FDA Manufacturing Inspections: What They Are and Why They Matter for Your Medications
When you take a pill, you trust it was made under strict rules. That trust comes from FDA manufacturing inspections, official checks by the U.S. Food and Drug Administration on drug factories to ensure they follow safety and quality standards. Also known as pharmaceutical facility audits, these inspections are the backbone of drug safety in the U.S.—whether the medicine is brand-name or a cheap generic. The FDA doesn’t just approve drugs; they watch how they’re made. A factory in India, China, or Pennsylvania must pass these inspections before your medication ever hits the shelf.
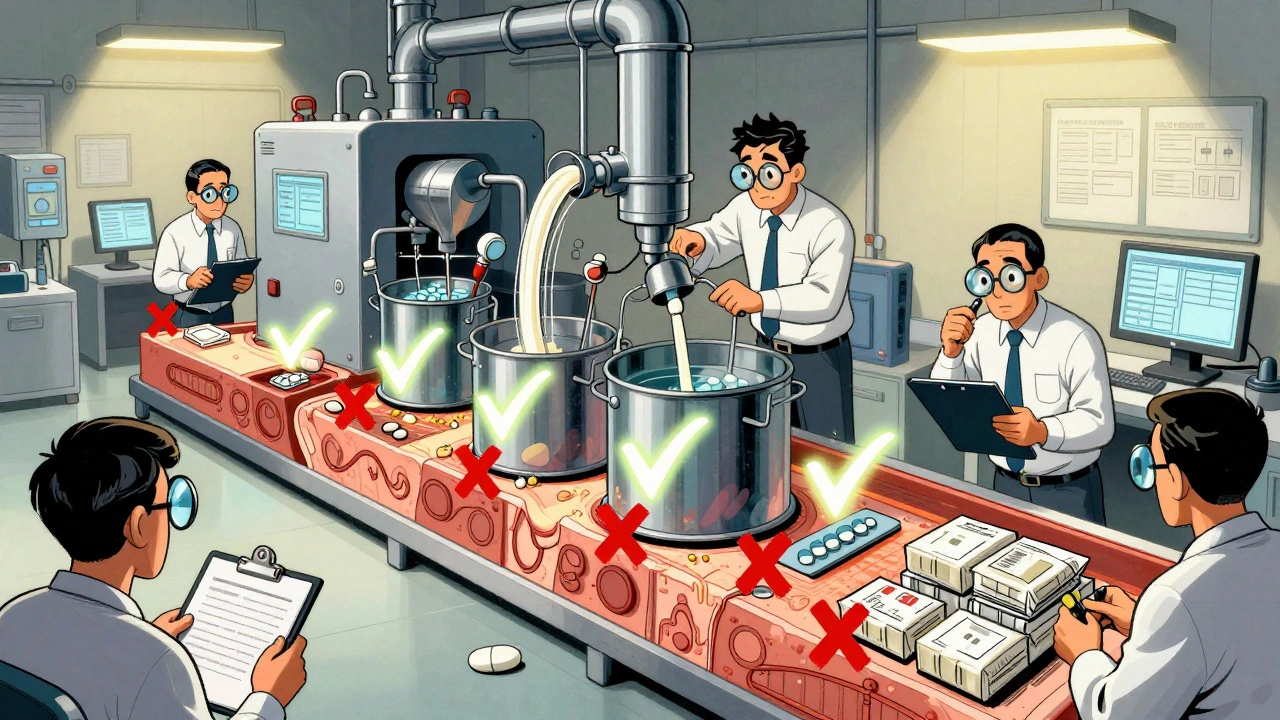
These inspections aren’t random. They target facilities that make high-risk drugs, have past violations, or supply products with known safety issues. The FDA looks at everything: how clean the equipment is, whether workers follow procedures, if records are falsified, and if raw materials are properly tested. One failed inspection can mean a drug recall, a supply shortage, or worse—patients getting pills that don’t work or contain harmful contaminants. In 2020, the FDA shut down a major Indian plant after finding fake test results for blood pressure meds. That’s not a hypothetical risk. It’s happened.
And it’s not just about big pharma. Generic drug makers, which supply over 90% of U.S. prescriptions, face the same scrutiny. But because they operate on thin margins, some cut corners. That’s why drug safety, the system that ensures medications work as intended and don’t harm users depends on these inspections. Without them, you’d have no way to know if your generic metformin or amoxicillin was made in a facility with mold in the vents or untrained staff mixing batches by guesswork.
FDA inspections, the on-site evaluations conducted by FDA investigators to verify compliance with Current Good Manufacturing Practices are public record. You can look up inspection reports online—though most people don’t. That’s a problem. These reports tell you if a factory was cited for failing to clean equipment between batches, or if they hid data from inspectors. One inspection found a plant using expired ingredients and labeling them as new. That’s not a mistake. That’s negligence.
And here’s the thing: inspections don’t always catch everything. Some factories get warned, fix the visible problems, and go back to old habits until the next visit. That’s why generic drug quality, the consistency and reliability of non-brand medications across different batches and manufacturers can vary—even when they’re labeled the same. The FDA’s post-market monitoring, like tracking adverse events from generics, helps fill the gaps. But it’s reactive. Inspections are proactive. They’re your first line of defense.
What you’ll find in the posts below are real stories tied to this system: how bad manufacturing led to drug shortages, why some generics cause unexpected side effects, and how the FDA tracks problems after pills are already in your medicine cabinet. You’ll see how batch variability, oversight failures, and corporate pressure shape what ends up in your bottle. This isn’t theory. It’s the hidden reality behind every prescription you fill. And if you’ve ever wondered why your generic pill looks different or works differently than last time—you now know where to start looking.