Bile Acid Sequestrant Timing Calculator
Medication Timing Calculator
Bile acid sequestrants like colesevelam bind medications in your gut. Proper timing ensures medication effectiveness.
Quick Takeaways
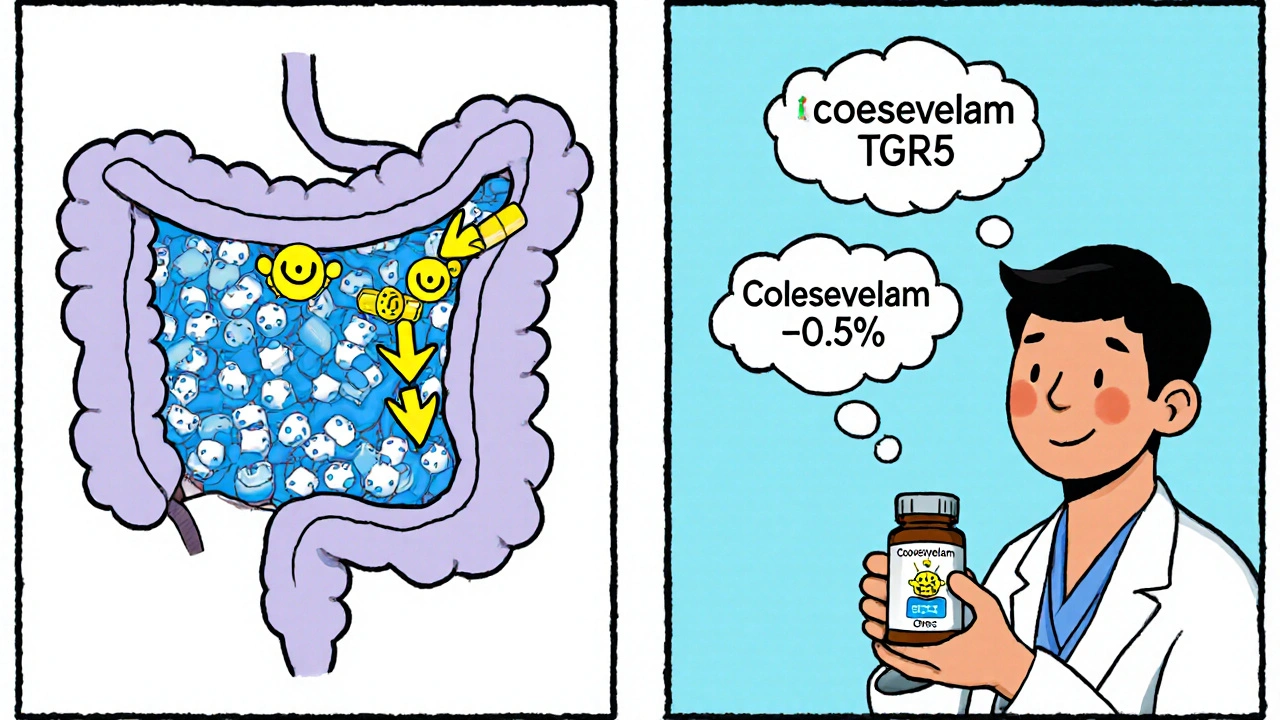
- Bile acid sequestrants lower HbA1c by ~0.5% and cut LDL‑C 15‑18%.
- GI upset (constipation, nausea) affects 20‑30% of users.
- Take them at least 4 hours apart from thyroid meds, warfarin, statins and most oral antidiabetics.
- Best fit: patients with mild hyperglycemia + significant dyslipidemia who can’t tolerate statins.
- Future BASs aim for better tolerability but market share keeps shrinking.
What are Bile Acid Sequestrants?
When it comes to managing type 2 diabetes, bile acid sequestrants are a class of non‑absorbable resins that bind bile acids in the gut and prevent their reabsorption. The first products, like cholestyramine, were launched in the 1970s to lower cholesterol. Over the years they earned a second life in diabetes because binding bile acids triggers a cascade that indirectly improves glucose handling.
