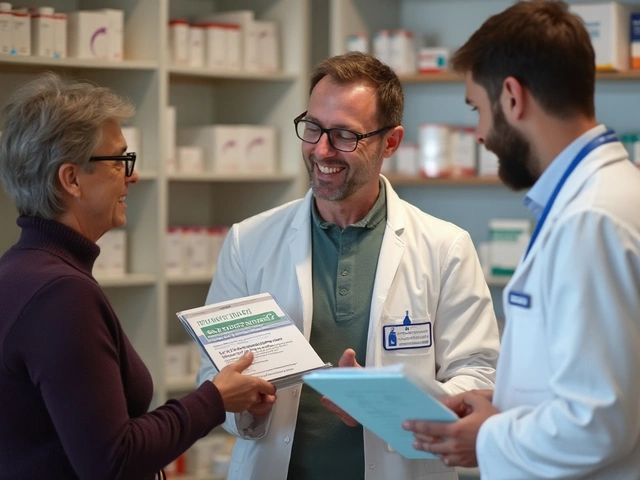
Here’s a trick: read the label out loud. If you can’t explain it in plain English, you don’t understand it. Ask your pharmacist to explain it to you. Don’t be embarrassed. They’ve seen it all. And they’re trained to translate medical jargon into something you can live with.

What to Do When You Pick Up Your Prescription
Don’t just grab your bottle and leave. Take five minutes. Do this:
- Check the label against your personal medication list. Is this new drug on there? Did you forget to mention a supplement?
- Look for the “Drug Interactions” section. Circle any drugs you’re already taking that show up.
- Ask: “Is there anything here I shouldn’t mix with my other meds?”
- Ask: “What symptoms should I watch for if something goes wrong?”
- Ask: “Can you write down the reason I’m taking this?”
That last one? It’s a game-changer. Harvard Medical School found that 12% of medication mix-ups happen because people confuse similar-sounding drugs-like Klonopin (for seizures) and clonidine (for blood pressure). Write “for anxiety” or “for high BP” right on the bottle with a Sharpie. It saves lives.
And if you’re on five or more medications? Bring all your bottles to the pharmacy. A 2023 study of 10,000 pharmacy visits found that 22% of patients had dangerous interactions that weren’t caught until the pharmacist saw all the meds together.
Tools That Help (And the Ones That Don’t)
There are apps like Drugs.com Drug Interactions Checker. They’re useful. They process over a million queries a month and catch 89% of interactions. But they’re not perfect. They only cover 92% of prescription drugs. And they don’t know your history. They don’t know if you’re 80 and have kidney disease. They don’t know if you’ve had a bleed before.
Prescription labels? They’re the only source legally required to be accurate for your specific drug. The FDA mandates that manufacturers validate every interaction warning. Apps? They’re crowdsourced. Sometimes they’re right. Sometimes they’re outdated. Always cross-check with your label.
But here’s the best tool: your pharmacist. Use the “Ask a Pharmacist” feature on Drugs.com or walk into your local pharmacy. People who use it report 83% better understanding of their meds. Pharmacists don’t just fill prescriptions-they’re your safety net.

Special Cases: Kids, Seniors, and Multiple Meds
If you’re giving medicine to a child, the CDC has one rule: “Read the label, follow directions, measure dose using the device that came with it.” Never use a kitchen spoon. A 2023 trial showed this simple approach cut pediatric dosing errors by 31%.
If you’re over 65 and taking five or more meds? You’re in the highest-risk group. 67% of seniors take that many. The label might list 10 interactions, but it won’t tell you how they stack up. That’s why you need a medication review every six months. Ask your doctor or pharmacist to do a “brown bag check”-bring all your meds in, and they’ll sort through them.
And if you’re on blood thinners, seizure meds, or heart drugs? Be extra careful. These are the ones most likely to cause life-threatening interactions. Don’t guess. Don’t assume. Always ask.
What’s Changing (And What’s Coming)
The FDA just updated its labeling rules in June 2024. New labels will start appearing in 2025. The big change? Clearer, bolder warnings. Instead of burying the risk in a paragraph, they’ll highlight the bottom line: “Don’t take with X,” “Stop if you feel Y,” “Call your doctor if Z happens.”
By 2026, your electronic health record will automatically warn your doctor if a new prescription clashes with your current meds. That’s thanks to the 21st Century Cures Act. But until then? You’re still the last line of defense.
Some pharmacies are testing QR codes on bottles. Scan it, and you’ll get up-to-date interaction info, videos, and even audio explanations. Pilot programs started in early 2025. It’s not everywhere yet-but it’s coming.
Your Action Plan
Here’s what to do today:
- Make a list of every medication, supplement, and vitamin you take-including doses and reasons.
- When you get a new prescription, read the label. Find Section 5 and Section 7. Circle any matches to your list.
- Ask your pharmacist: “Does this interact with anything I’m already taking?”
- Write the reason for taking each drug on the bottle.
- Use Drugs.com or a similar tool as a backup-not a replacement.
- Bring your list to every doctor visit.
It takes less than 3 minutes per medication. That’s less time than it takes to scroll through your phone. But it could stop you from ending up in the hospital.
Medications save lives. But they can also hurt you-if you don’t know how to read the label. You don’t need to be an expert. You just need to be careful. And curious. And willing to ask questions.
What should I do if I see a drug interaction warning I don’t understand?
Don’t guess. Call your pharmacist or doctor. Ask them to explain it in simple terms. You can also ask: “Is this something I need to avoid completely, or just watch for symptoms?” Most pharmacists will walk you through it over the phone-no appointment needed.
Can I skip a medication if the label says it interacts with something I take?
Never stop or skip a prescribed medication without talking to your doctor. Some interactions can be managed with dose changes or timing adjustments. For example, taking two drugs 12 hours apart might reduce the risk. Your doctor might even switch you to a safer alternative. But only they can decide what’s safe for you.
Do I need to worry about interactions with food or alcohol?
Yes. Grapefruit juice can make some cholesterol and blood pressure meds dangerously strong. Alcohol can increase drowsiness with painkillers or anxiety meds. The label should mention this in the “Warnings” section. If it doesn’t, ask your pharmacist. Many interactions with food and alcohol aren’t listed on the label but are still dangerous.
Why don’t prescription labels list interactions with herbal supplements?
Because supplement manufacturers aren’t required to prove safety or effectiveness like drug makers are. So the FDA doesn’t require drug labels to list interactions with them-unless there’s strong, proven evidence. That’s why it’s so important to tell your doctor and pharmacist about every herb, vitamin, or tea you take. Even if you think it’s “natural,” it can still cause serious reactions.
How often should I review my medication list?
Every time you get a new prescription, and at least every six months. If you change doctors, switch pharmacies, or start feeling different-like more tired, dizzy, or nauseous-review your list right away. Your body changes. Your meds might need to change too.












