Blood Thinner Bleeding Risk & Treatment Advisor
This tool helps you understand your bleeding risk based on your blood thinner type and shows evidence-based treatment options from the latest guidelines.
Select your blood thinner and bleeding severity to see personalized recommendations
Talk to Your Doctor
Bring these points to your next appointment:
- "My periods have gotten much heavier since starting [drug name]. I'm changing pads every hour and missing work."
- "Can we consider switching to apixaban or dabigatran if rivaroxaban is causing severe bleeding?"
- "Can I start tranexamic acid or get a levonorgestrel IUD while staying on my current blood thinner?"
If you’re on a blood thinner and your periods have turned into a daily emergency, you’re not alone-and you’re not overreacting. About 70% of menstruating women taking anticoagulants experience heavy menstrual bleeding (HMB) that disrupts work, sleep, and confidence. It’s not a side effect you should just live with. The good news? There are real, effective ways to manage it without stopping your life-saving medication.
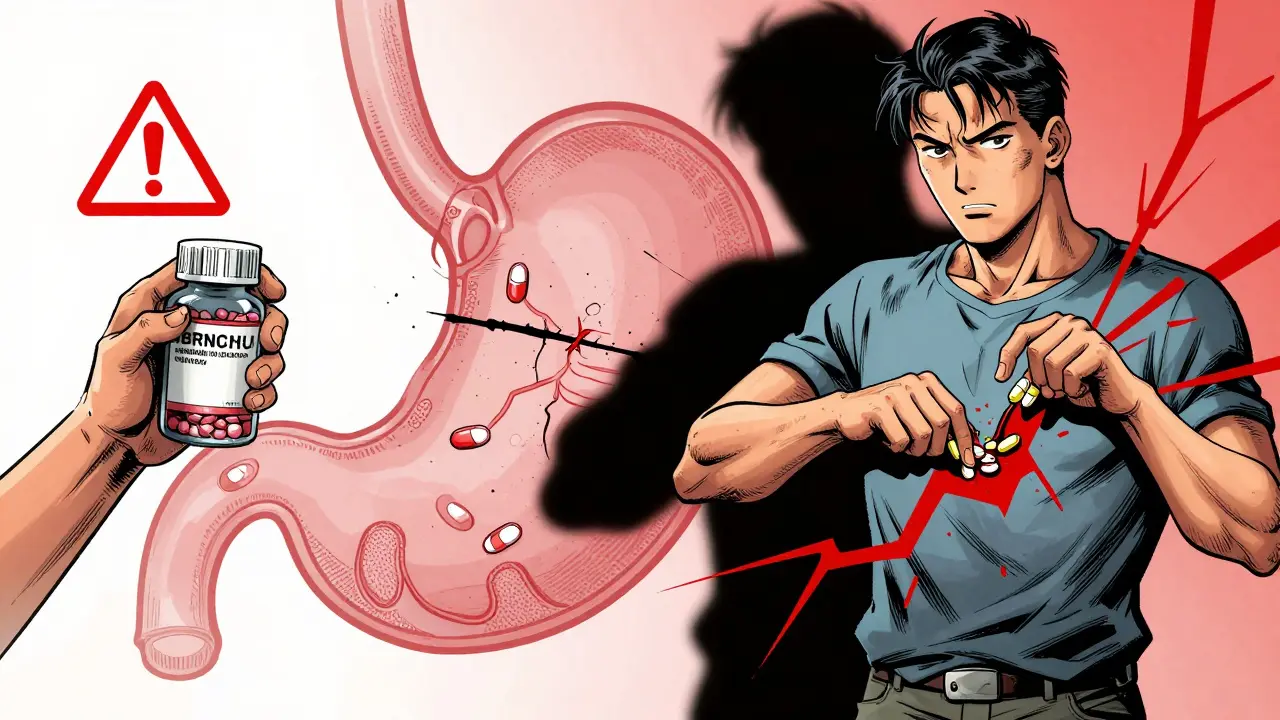
Why Blood Thinners Make Periods So Heavy
Blood thinners-like warfarin, apixaban, rivaroxaban, and dabigatran-work by slowing down your blood’s ability to clot. That’s great for preventing strokes or clots in your legs, but it also means your uterus can’t stop bleeding as efficiently during your period. Normal menstrual bleeding affects 10% to 30% of women. On blood thinners? That jumps to nearly 7 in 10. Some women go from light flows to needing a pad change every 30 minutes. Others bleed through clothes, skip work for days, or end up in the ER.What makes this worse is that most doctors don’t ask about it. A 2023 survey found that 68% of women on anticoagulants said their hematologist never brought up menstrual changes-even though 72% were struggling. That’s a gap in care that’s costing women their quality of life.