How They Influence Blood Sugar
The liver reacts to the loss of bile acids by ramping up cholesterol 7 alpha‑hydroxylase (CYP7A1), the enzyme that makes new bile acids from cholesterol. This shift activates two receptors that sit on gut and liver cells: the farnesoid X receptor (FXR) and the G‑protein‑coupled receptor TGR5. Both receptors help regulate glucose production, insulin sensitivity and even energy expenditure. In practice, the net result is a modest reduction in HbA1c-about 0.3‑0.6 % when the drug is added to metformin.

FDA‑Approved Options for Diabetes
The only BAS formally approved for glucose control in the United States is colesevelam (brand WelChol). It comes in 625 mg and 1 250 mg tablets, usually taken as 3.75 g per day (six 625 mg tablets) with meals. A typical titration starts at 1 875 mg daily and climbs over four weeks to the full dose to ease GI symptoms.
Another resin, sevelamer (Renvela), was designed for phosphate binding in kidney disease. Doses range from 800 mg to 1 600 mg three times daily with meals. While not FDA‑approved for diabetes, several trials reported similar HbA1c drops, but the pill burden and cost keep it off the mainstream diabetes formulary.
The first‑generation agent cholestyramine is still on the market for cholesterol, yet its gritty texture and high dose (often >10 g/day) make it rarely chosen for glucose control today.
Effectiveness Compared to Other Diabetes Classes
| Agent | Typical HbA1c reduction | LDL‑C impact | Common side effects | Notable drug interactions | FDA diabetes indication? |
|---|---|---|---|---|---|
| Colesevelam (BAS) | ≈ 0.5 % | ‑15 % to ‑18 % | Constipation, nausea, bloating | Thyroid meds, warfarin, statins, metformin | Yes (2008) |
| Sevelamer (BAS) | ≈ 0.4 % | ‑12 % to ‑15 % | GI upset, hyperphosphatemia | Similar to colesevelam | No |
| Liraglutide (GLP‑1 agonist) | 0.8 %‑1.5 % | ‑10 % to ‑15 % | Nausea, vomiting, pancreatitis risk | None major; injectables | Yes |
| Empagliflozin (SGLT2 inhibitor) | 0.66 %‑1.03 % | ‑5 % to ‑8 % | Genital infections, volume depletion | Diuretics, insulin dose adjustment | Yes |
| Atorvastatin (statin) | ‑0.1 % (minimal) | ‑30 % to ‑50 % | Myopathy, liver enzymes | Warfarin, CYP3A4 drugs | No (lipid‑only) |
Typical Side‑Effect Profile
GI intolerance is the headline. In placebo‑controlled trials, about 20 % of colesevelam users report constipation, compared with 5 % on placebo. Nausea and gas affect roughly a quarter of patients. The texture-chalky and gritty-makes some people stop within the first month. A 2010 GLOWS trial found a 19 % discontinuation rate due to GI problems, versus 5 % for placebo.
On the upside, these agents do NOT cause hypoglycemia or weight gain, which can be a relief for patients already juggling multiple meds.
Drug‑Interaction Pitfalls
The resin’s binding power is a double‑edged sword. It can trap oral medications and cut their absorption dramatically. FDA labeling recommends spacing other drugs at least 4 hours before or 1 hour after taking a BAS.
- Thyroid hormones (levothyroxine): absorption can drop 30‑40 %; split the dose by 6 hours.
- Warfarin: reduced INR has been reported; check levels weekly after starting a BAS.
- Statins: colesevelam cuts simvastatin AUC by ~40 % and atorvastatin by ~20 %; dose adjustments may be needed.
- Metformin and sulfonylureas: modest reduction in blood levels, so monitor glucose closely for the first two weeks.
- Other oral antibiotics, iron supplements, and fat‑soluble vitamins: give them at a different time of day.
