Switching from warfarin to a direct oral anticoagulant (DOAC) can make life simpler-no more weekly blood tests, fewer food restrictions, and less risk of serious bleeding. But if you do it wrong, you could be at risk for a stroke, a clot, or dangerous bleeding. This isn’t a decision to make on your own. It’s a medical transition that needs precision, timing, and clear guidance.
Why Switch from Warfarin?
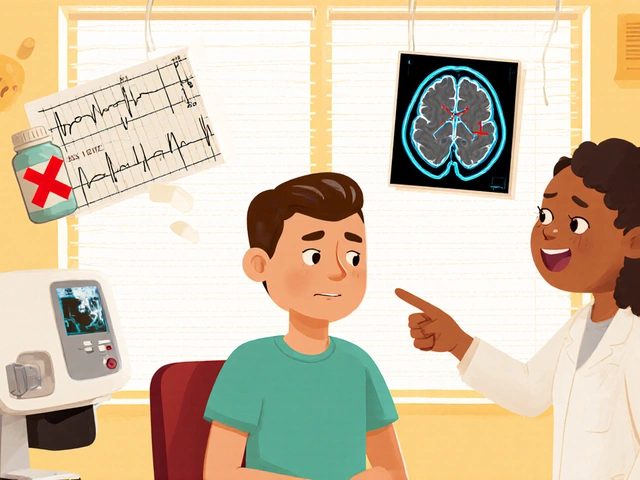
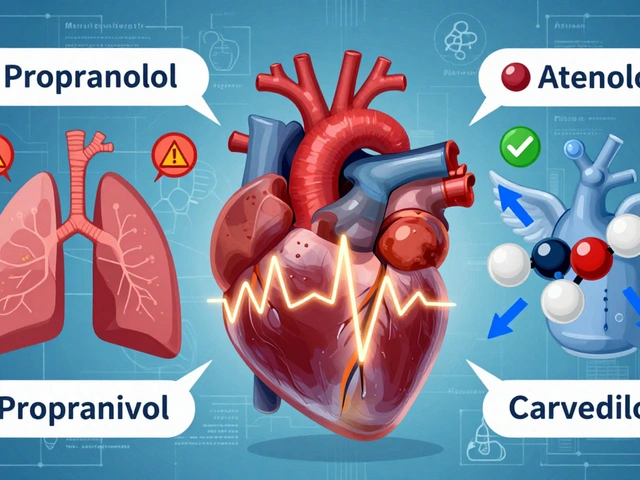
Warfarin has been the go-to blood thinner for over 70 years. It works, but it’s finicky. You need regular INR blood tests-often every 1 to 4 weeks-to make sure your blood isn’t too thin or too thick. Even small changes in diet, other medications, or how well you sleep can throw your INR off. That’s why millions of people are switching to DOACs like apixaban, rivaroxaban, dabigatran, and edoxaban. DOACs don’t need routine blood tests. They work more predictably. You take the same dose every day, and your doctor doesn’t have to tweak it constantly. Studies show they’re just as good at preventing strokes in people with atrial fibrillation-and they cause fewer brain bleeds. The RE-LY trial found intracranial hemorrhage dropped from 4.0 to 2.7 events per 100 patient-years with dabigatran compared to warfarin. But switching isn’t just swapping one pill for another. It’s a high-stakes handoff. If you stop warfarin too early, your blood can clot. If you start the DOAC too soon, you could bleed. Timing matters.When to Start the DOAC: The INR Rules
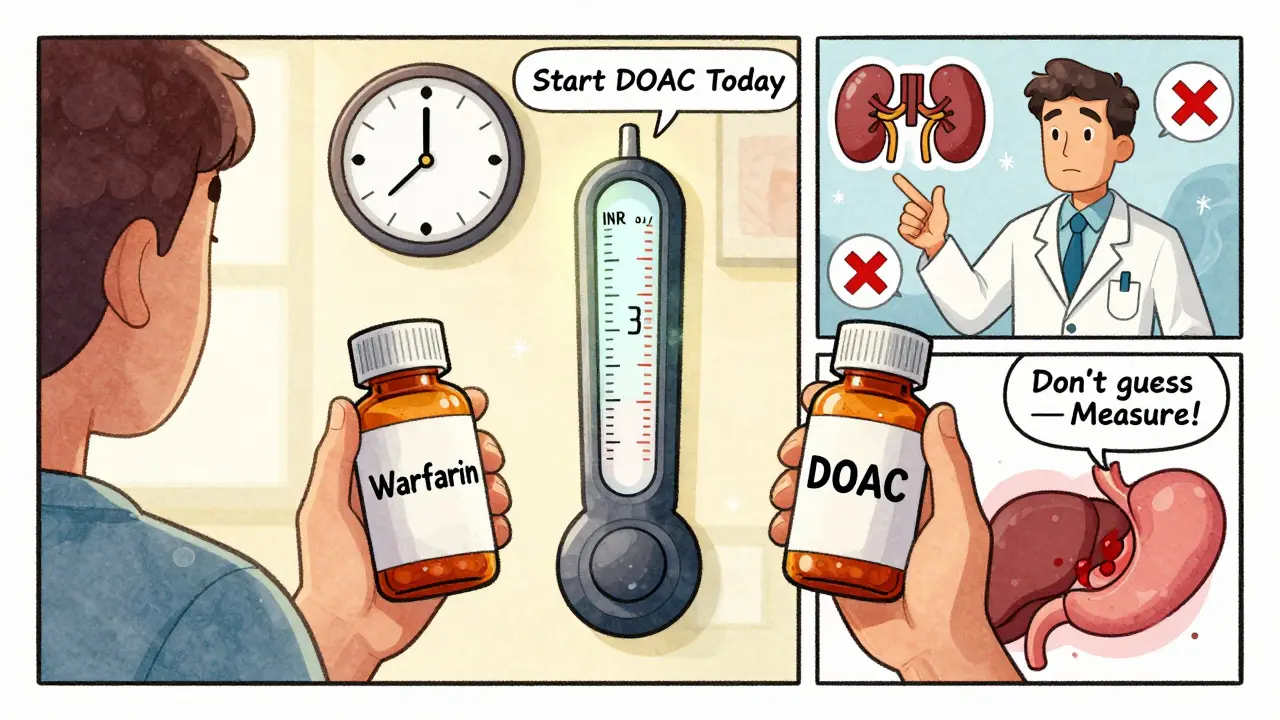
The key to a safe switch is your most recent INR number. This isn’t a guess. It’s a measurement. Here’s what experts say:- If your INR is 2.0 or lower: You can start the DOAC right away.
- If your INR is between 2.0 and 2.5: Start the DOAC the same day or wait until the next day.
