Parlodel (Bromocriptine) vs. Alternative Dopamine Agonists: A Complete Comparison
Compare Parlodel (bromocriptine) with other dopamine agonists, weigh benefits, side‑effects, dosing, and choose the right option for prolactinoma and beyond.
When dealing with prolactinoma treatment, the process of lowering excess prolactin caused by a pituitary tumor and managing related symptoms. Also known as pituitary prolactinoma therapy, it usually begins with medication before considering surgery or radiation. The first line of therapy is dopamine agonists, drugs such as cabergoline and bromocriptine that activate dopamine receptors to suppress prolactin secretion. Most patients see a sharp drop in prolactin levels within weeks, and tumor size often shrinks without an operation. If meds don’t achieve desired control, many turn to transsphenoidal surgery, a minimally invasive procedure performed through the nasal cavity to remove the adenoma. This approach preserves normal pituitary tissue and carries a low complication rate when done by an experienced neurosurgeon. Throughout the journey, hormonal monitoring, regular blood tests for prolactin and other pituitary hormones that guide dose adjustments and detect recurrence early is essential for long‑term success.
Imaging plays a pivotal role in every step. A high‑resolution MRI scan maps the tumor’s size, shape, and proximity to surrounding structures, helping doctors decide whether medication alone will suffice or if surgery is needed. After surgery, repeat MRI checks confirm complete removal and identify any residual tissue that might require further treatment. Side effects vary by approach: dopamine agonists can cause nausea, dizziness, or low blood pressure, while surgery may lead to temporary nasal congestion or rare hormonal deficits. Lifestyle tweaks—like avoiding stress, maintaining a balanced diet, and staying hydrated—support recovery and improve medication tolerance. Patients who combine proper drug dosing with regular imaging and hormone checks often achieve normal prolactin levels and regain fertility, menstrual regularity, or libido within months.
All of this falls under prolactinoma treatment strategies that blend pharmacology, precise imaging, and diligent follow‑up. In the list below you’ll find articles that dive deeper into each component: how specific dopamine agonists compare, what to expect during transsphenoidal surgery, tips for interpreting MRI results, and real‑world stories of hormone monitoring success. Use these resources to build a clear roadmap for your own care or to support a loved one navigating this condition.
Compare Parlodel (bromocriptine) with other dopamine agonists, weigh benefits, side‑effects, dosing, and choose the right option for prolactinoma and beyond.

Steroid eye drops treat severe eye inflammation but carry risks like glaucoma and cataracts. Learn how to monitor them safely, recognize warning signs, and explore safer alternatives for long-term use.
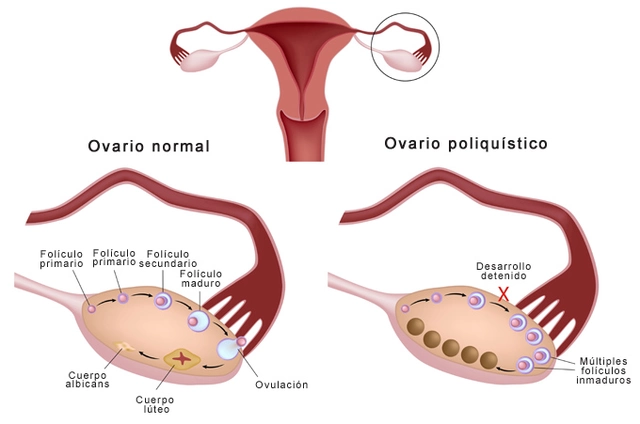
As someone who's been researching Polycystic Ovary Syndrome (PCOS), I recently came across an interesting potential treatment called Enclomiphene. It's a non-steroidal selective estrogen receptor modulator that has shown promising results in stimulating ovulation in women with PCOS. I find it fascinating that Enclomiphene could potentially improve fertility and menstrual regularity in those affected by this condition. Although more clinical trials and research are needed, it's definitely something to keep an eye on. I'll continue to follow the progress of Enclomiphene as a potential game-changer in the treatment of PCOS.

ADHD treatment combines stimulants, non-stimulants, and behavioral strategies for the best results. Learn how each works, their side effects, and what real people experience.

Nickel allergy is more common than you might think, and it’s a leading cause of contact dermatitis worldwide. This article breaks down why nickel triggers skin rashes, what everyday items are the biggest culprits, and how to manage or avoid those annoying flare-ups. Discover how to spot symptoms and learn practical ways to protect your skin if you’re sensitive to nickel. Packed with facts, tips, and relatable advice for anyone struggling with stubborn skin reactions. If you've ever wondered why your skin gets itchy from simple things like earrings or a wristwatch, this is your go-to guide.

The COVID-19 pandemic caused widespread drug shortages and made illegal drugs deadlier due to fentanyl contamination. Millions faced delays in essential medications while overdose deaths surged, exposing deep flaws in healthcare and drug supply systems.
