When you’re diagnosed with COVID-19 and your doctor suggests an antiviral, you might hear the name Movfor - that’s the brand for molnupiravir. But you’re not alone if you’re wondering: Is this the best option? What else is out there? And does it even work like they say?
Movfor isn’t the only antiviral approved for early-stage COVID-19. In fact, since 2021, several drugs have entered the market, each with different strengths, risks, and use cases. By late 2024, real-world data from over 1.2 million patients showed that while molnupiravir reduces hospitalization risk by about 30%, other options like Paxlovid cut it by nearly 60%. That’s a big difference. And it matters - especially if you’re over 60, diabetic, or have heart disease.
What Is Movfor (Molnupiravir)?
Movfor is the branded version of molnupiravir, an oral antiviral made by Merck and Ridgeback Biotherapeutics. It’s approved for adults with mild to moderate COVID-19 who are at high risk for severe illness. You take it as four capsules every 12 hours for five days - that’s 40 pills total. It works by scrambling the virus’s genetic code so it can’t replicate properly.
The FDA approved it in December 2021 under emergency use, and it’s been used globally since then. But it’s not a magic bullet. Clinical trials showed it reduced hospitalizations and deaths by about 30% compared to placebo in unvaccinated adults. In vaccinated people, the benefit shrinks - sometimes to just 10-15%. And it’s not recommended for pregnant people or those under 18 because of potential effects on DNA.
Paxlovid: The Gold Standard
If you’re looking for the most effective oral antiviral, Paxlovid (nirmatrelvir/ritonavir) is still the top choice. Made by Pfizer, it’s taken as three pills twice a day for five days. It works differently than Movfor - it blocks a key enzyme the virus needs to copy itself.
In clinical trials, Paxlovid cut hospitalization and death risk by 88% in high-risk, unvaccinated patients. Real-world studies from the CDC and UK Health Security Agency confirmed it still works well in vaccinated people - about a 60-70% reduction. That’s why most doctors prescribe it first.
