Blood Thinner Reversal Agent Selector
Select Your Blood Thinner
Choose the blood thinner you need to reverse. The correct reversal agent will be displayed below.
Reversal Information
Select a blood thinner to see the appropriate reversal agent.
When someone is on a blood thinner, the goal is simple: stop dangerous clots before they form. But what happens when things go wrong? A fall, a stroke, a major bleed - suddenly, the very drug saving their life becomes a life-threatening problem. The good news? We now have tools to reverse these medications quickly. The bad news? Choosing the right one isn’t simple, and delays can be fatal.
Why Reversal Matters More Than Ever
Over 12 million Americans take blood thinners today, mostly for atrial fibrillation, deep vein thrombosis, or after joint replacements. Most of these are now novel oral anticoagulants (NOACs) - drugs like dabigatran, rivaroxaban, apixaban, and edoxaban. They’re easier to use than warfarin, don’t need regular blood tests, and have fewer food interactions. But until 2015, there was no reliable way to undo their effects in an emergency. Before idarucizumab and andexanet alfa arrived, doctors had to rely on older, less precise tools like four-factor prothrombin complex concentrate (4F-PCC) or fresh frozen plasma. These worked inconsistently, especially for NOACs. In a major bleed, every minute counts. A 2021 meta-analysis of over 150 studies found that without a specific reversal agent, the chance of stopping bleeding dropped by nearly half.The Two Main Reversal Agents - And When to Use Them
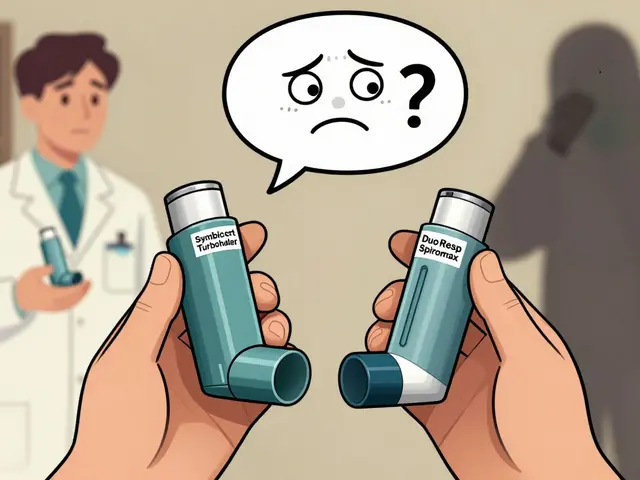
There are two FDA-approved, targeted reversal agents - each designed for a different class of blood thinner.- Idarucizumab (Praxbind) reverses dabigatran (Pradaxa). It’s a monoclonal antibody fragment that grabs dabigatran molecules like a magnet and pulls them out of circulation. Within minutes, clotting function returns to normal.
- Andexanet alfa (AndexXa) reverses Factor Xa inhibitors - that’s rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Savaysa). It works by acting as a decoy: it binds to the drug so it can’t inhibit Factor Xa, letting clotting resume.
How Fast Do They Work?
Speed is everything in emergencies. Here’s what the data shows:- Idarucizumab achieves near-total reversal of dabigatran in under 5 minutes. In the RE-VERSE AD trial, 100% of patients showed complete reversal of anticoagulation within minutes. For someone with a brain bleed, that means surgeons can operate in about 1.6 hours - compared to 4.7 hours with older methods.
- Andexanet alfa stops bleeding in 83% of cases within 2.5 hours. In patients with intracranial hemorrhage, bleeding ceased in under 3 hours on average. But it takes a two-hour infusion, so it’s slower to start than idarucizumab.
Cost, Risk, and the Hard Choices
These drugs aren’t cheap. And the price tag changes who gets them.- Idarucizumab costs about $3,800 per vial. Two vials are standard - so around $7,600 per treatment.
- Andexanet alfa runs about $17,900 per treatment. That’s more than double the cost of idarucizumab - and it’s not even twice as effective.
- 4F-PCC, the non-specific alternative, costs $1,500-$3,000. It works for both classes of drugs, but less reliably.
What About Rebound Bleeding?
