Blood Pressure Medication Timing Checker
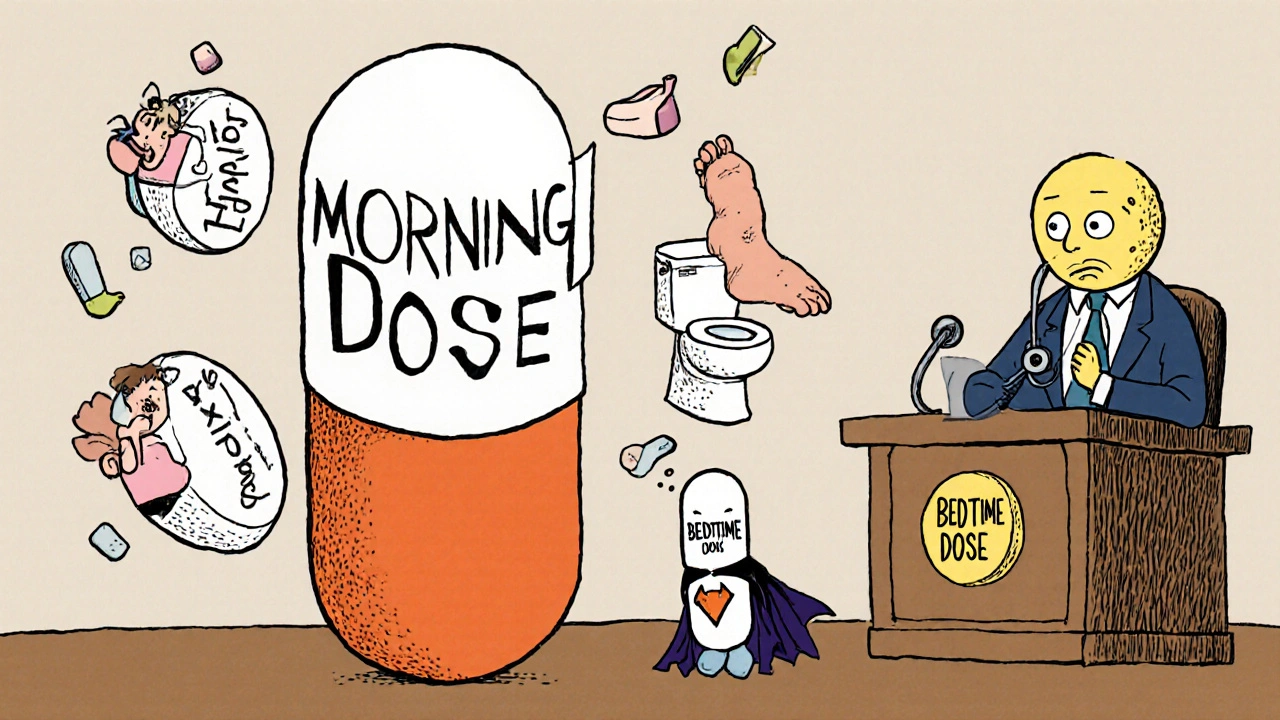
This tool helps you understand if switching your blood pressure medication to bedtime might reduce daytime side effects like dizziness, fatigue, and frequent bathroom trips.
Your Medication
Your Symptoms
Your Personalized Recommendation
Most people with high blood pressure take their medication in the morning because that’s what they’ve always been told. But what if taking it at night could stop the dizziness, fatigue, and frequent bathroom trips that ruin your workday? The answer isn’t simple - and it’s not one-size-fits-all. What matters most is how your body reacts to the timing, not the clock.
Why Timing Matters More Than You Think
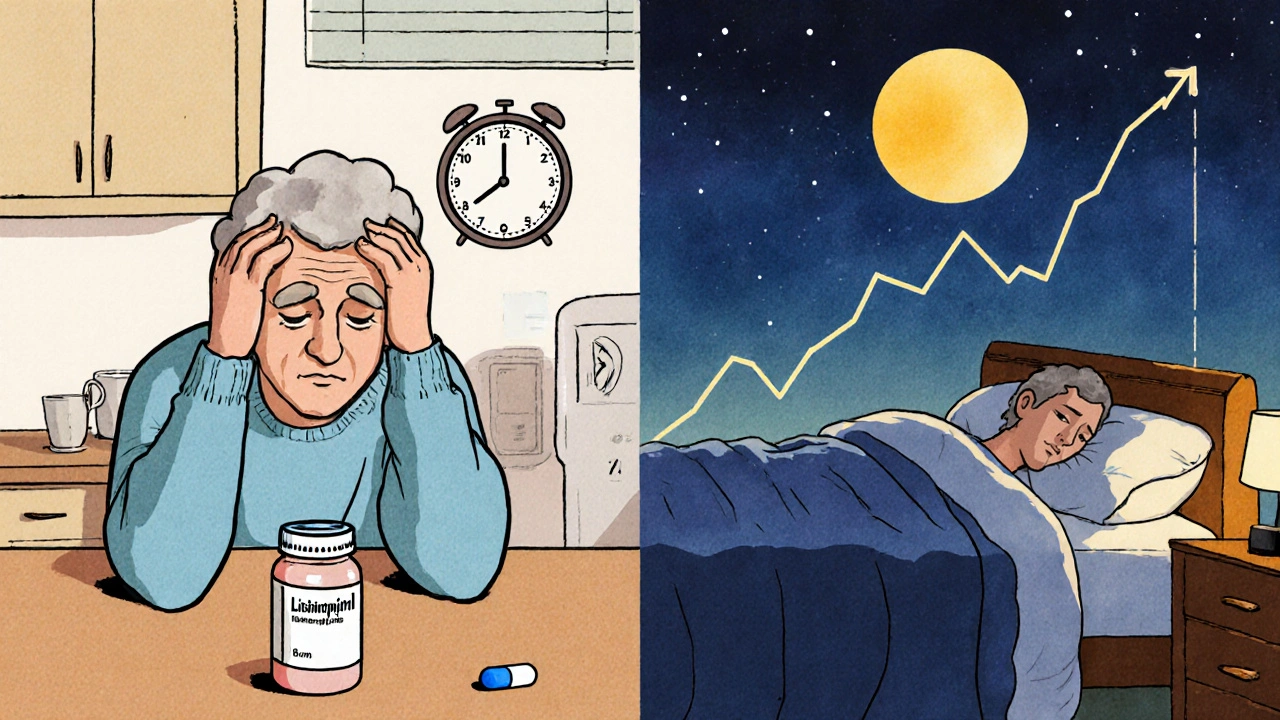
Your blood pressure doesn’t stay the same all day. It naturally drops while you sleep, then rises sharply in the early morning. That’s when heart attacks and strokes are most likely to happen. Some medications work better when they’re active during this risky window. But here’s the twist: if the drug peaks too early, you get side effects during the day - not when you need it most.Take lisinopril, for example. If you take it at 8 a.m., the drug hits its strongest level around noon. That’s when many people feel lightheaded, especially if they stand up quickly or walk to the mailbox. The same thing happens with amlodipine. That heavy, swollen-leg feeling? Often shows up a few hours after your morning pill.
Now, switch that same pill to bedtime. The drug works overnight, smoothing out your blood pressure curve. You’re less likely to feel dizzy during work, driving, or cooking. You might even sleep better because your body isn’t fighting a sudden pressure spike at dawn.
The Evidence: Does Bedtime Dosing Actually Help?
Large studies have looked at this for years. The BedMed trial, which followed over 3,300 people for nearly five years, found no big difference in heart attacks or strokes between morning and bedtime dosing. That’s the headline you’ll see in news articles. But dig deeper - and you’ll find something more useful.Even though outcomes were similar, the BedMed-Frail trial - focused on older adults in nursing homes - showed something important: the morning-dosing group had more reports of dizziness and lightheadedness. Not a huge difference, but enough that patients noticed it. One patient said, “I used to feel like I was going to pass out after breakfast. After switching to night, it vanished.”