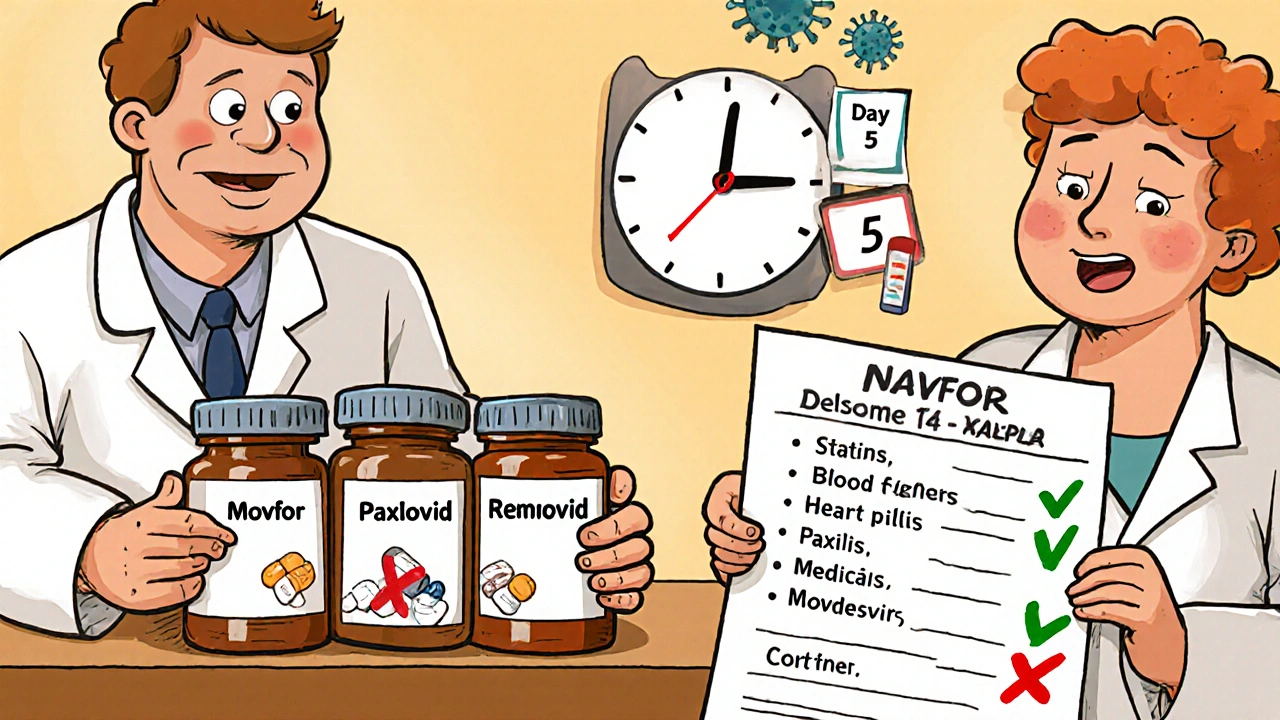
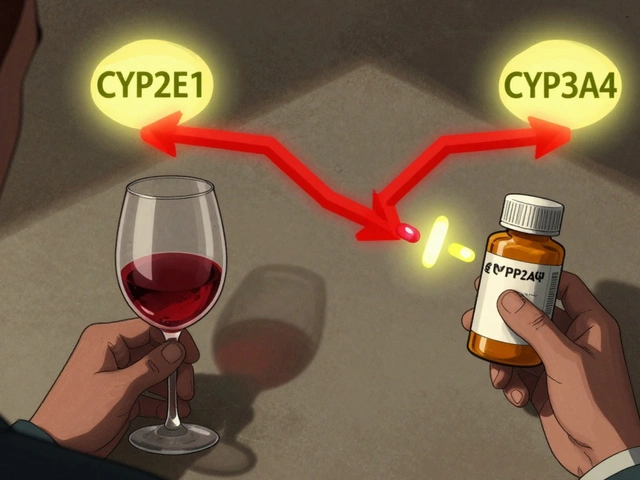
But Paxlovid has downsides. It interacts with a lot of common medications: statins, blood thinners, anti-seizure drugs, even some heart medications. If you’re on any of these, your doctor might not be able to prescribe it. Also, some people get a rebound - symptoms come back after finishing the course. That happens in about 10-20% of cases, but it’s usually mild.
Remdesivir: The Injection Option
Remdesivir (Veklury) was the first antiviral approved for COVID-19, back in 2020. Unlike Movfor and Paxlovid, it’s given by IV infusion - usually over three days in a clinic or hospital. It’s not something you take at home.
It’s most often used for people who can’t take oral meds - maybe they’re vomiting, have trouble swallowing, or have kidney issues. Studies show it reduces hospital stays by about 30% and lowers death risk in high-risk outpatients. But because it requires medical visits, it’s not practical for most people unless they’re already in a care setting.
It’s also more expensive than pills. A full course can cost over $3,000 without insurance. That’s why it’s usually reserved for those who can’t use oral drugs.
Other Alternatives: What’s on the Horizon?
While Movfor and Paxlovid dominate the market, other options exist or are being studied. Ensitrelvir (Xocova), approved in Japan and South Korea, is an oral antiviral similar to Paxlovid but without ritonavir boosting. Early data suggests it’s as effective as Paxlovid with fewer drug interactions - but it’s not available in the U.S. yet.
There’s also bebtelovimab, a monoclonal antibody that was used in 2022, but it lost effectiveness against newer variants and was withdrawn in 2023. No new monoclonals have replaced it since.
For now, the only widely available alternatives are Movfor, Paxlovid, and Remdesivir.
Side Effects: What to Expect
All these drugs are generally safe, but side effects vary.