One hidden danger: the drug can come back. Dabigatran has a long half-life. Even after idarucizumab clears it from the blood, more of the drug can leak out of tissues over the next 24 hours. In the RE-VERSE AD trial, 23% of patients saw dabigatran levels rise again above dangerous levels - and 10 of them had recurrent bleeding. That’s why monitoring doesn’t stop after the IV drip ends. Patients need at least 24-48 hours of observation. Some need a second dose of idarucizumab. Emergency teams now keep extra vials ready - just in case.What Do You Do If You’re Not in a Hospital?
This isn’t a home treatment. All reversal agents require IV administration and constant monitoring for clots, heart rhythm issues, or allergic reactions. If someone on a blood thinner has a major bleed - vomiting blood, head trauma, sudden weakness - call 911. Don’t wait. Don’t try to drive them yourself. In the ER, the first step is confirming which drug they’re on. Blood tests like dilute thrombin time (for dabigatran) or anti-Factor Xa activity (for Xa inhibitors) help. But in a true emergency, doctors often start reversal based on what the patient says they take - and adjust later.
What’s Coming Next?
The future might be simpler. A drug called ciraparantag (PER977) is in Phase III trials. It’s designed to reverse all major anticoagulants - including heparin, warfarin, dabigatran, rivaroxaban, and apixaban - with one injection. Early results show it works in under 10 minutes. If it gets approved, it could replace all current reversal agents. No more guessing which drug the patient took. No more stocking two expensive vials. Just one universal solution. But it’s not here yet. As of late 2025, ciraparantag is still being tested. Until then, we’re stuck with the tools we have.What Should You Know as a Patient?
If you’re on a blood thinner:- Know exactly what you’re taking - brand and generic names.
- Carry a medical alert card or wear a bracelet listing your drug.
- Know the signs of major bleeding: black stools, vomiting blood, sudden severe headache, unexplained bruising, swelling or pain in limbs.
- Tell every doctor, dentist, or ER staff member you’re on a blood thinner - even if you think it’s obvious.
- Don’t skip doses unless instructed. Missing one doesn’t make you safer - it makes you vulnerable to clots.
Bottom Line: Reversal Is Possible - But It’s Not Perfect
We’ve come a long way. Ten years ago, a major bleed on a NOAC meant a 20% chance of death. Now, with the right agent, that risk drops to around 18%. It’s not a cure. It’s a bridge - buying time so doctors can fix the problem behind the bleed. Idarucizumab is fast, reliable, and low-risk for dabigatran users. Andexanet alfa works for three drugs, but brings higher clotting risks and a hefty price. 4F-PCC remains a practical backup - especially where budgets are tight. The best strategy? Prevention. Take your meds as prescribed. Avoid alcohol and NSAIDs like ibuprofen. Tell your care team about every new drug or supplement. And if you’re at risk for falls or trauma - talk to your doctor about whether a blood thinner is still the right choice. Reversal agents saved lives. But they’re not magic. They’re tools - and like any tool, they work best when you know how to use them.Can you reverse blood thinners at home?
No. Reversal agents like idarucizumab and andexanet alfa require intravenous administration and continuous monitoring in a hospital setting. They cannot be given at home. If you suspect a major bleed, call emergency services immediately.
Which blood thinner is hardest to reverse?
Before 2015, all NOACs were hard to reverse. Today, dabigatran is the easiest with idarucizumab, which achieves 100% reversal in minutes. Factor Xa inhibitors (rivaroxaban, apixaban, edoxaban) are reversed by andexanet alfa, but it’s slower and carries higher clotting risks. Warfarin is still reversed with vitamin K and 4F-PCC - it’s reliable but takes hours to fully work.
Do reversal agents cause blood clots?
Yes, they can. Andexanet alfa has a 14% risk of causing dangerous clots like strokes or pulmonary embolisms. Idarucizumab carries a lower risk - around 5%. Even 4F-PCC can trigger clots in 8% of cases. This is why patients are monitored closely for 24-48 hours after reversal, even if bleeding stops.
How long does it take for a blood thinner to wear off naturally?
It depends on the drug and your kidney function. Dabigatran lasts 12-17 hours in healthy people, but up to 30 hours if kidneys are impaired. Rivaroxaban and apixaban last 8-15 hours. Warfarin can take days to clear. In emergencies, you can’t wait - that’s why reversal agents exist.