- If your INR is between 2.5 and 3.0: Wait 1 to 3 days, then recheck your INR.
- If your INR is 3.0 or higher: Don’t start the DOAC. Wait 3 to 5 days and test again.
Who Shouldn’t Switch?
Not everyone is a candidate. Some people should stay on warfarin. Here’s who:- Anyone with a mechanical heart valve. DOACs don’t work here. Warfarin is still the only option.
- People with severe kidney disease (CrCl under 15-30 mL/min, depending on the DOAC). Dabigatran and edoxaban are especially risky in advanced kidney failure.
- Those with advanced liver disease (Child-Pugh Class C). The liver helps clear these drugs. If it’s failing, the DOAC can build up to dangerous levels.
- Women who are pregnant or breastfeeding. DOACs can cross the placenta and harm the baby. Warfarin is still preferred in pregnancy, though it carries its own risks.
Side Effects You Might Not Expect
DOACs are safer overall, but they have their own risks.- Gastrointestinal bleeding: Dabigatran, in particular, can irritate the stomach lining. If you have a history of ulcers, your doctor may avoid it.
- INR elevation: DOACs can falsely raise your INR number. That doesn’t mean you’re over-anticoagulated. It’s a lab artifact. Never adjust your dose based on an INR taken after switching to a DOAC.
- Missed doses: Unlike warfarin, DOACs leave your system in 12 to 24 hours. If you skip a dose, your protection drops fast. That’s why consistency matters more than ever.

What About Surgery or Procedures?
If you’re scheduled for a procedure-dental work, colonoscopy, even a minor skin surgery-you need a plan. Stopping your DOAC too early? Risk of clot. Stopping too late? Risk of bleeding. Here’s what works in practice:- Low-risk procedure (e.g., tooth extraction): Hold dabigatran 24 hours if your kidney function is normal (CrCl >90 mL/min). Hold 36 hours if your kidneys are moderate (CrCl 45-50 mL/min).