Which Blood Thinners Are Least Likely to Cause Heavy Bleeding?
Not all blood thinners are equal when it comes to periods. Research shows clear differences in how much they affect menstrual bleeding:- Apixaban and dabigatran are linked to the lowest risk of heavy bleeding.
- Rivaroxaban carries the highest risk among the newer drugs (DOACs).
- Warfarin is unpredictable-some women handle it fine, others have severe bleeding.
A 2020 study in Blood Advances confirmed that switching from rivaroxaban to apixaban or dabigatran can reduce bleeding in many women. If you’re on rivaroxaban and your periods are unbearable, talk to your doctor about switching. You don’t need to suffer just because your clotting risk is low.
First-Line Treatments That Actually Work
The best part? You don’t have to stop your blood thinner to fix this. These treatments work alongside anticoagulants and are backed by clinical guidelines:1. Levonorgestrel IUD (Mirena, Kyleena)
This small, T-shaped device releases progesterone directly into the uterus. It’s the most effective option for HMB on blood thinners. Studies show it reduces bleeding by 70% to 90% within 3 to 6 months. Many women report their periods becoming light or stopping completely. One woman on Eliquis (apixaban) wrote on Reddit: “After Mirena, my periods went from ER visits to nearly nonexistent.” It also lasts up to 5 years and doesn’t interfere with your anticoagulant.
2. Progestin Pills (Norethisterone)
The American Society of Hematology recommends a high-dose progestin regimen: 5 mg taken three times a day for 21 days, starting at the beginning of your period. This thickens the uterine lining and reduces flow. It’s not a long-term fix, but it’s great for short-term control-especially if you’re waiting for an IUD or can’t use hormones long-term.
3. Tranexamic Acid
This prescription pill helps blood clot in the uterus. Taken only during your period (usually 4 times a day for up to 5 days), it cuts blood loss by 30% to 50%. It’s safe to use with blood thinners, but timing matters. Don’t take it every day-only during bleeding. It’s not a hormone, so it doesn’t affect your cycle long-term. If you’ve tried pads, cups, and tampons with no relief, this is worth a try.
What Doesn’t Work (and What to Avoid)
Some common suggestions can make things worse:
- NSAIDs like ibuprofen or aspirin can reduce bleeding by 20% to 40% in some women, but combining them with blood thinners increases your risk of dangerous bleeding. Avoid unless your doctor specifically approves it.
- Skipping or reducing your blood thinner dose is extremely dangerous. Stopping even for a few days can raise your risk of a clot by five times. Don’t do it.
- Endometrial ablation (a procedure to burn off the uterine lining) works for many women-but it’s risky if you’re on blood thinners. It requires stopping anticoagulants temporarily, which brings back the clot risk. Only consider this as a last resort, and only with a hematologist and gynecologist working together.
Check for Iron Deficiency-It’s Common and Easy to Fix
Heavy bleeding drains your iron. If you’re tired all the time, dizzy, or have cold hands and feet, you might be anemic. A simple blood test for ferritin and hemoglobin can confirm it. Iron supplements are safe to take with blood thinners, and they can restore your energy fast. The National Blood Clot Alliance recommends all women on anticoagulants get checked for iron deficiency at least once a year-or sooner if bleeding is heavy.