Is there a universal reversal agent coming?
Yes - ciraparantag (PER977) is in Phase III trials as of 2025 and has shown promise in reversing all major anticoagulants, including heparin and NOACs, within 5-10 minutes. If approved, it could replace current agents by 2027, simplifying emergency care.
Can you take a blood thinner after a reversal?
Yes - but only under strict medical supervision. After reversal, your clotting risk returns quickly. If you had a stroke or clotting event, your doctor may restart the same drug, switch to a different one, or use mechanical options like a left atrial appendage closure device. Never restart on your own.










13 Comments
so like... uhhh idarucizumab? i think i spelled that right?? anyway, why does everything cost 20k now? my cat's vet bill was less than this and she just licked a poison ivy leaf lmao 💸
America. 🇺🇸 Where your life is worth $17,900 and your kidneys are just a suggestion. If you can't afford the reversal drug, you deserve to bleed out. #MakeHealthcareGreatAgain
This is so important. Knowing your meds and wearing a bracelet could save your life. 💪 You're not alone in this - reach out if you need help organizing your meds!
The fundamental epistemological flaw in contemporary hemostatic interventionism lies in its ontological reduction of coagulopathy to pharmacological negation. One cannot 'reverse' a physiological cascade without addressing the systemic dysregulation that precipitated it. The market-driven proliferation of targeted agents reflects not therapeutic progress, but capitalistic fragmentation of clinical reasoning.
NOACs are just corporate toys. Warfarin worked fine for 70 years. Now we pay 20k for a drug that takes 2 hours to work and gives you clots. Pharma is raping us all
It's fascinating how we've engineered such precise molecular countermeasures - monoclonal antibodies that act like guided missiles against dabigatran, decoy proteins that trick Factor Xa inhibitors into binding to them instead of our clotting factors - yet we still treat this like a technical problem rather than a moral one. We have the science to save lives in minutes, but we ration access based on insurance tiers and hospital budgets. The real tragedy isn't the bleeding - it's that we've built a system where the difference between life and death is often just whether your hospital's pharmacy director had the foresight to spend $18,000 on a vial you might never need. And then we wonder why people distrust medicine.
I had a friend on Eliquis who fell and cracked her skull. They gave her the andexanet thing and she was fine... but then she had a mini stroke 3 days later. The docs were like 'yeah that happens'. I'm just saying... sometimes the cure feels worse than the disease 😔
The data is unequivocal: idarucizumab provides superior time-to-hemostasis metrics compared to andexanet alfa, with a statistically significant reduction in recurrent hemorrhage events (p<0.01). However, the economic burden and thromboembolic risk profile of andexanet alfa necessitate a tiered formulary approach in resource-constrained settings. Institutional protocols must prioritize evidence-based triage, not cost minimization. The ethical imperative to preserve life cannot be subordinated to fiscal austerity.
Ciraparantag sounds like sci-fi 😍 Imagine one shot for everything - warfarin, heparin, NOACs, all gone in 10 mins. I hope they approve it soon. This is the future we deserve 🚀
It’s deeply concerning that patients are being encouraged to carry medical alert bracelets - as if the onus of systemic failure should rest on the individual. We have created a medical landscape where people must arm themselves with plastic cards to avoid being left to die because their hospital can't afford a $17,900 vial. This isn’t healthcare. This is triage capitalism dressed in white coats. And yet, we praise the 'innovation' of reversal agents while ignoring the fact that they exist only because we refused to regulate drug pricing in the first place.
so like... i got my bro on xarelto and he was like 'bro this stuff is easy' and then he fell off his bike and i was like 'oh no' and we rushed him and they gave him the andex thing and he was fine but then he got a clot and now he's on blood thinner again 😭 life is wild
You're not alone. If you're on a blood thinner, you're doing something brave every day. Keep track of your meds, talk to your team, and remember - you're not a burden. You're someone who's fighting to stay here. 💛
If you're taking a blood thinner, you're essentially gambling with your life. The reversal agents are just a bandage on a bullet wound. You think you're safe because you're 'on medication'? No. You're just a walking time bomb with a price tag. And if you can't afford the antidote? You're just another statistic they'll cite in a grant proposal.