- High-risk procedure (e.g., joint replacement): Hold dabigatran for 96 to 108 hours if your CrCl is 45 mL/min. That’s 4 to 4.5 days.
How to Make the Switch Safely
There’s a proven five-step process used in Australia and Canada:- Check your bloodwork. Make sure you’ve had recent kidney and liver tests (within the last 6 months). If not, get them done.
- Measure your INR. Do this right before your switch. Don’t rely on an old result.
- Calculate your CrCl. Use the Cockcroft-Gault formula: (140 - age) × weight (kg) × [0.85 if female] / (72 × serum creatinine). Your doctor will do this for you.
- Prescribe the right DOAC and dose. Doses vary by kidney function, weight, and indication. Apixaban 5 mg twice daily? Or 2.5 mg? That depends on your age, weight, and creatinine levels.
- Give clear instructions. Tell the patient exactly when to stop warfarin and when to start the DOAC. Write it down. Give them a printed schedule.
What If You Miss a Dose?
DOACs don’t forgive missed pills like warfarin sometimes does. If you miss a dose:- If it’s within 6 hours of your usual time: Take it right away.
- If it’s more than 6 hours late: Skip it. Don’t double up.
- Resume your regular schedule the next day.
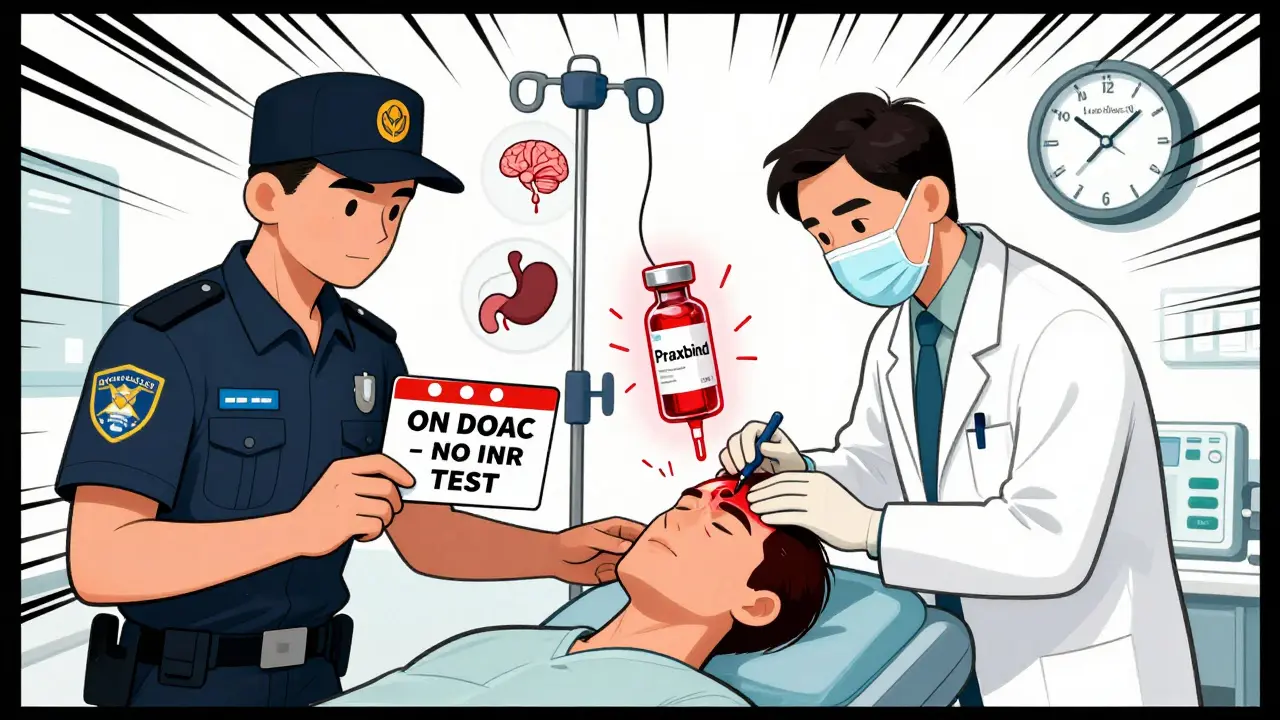
Reversing DOACs: What Happens If You Bleed?
This is a real concern. Warfarin can be reversed with vitamin K and fresh frozen plasma. DOACs? It’s harder.- Dabigatran: Can be reversed with idarucizumab (Praxbind). It works fast-in minutes.