Because of these interactions, a thorough medication review is essential before adding a BAS.
Practical Tips for Patients
- Start low: 1 875 mg (three 625 mg tablets) once daily with a main meal.
- Increase by 1 875 mg each week until you reach 3 750 mg, watching for constipation.
- Boost fiber (e.g., psyllium) and water intake to ease stool passage.
- Set a strict schedule: take the resin at dinner, then wait four hours before your thyroid pill.
- Track LDL‑C and HbA1c every 3 months; if LDL drops but glucose stays the same, you may have found a sweet spot.
- Report any severe constipation or abdominal pain to your clinician promptly-rarely it can lead to bowel obstruction.
Who Might Benefit Most?
Think of patients who sit at the intersection of two problems: mild‑to‑moderate hyperglycemia (HbA1c 7‑8 %) and elevated LDL‑C that isn’t fully controlled by a statin (or who can’t tolerate statins). Older adults (55‑75 years) with a history of statin‑related muscle pain often appreciate a pill that tackles both issues without adding weight or hypoglycemia risk.
Conversely, anyone with baseline HbA1c >10 % or severe GI sensitivity is unlikely to see a worthwhile benefit.
Future Outlook
The market for BASs in diabetes is shrinking. Global sales slipped to $1.1 billion in 2024 and are projected to keep falling as GLP‑1 agonists become cheaper and more cardioprotective. Nevertheless, research isn’t dead. A 2023 phase‑2 trial of an elobixibat‑derived BAS showed 40 % fewer GI complaints while preserving the 0.5 % HbA1c drop. Some investigators are also testing colesevelam together with semaglutide, hoping the two mechanisms will reinforce each other.
For now, the practical reality is that BASs occupy a niche: they’re a reasonable third‑line add‑on for a select group of patients, not a frontline therapy.
Frequently Asked Questions
Can bile acid sequestrants cause low blood sugar?
No. Because they work in the gut and don’t stimulate insulin, the risk of hypoglycemia is essentially nil, even when combined with metformin or sulfonylureas.
How long does it take to see a change in HbA1c?
Most studies report a measurable drop after 12‑18 weeks of stable dosing. If you’re not seeing the expected ~0.5 % reduction after three months, talk to your doctor about dose adjustment or a different add‑on.
Do I need to take a BAS with food?
Yes. Taking the resin with a meal helps it bind bile acids efficiently and reduces the chance of stomach upset.
Can I use colesevelam if I’m already on a statin?
You can, but you’ll need to monitor the statin’s blood level. Colesevelam can cut simvastatin exposure by about 40 %, so your doctor may lower the statin dose or switch to a less‑affected agent like pravastatin.
Is there a generic version of colesevelam?
As of 2025, no generic version is approved in the United States. The brand WelChol remains the sole source, costing roughly $550 for a month’s supply.
Bottom line: bile acid sequestrants can be a handy add‑on for the right patient, but they demand careful timing and a willingness to tolerate some gut discomfort.









8 Comments
For patients who are already juggling a statin and metformin, adding a bile‑acid sequestrant can be a pragmatic way to hit two birds with one stone.
Colesevelam’s modest HbA1c drop of about 0.5 % comes without the weight gain or hypoglycemia risk that many oral agents carry.
Just remember to schedule the dose at least four hours away from thyroid hormone or warfarin to avoid absorption issues.
If constipation becomes a problem, a slow titration and extra fiber usually keep things moving.
Oh great, another pill that promises miracles while demanding a master’s degree in pharmacokinetics.
When you line up the timing, the resin acts like a molecular sponge, pulling bile acids out of the gut and freeing up cholesterol for LDL‑C reduction.
Because it’s not absorbed, the systemic side‑effect profile stays minimal, but the trade‑off is a bulky tablet that sits in the stomach for hours.
Take it with a main meal, then wait four hours before your levothyroxine or any other oral medication that could get trapped.