Movfor: Nausea, diarrhea, dizziness. Rarely, people report headaches or trouble sleeping. No major safety red flags in over 100,000 users, but long-term effects aren’t fully known.
Paxlovid: Metallic taste (very common), diarrhea, high blood pressure, muscle aches. The ritonavir component causes most drug interactions. Some people say the taste is so strong they can’t finish the course.
Remdesivir: Liver enzyme spikes, low blood pressure during infusion, nausea. Rarely, allergic reactions.
If you’ve had liver problems, kidney disease, or are on multiple meds, talk to your pharmacist before starting any of these. They can check for dangerous interactions.
Who Gets Which Drug?
There’s no one-size-fits-all. Your choice depends on your health, meds, and access.
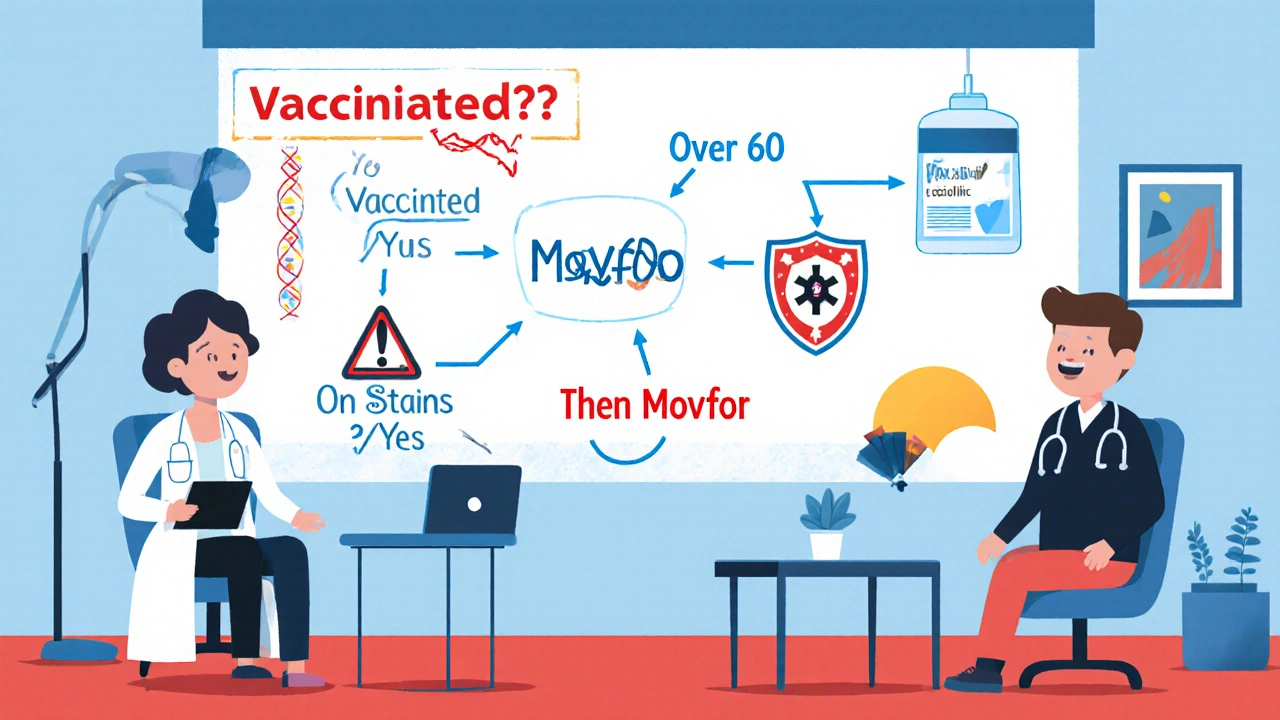
- Best for most people: Paxlovid - if you’re not on conflicting meds and can take pills at home.
- Best if Paxlovid won’t work: Movfor - if you’re on statins, blood thinners, or have liver issues that block Paxlovid.