- Rivaroxaban, apixaban, edoxaban: Can be reversed with andexanet alfa (Andexxa). But it’s expensive and not always available.
- No specific reversal agent?: Supportive care-pressure, transfusions, activated charcoal if taken recently, and sometimes prothrombin complex concentrate (PCC).
Cost and Access
Let’s be honest. Warfarin costs $10 to $30 a month in the U.S. DOACs? $500 to $700. That’s a big barrier. In Australia, PBS subsidies bring DOACs down to around $30 per script for concession card holders. If you’re paying full price, ask about patient assistance programs. Some manufacturers offer copay cards. But cost isn’t just about the pill. Warfarin adds up in lab fees, travel time, and missed work. DOACs save time-and maybe even lives.What’s Next?
The future of anticoagulation is personalized. Researchers are looking at genetic tests to predict how you’ll respond to warfarin. AI models are being trained to predict INR trends. But right now, the best tool is still the INR test-and following the guidelines. Switching from warfarin to a DOAC isn’t a quick fix. It’s a careful, step-by-step process. Do it right, and you’ll have fewer blood tests, less worry, and lower bleeding risk. Do it wrong, and the consequences can be deadly.Ask your doctor: What’s my INR today? What’s my kidney function? What’s the exact timing for switching? Write it down. Stick to it. Your life depends on it.
Can I switch from warfarin to a DOAC on my own?
No. Switching requires precise timing based on your INR, kidney function, and medical history. Only doctors or pharmacists trained in anticoagulation management should make this change. Doing it without supervision can lead to strokes, clots, or life-threatening bleeding.
Which DOAC is safest?
Apixaban has the lowest risk of major bleeding in most studies, including intracranial hemorrhage. Dabigatran carries a higher risk of stomach bleeding. Rivaroxaban may increase bleeding risk in older adults. But safety depends on your kidneys, weight, and other medications. There’s no single “best” DOAC-only the best one for you.
Do I still need blood tests after switching?
You won’t need INR tests anymore. But you still need kidney function tests every 6 to 12 months. DOACs are cleared by the kidneys. If your kidney function drops, your drug level can rise and increase bleeding risk. Liver tests may also be checked if you have other health conditions.
What if I take other medications like aspirin or NSAIDs?
Avoid NSAIDs like ibuprofen or naproxen if possible-they raise bleeding risk. Aspirin can be used in some cases, like after a heart attack, but only if your doctor approves. Many antibiotics and antifungals interact with DOACs. Always check with your pharmacist before starting any new medicine.
Can I drink alcohol while on a DOAC?
Moderate alcohol (1 drink per day for women, 2 for men) is usually fine. But heavy drinking can damage your liver and kidneys, which affects how your body processes the DOAC. It also increases bleeding risk. If you drink regularly, talk to your doctor. They may adjust your dose or recommend you cut back.
What if I need emergency surgery?
Tell the ER team you’re on a DOAC. Bring your medication list or alert card. If you took your last dose within 12 hours, they may use reversal agents like idarucizumab or andexanet alfa. If it’s been longer, they’ll manage bleeding with supportive care-fluids, transfusions, or clotting factors. Don’t wait to tell them.









9 Comments
The FDA is hiding the truth about DOACs. I’ve seen patients turn into walking zombies after switching - memory loss, internal bleeding they never reported, and then they vanish from the system. Who’s funding these trials? Big Pharma. They don’t care if you bleed out as long as the profit margin stays high. I’ve got documents. I’ve got emails. This isn’t medicine. It’s corporate euthanasia.
And don’t even get me started on reversal agents. Andexxa costs $50,000 a dose. You think your grandma’s gonna get that? Nah. She gets a saline drip and a prayer. Meanwhile, warfarin’s been saving lives since Nixon was president. Why fix what ain’t broke?
I’ve been tracking this since 2018. I’ve got 17 case studies. All with the same outcome: DOACs = silent killer. Your doctor’s just another pawn.
They told me my INR was ‘fine.’ Then I had a subdural. Now I walk with a cane. And they want me to trust a pill that can’t be reversed? No. No. NO.
I’m not paranoid. I’m informed. And if you’re switching without reading the black box warnings? You’re not brave. You’re dumb.
They’ll bury this thread. But I’ll be here. Waiting. Watching. Documenting.