How to Talk to Your Doctor
Most doctors aren’t trained to connect anticoagulants with menstrual bleeding. You have to lead the conversation. Here’s what to say:
- “My periods have gotten much heavier since I started [drug name]. I’m changing pads every hour and missing work.”
- “I’ve read that apixaban and dabigatran cause less bleeding than rivaroxaban. Can we consider switching?”
- “Can you refer me to a gynecologist who understands anticoagulant-related bleeding?”
- “Can I start tranexamic acid or get a levonorgestrel IUD while staying on my current blood thinner?”
Bring printed info from the American Society of Hematology or ACOG if your doctor seems unsure. You’re not asking for a favor-you’re asking for standard care.
What’s Changing in 2025
Finally, the medical community is catching up. In 2021, the International Society on Thrombosis and Haemostasis added menstrual bleeding to its official bleeding assessment tools. In 2024, ACOG updated its guidelines to include specific treatment pathways for anticoagulant-related HMB. By mid-2025, the American Society of Hematology and ACOG plan to release joint guidelines-finally giving doctors clear steps to follow.
Until then, you’re your own best advocate. If you’re bleeding heavily on a blood thinner, it’s not normal. It’s treatable. And you deserve to live without fear of leaks, exhaustion, or missed days.
Real Stories, Real Relief
One woman in Perth, on apixaban for a past blood clot, started bleeding so heavily she had to carry extra clothes to work. After switching from rivaroxaban to apixaban and getting a Kyleena IUD, her bleeding dropped 85%. She now runs marathons again.
Another woman in Sydney, on warfarin, started taking tranexamic acid only on her heaviest days. Her periods went from 8 days of soaking through to 3 days of light flow. She stopped needing iron infusions.
These aren’t rare cases. They’re the norm for women who speak up.












9 Comments
Okay, but can we talk about how insane it is that doctors still treat this like a women’s issue they can ignore? I had to bring my own research-printed, highlighted, with sticky notes-to my hematologist before he even considered switching me from rivaroxaban to apixaban. Seven years of bleeding through shirts, two ER visits, and zero empathy until I showed up with citations. This isn’t ‘just heavy periods.’ It’s a systemic failure wrapped in patriarchal silence.
And yes, Mirena changed my life. I went from ‘I need a change of clothes every 45 minutes’ to ‘Wait, is that a spot? Oh, that’s just my imagination.’
Also, tranexamic acid? Magic in a pill. No hormones. No drama. Just stop the flood. Why isn’t this the first thing every OB-GYN says?
This is one of the most well-researched and practical threads I’ve seen on this topic. I’m a nurse practitioner who works with anticoagulated patients, and I can confirm: most providers don’t ask about menses because they don’t know how to address it. The IUD is gold standard-safe, effective, and doesn’t interfere with INR or anti-Xa levels. Tranexamic acid is underused too. I always tell patients: ‘You’re not being dramatic. You’re being medically accurate.’
Side note: if you’re on warfarin and bleeding heavily, check your INR. Sometimes it’s not the drug-it’s the level. But if INR’s in range and you’re still drowning? That’s the drug’s effect. Switching to apixaban or dabigatran is totally reasonable.
Also, iron. Always check iron. Ferritin below 30? Start supplementation. Even if hemoglobin’s okay, low ferritin = fatigue, brain fog, hair loss. It’s not ‘just tired.’ It’s iron deficiency.
As someone from India where menstrual health is still taboo even without blood thinners, this article is a revelation. Here, many women are told to ‘endure’ heavy flow as part of being a woman. The idea that you can switch anticoagulants or use an IUD without compromising clotting safety? Most doctors here don’t even know these options exist.
I’ve seen women on warfarin for atrial fibrillation bleed for 14 days straight and be prescribed ‘iron tablets and rest.’ No one mentions tranexamic acid or IUDs. The gap between global guidelines and local practice is a chasm.