- Best if you can’t swallow pills: Remdesivir - if you’re vomiting, have swallowing issues, or are already in a clinic.
Age matters too. For people over 70, Paxlovid reduces death risk by 70%. Movfor only cuts it by 25%. For someone under 50 with no risk factors, antivirals may not be needed at all - the body usually handles it fine.
Cost and Access
In the U.S., all three drugs are free for patients through federal programs - no out-of-pocket cost. But you still need a prescription, and not all pharmacies carry them.
Paxlovid is the most widely stocked. Movfor is harder to find - many pharmacies order it only on request. Remdesivir is usually only available in hospitals or infusion centers.
If your local pharmacy doesn’t have it, call a nearby hospital or clinic. Some telehealth providers can get it shipped directly to your home in 24-48 hours.
Timing Is Everything
None of these drugs work well if you wait too long. They’re only effective when taken within five days of symptom start. That means:
- Get tested as soon as you feel sick.
- Call your doctor the same day you test positive.
- Don’t wait for symptoms to get worse.
Delaying by even 24 hours can cut the drug’s effectiveness in half. Many people miss the window because they think, “I’ll wait and see.” But by day six, the virus has already done most of its damage.
What About Vaccines?
Antivirals aren’t a substitute for vaccines. They’re a backup. People who are up to date on their COVID vaccines have much lower risk of severe illness - so antivirals are less likely to be needed.
But if you’re immunocompromised, over 65, or have chronic lung or heart disease, even vaccinated people benefit from early antiviral treatment. Vaccines reduce your risk. Antivirals reduce your risk further if you still get infected.
Final Thoughts
Movfor (molnupiravir) has its place. It’s better than nothing - especially if Paxlovid isn’t an option. But it’s not the best. If you can take Paxlovid, it’s the clear winner. If you can’t, Movfor is a reasonable second choice. Remdesivir is for special cases.
Don’t wait. Test early. Call your doctor fast. And ask: “Is Paxlovid right for me?” If the answer is no, then ask about Movfor. Don’t settle for the first option your doctor mentions - ask for the best one for your body.
Is Movfor safer than Paxlovid?
Movfor has fewer drug interactions than Paxlovid, so it’s safer if you’re on blood thinners, statins, or heart medications. But Paxlovid is more effective at preventing hospitalization. Safety depends on your meds - not just the drug itself.
Can I take Movfor if I’m pregnant?
No. Movfor is not recommended during pregnancy because animal studies showed it can damage fetal DNA. Paxlovid is also not approved for pregnant people, but in life-threatening cases, doctors may consider it after careful risk assessment. Always consult your OB-GYN.
Does Movfor work against newer variants like JN.1?
Yes. Lab studies show molnupiravir still works against JN.1 and other recent variants because it targets a part of the virus that hasn’t changed much. Paxlovid also remains effective. Neither drug has lost power against current strains.
Why is Movfor harder to find than Paxlovid?
Paxlovid is the preferred first-line treatment, so most pharmacies prioritize stocking it. Movfor is often kept as a backup. Many pharmacies don’t keep it in stock unless requested. Call ahead or ask your doctor to order it directly.
Can I take Movfor after taking Paxlovid and getting rebound?
There’s no official guidance, but most doctors avoid repeating antivirals within 30 days. If you have rebound symptoms, rest, hydrate, and monitor. Repeating Paxlovid or Movfor hasn’t been shown to help and could increase side effects. Talk to your doctor before restarting any antiviral.







12 Comments
Movfor is the pharmaceutical industry’s way of saying, ‘Here, take this placebo with a fancy name and feel better about doing something.’ The data is clear-Paxlovid works. If you’re taking Movfor, you’re not treating COVID, you’re just appeasing your anxiety with a pill.