Next time you fill a prescription, ask yourself: Who benefits?
Not you.
Wow. So many words. And yet not one sentence about how I’m supposed to afford this $700/month pill when my insurance says ‘nope’ and my job doesn’t cover it. Thanks for the novel, doc. Now can someone explain how I’m supposed to choose between food and my blood not turning into jelly?
This is one of the most thorough, clinically sound summaries of DOAC transition I’ve encountered in years. The emphasis on INR thresholds, renal clearance, and the moisture sensitivity of dabigatran is precisely the kind of detail that saves lives.
As a pharmacist with 18 years in anticoagulation clinics, I can confirm: the five-step protocol outlined here is gold-standard. The real challenge isn’t the science - it’s the execution. Too many primary care providers are handed a script and told to ‘just switch.’ No coordination. No follow-up. No printed schedule.
Patients need more than a pamphlet. They need a hand-holding plan. That’s why I always print out the dosing timeline, label the pills with the exact switch date, and schedule a 72-hour follow-up call. It’s extra work - but it’s the difference between a smooth transition and a trip to the ER.
Also, the note about NSAIDs is critical. I’ve seen too many patients take ibuprofen for ‘a little headache’ and end up with a GI bleed. Always check interactions. Always.
Thank you for writing this. It’s the kind of content that deserves to be pinned.
Oh, so now we’re trusting a pill that doesn’t need monitoring? How quaint. I suppose next they’ll tell us to just ‘trust your gut’ when it comes to chemotherapy.
Let me guess - the ‘guidelines’ were written by people who’ve never had to pay for a DOAC out of pocket. Or maybe they’ve never seen a 78-year-old with CrCl of 28 trying to swallow a capsule that costs more than their monthly rent.
And let’s not forget the ‘moisture-sensitive’ dabigatran. So now we’re supposed to babysit our meds like they’re fine china? Meanwhile, warfarin sits in a Ziploc bag for a decade and still works.
This isn’t progress. It’s pharmaceutical theater. You’re being sold convenience at the cost of your autonomy. And your wallet.
Next time someone tells you ‘it’s safer,’ ask them who’s paying for the reversal agent when it all goes sideways.
Switching from warfarin to a DOAC… it’s not just a medical decision. It’s a metaphysical one.
Warfarin demanded ritual - the blood draws, the calendar marks, the constant awareness of your body’s fragile equilibrium. It was a mirror. It forced you to confront your mortality, day after day.
DOACs? They offer oblivion. A silent, convenient surrender to the illusion of control. You take your pill, forget it exists, and pretend you’re not dancing on the edge of a cliff.
But here’s the truth: no pill can absolve you of your fragility. Whether it’s INR checks or kidney function tests, the body always demands its due.
Are we really better off when we outsource our awareness to a pharmacy? Or are we just numbing ourselves to the fact that life - real, messy, bleeding life - is still happening?
I miss warfarin. Not because it was easy. But because it made me feel alive.
Maybe that’s the real side effect they didn’t list: the quiet grief of losing the ritual that reminded you you were still here.
Just wanted to say - this is super helpful. I switched last year and didn’t know about the dabigatran moisture thing. I had it in a pill organizer for 3 months. My INR was fine, but my doctor freaked out when I told her. Turns out my dose was way too low. I’m on apixaban now and it’s been smooth. Just… don’t put your meds in plastic containers unless you know they’re safe. Learned the hard way.
Oh wow, so now we’re supposed to be scientists too? Calculate CrCl? Check INR? Remember if your last dose was 6 hours ago? Next they’ll want us to memorize the pharmacokinetics of each DOAC before we can breathe.
Meanwhile, my doctor handed me a script and said ‘take this, don’t die.’ That’s it. No spreadsheet. No flowchart. Just a pill and a prayer.
And yet somehow, I’m still alive. Who knew medicine could be this simple?
Also, I’m pretty sure my dog takes warfarin. He’s got atrial fibrillation. Probably from all the squirrels he chases. I’m just waiting for his insurance to cover Andexxa.
My uncle took apixaban and lived to 92. He forgot his pill twice a week. Never bled. Never clotted. Just kept gardening. Maybe the system’s not broken - maybe we’re just overcomplicating it. 🤷♂️
INR < 2.0 → start DOAC. Simple. Clear. No guesswork.
Don’t overthink it. Follow the guidelines. Your life depends on precision, not opinion.