That schedule definitely feels like a hassle, but many of my older patients say the peace of mind from a stable LDL and steady glucose makes it worth the extra planning.
If you pair it with a good water intake and a little psyllium, the constipation usually settles down within a couple of weeks.
Esteemed colleagues, it is evident that the pharmaceutical consortium has orchestrated a clandestine campaign to obscure the true potential of bile‑acid sequestrants, embedding them within a labyrinth of drug‑interaction warnings that only the most diligent of clinicians can decipher.
One might conjecture that the very requirement to separate dosing by four hours is a subtle test of patient compliance, designed to filter out those unworthy of accessing the purported lipid‑lowering benefits.
Nonetheless, for the discerning practitioner who can navigate these obfuscated guidelines, the modest glycemic improvement may serve as a clandestine advantage in the broader therapeutic armamentarium.
Let’s take a step back and consider the full cascade of events that begins when a patient swallows a tablet of colesevelam, because understanding the underlying physiology can really demystify why we see the clinical effects we do.
First, the resin binds bile acids in the intestinal lumen, preventing their enterohepatic recirculation and forcing the liver to synthesize new bile acids from cholesterol, which in turn reduces hepatic cholesterol stores.
This depletion up‑regulates the enzyme cholesterol 7α‑hydroxylase (CYP7A1), a key step that shifts the metabolic balance toward increased conversion of cholesterol to bile acids.
Simultaneously, the rescued bile acids act as ligands for the farnesoid X receptor (FXR) and the TGR5 receptor, both of which have downstream effects on glucose homeostasis, insulin sensitivity, and even energy expenditure.
The activation of FXR in the ileum leads to the production of fibroblast growth factor 19 (FGF19), which travels to the liver and suppresses gluconeogenesis, thereby contributing to the modest HbA1c reduction observed in trials.
Meanwhile, TGR5 activation on enteroendocrine L‑cells stimulates the release of glucagon‑like peptide‑1 (GLP‑1), adding another layer of glycemic control without the risk of hypoglycemia.
From a lipid perspective, the interruption of the bile acid pool reduces the re‑absorption of dietary cholesterol, which translates into the 15‑18 % drop in LDL‑C that is consistently reported across studies.
Patients often notice this LDL‑C improvement within six to eight weeks, making it a useful adjunct for those who cannot tolerate high‑intensity statins or who have residual dyslipidemia despite optimal statin therapy.
However, the trade‑off is the gastrointestinal burden: the resin’s gritty texture can provoke constipation, bloating, and nausea in a sizeable minority of users.
To mitigate these effects, a slow titration schedule-starting at 1 875 mg daily and increasing by the same amount each week-has been shown to improve tolerability without sacrificing efficacy.
In addition, augmenting dietary fiber intake and ensuring adequate hydration are simple yet effective strategies to keep stools soft and regular.
It is also crucial to counsel patients on the timing of their other oral medications, because the resin’s binding capacity can reduce the absorption of thyroid hormones, warfarin, statins, metformin, and various micronutrients by up to 40 %.
For example, levothyroxine should be taken at least six hours apart, while statins like simvastatin may require dose reduction or a switch to a less‑affected agent such as pravastatin.
Monitoring becomes essential during the first two to three months: checking INR for patients on warfarin, re‑checking thyroid‑stimulating hormone, and tracking fasting lipid panels and HbA1c every 12 weeks.
When these practical considerations are addressed, the net clinical benefit-modest glycemic improvement without weight gain, plus a meaningful LDL‑C reduction-can be an attractive option for a select group of patients, especially older adults with statin intolerance.
Bottom line: if you have a patient stuck between borderline diabetes and stubborn LDL, don’t overlook colesevelam as a viable add‑on, but push for a clear dosing schedule and close lab monitoring to make sure the benefits outweigh the gut discomfort.
I’ve seen a few folks feel uneasy about the pill burden, but keeping a simple log of when each medication is taken can really take the guesswork out of it and help you stay on track without the stress.