Thank you for writing this. It’s not just helpful-it’s necessary. Maybe someone in a rural clinic in Kerala will read this and change a life.
Look, I’m not a doctor but I’ve read a lot. The fact that you can just pop tranexamic acid during your period and it works? That’s wild. I mean, why isn’t this on the shelf next to ibuprofen? It’s like the medical world decided to make women bleed out while they wait for a specialist.
Also, rivaroxaban is the worst. I know a girl who was on it for DVT and had to quit her job because she was bleeding through her jeans. Switched to apixaban and boom-normal. No drama. No trauma. Just a different pill.
And yeah, IUDs aren’t scary. They’re tiny. They don’t hurt. They save your dignity. Stop listening to your aunt who says ‘it’ll make you infertile.’ That’s 1980s nonsense.
so i was on xarelto and my period was like a horror movie every month. i’d be on the floor with a heating pad and a trash bag full of pads. no joke. i thought i was just unlucky until i found this post.
switched to eliquis + mirena. now i forget when my period is. like, i had to check my calendar yesterday. it’s been 3 months since i needed a pad. i cried. not from sadness. from relief.
also tranexamic acid? i tried it once. felt like a superhero. like, ‘i am the queen of clotting now.’
doctors need to stop acting like this is normal. it’s not. it’s a problem. and it’s fixable.
Let’s be real: most of these ‘solutions’ are just band-aids. The real issue is that anticoagulants were never designed with menstrual physiology in mind. The fact that we’re now retrofitting treatments like IUDs and tranexamic acid just proves how negligent the pharmaceutical industry has been.
Also, apixaban being ‘safer’? That’s relative. It still inhibits Factor Xa. The uterus isn’t a clotting-resistant organ. You’re just trading one risk for another.
And don’t get me started on ‘trusting your gut.’ Women have been told that for centuries. The real solution? More clinical trials with menstrual bleeding as a primary endpoint. Not an afterthought.
Why are we even having this conversation? In India, we have Ayurvedic remedies, yoga, and centuries of wisdom about balancing doshas. Why are we relying on Western pharmaceuticals to fix what nature can manage? Why are we not talking about turmeric, ashwagandha, or pomegranate juice to reduce bleeding?
And why are we normalizing inserting foreign objects like IUDs into the body? That’s invasive. That’s not traditional. That’s corporate medicine selling convenience as cure.
Let’s go back to roots. Let’s stop treating women like broken machines. Let’s heal holistically. Or are we too addicted to pills and devices to remember our own bodies?
I want to hug every woman who read this and thought, ‘I’m not crazy.’ You’re not. You’re just unheard.
I was that woman bleeding through three pads an hour, crying in the bathroom at work, pretending I was just ‘really tired.’ I didn’t say anything for two years because I thought it was normal.
Then I found a gynecologist who actually listened. We switched me to apixaban, I got Kyleena, and I started tranexamic acid on heavy days. I’m not just surviving now-I’m living. I run. I travel. I wear white pants again.
If you’re reading this and you’re bleeding like a faucet? Please, please, please talk to someone. Bring this post. Print it. Tape it to your doctor’s desk. You deserve to feel like yourself again. You’re not alone. And you’re not broken. You’re just overdue for the right care.
Wow. So the solution to bleeding like a broken faucet is… more medicine? More devices? More pills? How about we just stop pretending the body needs to be fixed by a checklist?
Also, IUDs are great. I get it. But let’s not pretend this isn’t the medical-industrial complex selling us convenience as empowerment. You don’t need a T-shaped plastic thing in your uterus to have a normal period. You need a system that listens.
And why are we always the ones doing the research? Why aren’t the doctors already telling us this? Because they’re busy pretending they know everything while we’re Googling our way out of hemorrhage.
Anyway. I’m glad it works for some. Just… don’t make it sound like this is the only way. It’s not. It’s just the most documented way.