13 Comments
Bro, I once took ibuprofen with my blood thinner because the label said 'take with food' and I thought that meant 'it's fine with other stuff.' Ended up in the ER with a hematoma the size of a grapefruit. Don't be me.
It is imperative to underscore that pharmacokinetic interactions, particularly those mediated via the CYP450 enzyme system, remain underappreciated by the lay public. The absence of standardized patient education protocols constitutes a systemic failure in pharmaceutical safety governance.
Let me tell you something-reading the label isn't just a good habit, it's a survival skill. I'm a pharmacist, and I see people come in every single day with a bottle of St. John’s wort, ginkgo, or some ‘natural’ energy booster they got from Amazon, and they have no idea it’s tanking their warfarin levels or making their antidepressant useless. You don’t need a degree to understand ‘avoid use with’ or ‘monitor for bleeding.’ But you do need to stop assuming your supplements are harmless just because they’re sold next to granola bars. Write down everything. Bring it to your pharmacist. Ask them to explain it like you’re five. They won’t judge you-they’ve seen a diabetic take metformin with grapefruit juice and then wonder why they passed out at the grocery store. You’re not dumb for not knowing. You’re just uneducated. And education is free. Go do it.
Man, this is so real. I used to skip reading labels because I thought ‘if it’s prescribed, it’s safe.’ Then my grandma nearly had a stroke because she was mixing her blood pressure med with a ‘heart health’ supplement she got from her yoga teacher. Now I make her read everything out loud with me. It’s awkward, but it saves lives. Also-QR codes on bottles? Yes please. I can barely read the tiny print anyway.
Indeed, the responsibility for medication safety rests not solely upon the physician or the pharmacist, but upon the individual who consumes the medication. In my country, we often rely on traditional remedies without disclosing them to allopathic practitioners. This practice, while culturally rooted, poses significant risk. I now maintain a written log of all substances ingested, and I present it to every healthcare provider without exception. A small effort, but one that may prevent catastrophe.
lmao i once took tylenol with my anticoagulant bc i thought it was just for pain. turns out it was a bad idea. now i just yell at my pharmacist every time i get a new script. they laugh but they get it.
isnt it strange how we trust machines to fly us across oceans but we dont trust ourselves to read a label? maybe the real danger isnt the drugs… its the illusion that someone else is watching out for us. we are all just walking pharmacies with a list of unknown variables.
As an officer who has seen the consequences of negligence, I urge every citizen to treat medication safety with the seriousness it deserves. In India, we have a culture of self-medication, often fueled by misinformation. The label is not a suggestion-it is a legal and medical safeguard. Take the time. Ask questions. Protect your life and the lives of your loved ones. Knowledge is the only true medicine.
Just started reading my labels after my cousin had to get a blood transfusion because of a supplement she didn’t tell anyone about. Honestly? It’s not hard. Just take 30 seconds. I even took a picture of my list and saved it on my phone. Now I show it to every doc. Feels like a superpower.
the fda is lying. they dont want you to know that big pharma pays to hide interactions. that’s why supplements are left out. they’re too cheap to patent. next they’ll say aspirin causes cancer. trust no one. burn your pills.
ok but like… why is this label so tiny?? i need glasses just to read ‘do not take with grapefruit’ and i’m 32?? this is a crime. also why is the font smaller than the fine print on my credit card? someone get me a magnifying glass and a lawyer.
This is one of the most practical pieces of health advice I’ve read in years. Simple, clear, and backed by data. I’ve started sharing this with my parents and friends. Small changes, big impact.
AMERICA IS DYING FROM STUPIDITY. READ THE LABEL OR DIE. NO EXCUSES. NO WHINING. NO SUPPLEMENTS. JUST FOLLOW THE INSTRUCTIONS OR GET OUT OF THE WAY.