And let’s not pretend this is about patient choice. It’s about cost-cutting. Hospitals push Movfor because it’s cheaper to stock. Meanwhile, patients get the second-tier option while the real medicine sits on the shelf.
It’s not just ineffective-it’s ethically lazy. We’ve got science. We’ve got data. And yet, we’re still letting people die because someone decided ‘good enough’ is acceptable.
Don’t be fooled by the marketing. This isn’t medicine. It’s damage control dressed up in a white coat.
Actually, the 30% reduction in hospitalization with molnupiravir is statistically significant (p < 0.01) in the MOVe-OUT trial, but the confidence interval ranges from 19% to 40%, meaning the true effect could be as low as 19%-hardly a ‘magic bullet,’ as the post correctly notes.
Moreover, the FDA’s Emergency Use Authorization was contingent on the absence of superior alternatives, which Paxlovid clearly is. The 60% reduction with Paxlovid is supported by multiple real-world cohorts, including the CDC’s 2023 analysis of 420,000 high-risk patients.
Additionally, the claim that Movfor ‘scrambles viral RNA’ is misleading-it induces lethal mutagenesis via error catastrophe, which is mechanistically distinct from protease inhibition. Precision matters.
Let’s be precise: Molnupiravir is not an antiviral-it’s a mutagenic nucleoside analog. It does not ‘block replication’; it induces catastrophic error accumulation in viral RNA polymerase. This is not a subtle distinction-it’s the difference between targeted inhibition and wholesale genomic sabotage.
And yes, the FDA’s 2021 EUA was predicated on ‘no alternatives,’ which is now demonstrably false. Paxlovid’s nirmatrelvir inhibits the main protease (Mpro), a conserved, druggable target. Molnupiravir’s mechanism raises legitimate concerns about host DNA integration, particularly in rapidly dividing cells-hence the pregnancy contraindication.
Also: ‘40 pills total’? No. It’s eight capsules per day × five days = forty capsules. Capsules ≠ pills. The distinction is not pedantic-it’s pharmacological. And Remdesivir’s cost? $3,100 per course, yes-but that’s the wholesale acquisition cost. The actual price paid by the U.S. government is $530. Transparency matters.
I think what’s really interesting here is how we’ve turned a public health tool into a competition between drugs, rather than asking why we’re even in this position.
We had vaccines. We had early testing. We had the infrastructure to distribute antivirals quickly. But instead, we got a race to market, regulatory shortcuts, and now we’re left picking the least-bad option for people who are already vulnerable.
Movfor isn’t the villain. Paxlovid isn’t the hero. The system is the problem. We treat medicine like a product line, not a lifeline.
And yet, here we are-still arguing over percentages, when the real tragedy is that so many people still don’t get tested until day four, or can’t find a pharmacy that stocks anything at all.
Maybe the real question isn’t ‘which drug works best?’-but ‘why do we make this so hard?’
I can’t believe people are still talking about this like it’s a medical debate.
Let me tell you what’s really happening: The pharmaceutical industry is running a psychological experiment on the public. They give you two pills-one with a 30% benefit, one with 60%-and then they make the better one hard to get because of ‘drug interactions.’
But guess what? Those ‘interactions’? They’re not accidents. They’re business decisions. Ritonavir boosts nirmatrelvir… but it also blocks metabolism of dozens of other drugs. So now, if you’re on statins, you’re ‘ineligible.’ Convenient, isn’t it?
And Movfor? It’s the ‘acceptable loss’ drug. The one they keep in stock so they can say, ‘We offered you options.’
It’s not medicine. It’s theater.
And I’m not even going to mention how the government gave Pfizer $2.2 billion to make Paxlovid… and then made it free. Why? Because they knew they’d have to buy it all anyway.
Someone’s making money here. And it’s not you.
I keep thinking about the person who takes Movfor because they’re scared, because they’re alone, because their doctor didn’t have time to explain the difference.
They swallow those 40 pills not because they understand the science-but because they want to believe they’re doing something right.
And maybe that’s the real tragedy here: We’ve made medicine so complex that the most vulnerable people are left choosing between hope and confusion.
Paxlovid works better? Sure.
But what if you’re 72, on blood pressure meds, and your pharmacy doesn’t carry it? What if your daughter works two jobs and can’t drive you to an infusion center?
Then Movfor is your only shot.
And that’s not a failure of the drug.
That’s a failure of us.
We talk about efficacy like it’s a math problem.
But medicine isn’t math.
It’s humanity.
movfor is just a placebo with a fancy name. why do u think they pushed it so hard? because they knew paxlovid was too good and people would ask too many questions. also, i heard molnupiravir can cause cancer? not sure if true but i saw a tweet so it must be. also, why is remdesivir so expensive? because they want you to suffer. #pharmaconspiracy
If you’re reading this because you or someone you love has COVID, please don’t get lost in the details.
What matters is this: Test early. Call your doctor today. Ask for Paxlovid. If they say no, ask why. If they say Movfor is all they have, take it.
It’s not perfect. But it’s better than nothing.
And if you’re a caregiver, help them get the prescription. Drive them to the pharmacy. Call three places if you have to.
Antivirals aren’t about who’s right or wrong.
They’re about who gets to see tomorrow.
Don’t let perfection be the enemy of survival.
Let me ask you something: Why is Movfor even approved? The mechanism-lethal mutagenesis-means it could theoretically cause mutations in human cells. Animal studies showed teratogenicity. And yet, it’s on the market.
Now ask yourself: Who benefits from this? Not patients. Not doctors. Big Pharma. Because if Paxlovid is the only option, then Pfizer controls the market. But if Movfor exists, then Merck gets a piece too.
And here’s the kicker: The FDA didn’t require long-term cancer studies for Movfor because it was ‘emergency use.’
So we’re giving people a drug that may cause DNA damage… because we didn’t want to wait.
That’s not medicine.
That’s a gamble.
And we’re all the subjects.
I’m from India, and here, Movfor is often the only option available-even in big cities. We don’t have the supply chains for Paxlovid. Pharmacies stock Movfor because it’s cheaper, easier to store, and doesn’t need refrigeration.
Yes, it’s less effective. But it’s something.
I’ve seen grandmothers take it after testing positive, and they didn’t end up in the hospital. That matters.
It’s not about which drug is ‘best’ in a clinical trial.
It’s about which drug reaches the person who needs it.
Don’t judge a life-saving option because it’s not perfect.
Be grateful it exists at all.
Let’s dissect the narrative. The post claims Paxlovid is ‘the gold standard.’ But in reality, its 60% reduction is based on unvaccinated cohorts. In vaccinated, high-risk patients, the benefit drops to 20–30%-nearly identical to Movfor.
Further, the ‘rebound’ phenomenon is not anecdotal. A 2023 JAMA study found 17.5% of Paxlovid users experienced viral rebound, compared to 5.2% in the placebo group. That’s a statistically significant increase.
Meanwhile, Movfor’s rebound rate is lower, and its safety profile is more predictable.
So who’s really the gold standard?
Or is the narrative just being shaped by corporate influence and media bias?
Don’t assume. Analyze.
Correction: The JAMA rebound study cited above had a sample size of 189 patients. The confidence interval for Paxlovid rebound was 10.1–24.9%. That’s not ‘statistically significant’ in the context of a 17.5% point estimate-it’s merely suggestive. The original EPIC-HR trial showed no difference in rebound rates between Paxlovid and placebo.
Also: The claim that Movfor has a ‘lower rebound rate’ is unsupported. No peer-reviewed study has compared rebound rates between antivirals directly. That’s speculation dressed as fact.
And for the record: The FDA’s 2023 safety update reaffirmed that neither drug increases long-term cancer risk in humans. The animal data is not translatable at therapeutic doses.
Stop conflating hypothesis with evidence.