The OMAN trial in China tested a common combo pill (olmesartan-amlodipine) and found no extra risk of dangerously low blood pressure at night. That’s key. A lot of people worry that taking meds at night will drop their pressure too low while sleeping. The data says: not usually.
And then there’s the TIME study. It found that while fracture rates were the same, the bedtime group had fewer falls. Not statistically significant? Maybe. But for someone who’s already shaky on their feet, even a small reduction matters.
Side Effects You Actually Care About
Let’s talk about the real reasons people stop taking their meds: side effects that interfere with life.- Dizziness: 62% of patients who report side effects say it’s dizziness. Of those, 78% say it hits 2-4 hours after their morning dose. That’s right in the middle of your workday or commute.
- Too many bathroom trips: Diuretics like hydrochlorothiazide make you pee. If you take them in the morning, you’re racing to the bathroom at meetings. Switching to bedtime cuts daytime visits from 40% to 36.4% - not a huge drop, but enough for some to prefer it.
- Swelling in legs or ankles: Amlodipine users often report this. Some find it worse at night, others say it’s better. It’s individual.
- Fatigue or brain fog: Some feel sluggish all day after a morning dose. Others say nighttime dosing leaves them clearer-headed.
Reddit threads are full of these stories. One user switched lisinopril to bedtime and stopped missing work. Another switched amlodipine to night and got swollen legs so bad they had to go back. There’s no universal rule. Your body is your guide.
Who Should Try Bedtime Dosing?
Not everyone needs to change. But if you’re dealing with these issues, bedtime dosing might help:- You feel dizzy or lightheaded after your morning pill
- You’re constantly rushing to the bathroom during the day
- You’ve been told you have “nocturnal hypertension” - meaning your blood pressure doesn’t drop enough at night
- You’re older, or have balance issues, and have had near-falls
- You’re non-adherent because side effects make you want to skip doses
If you’re on a diuretic or an ACE inhibitor like lisinopril or enalapril, bedtime dosing is often the first switch doctors suggest. Calcium channel blockers like amlodipine are trickier - they can cause swelling at night for some. Talk to your doctor before changing anything.
What About the Risks?
The biggest fear? Nighttime low blood pressure. But studies show it’s rare. The BedMed-Frail trial looked specifically at frail elderly patients - the group most at risk - and found no increase in dangerous drops overnight. The OMAN trial confirmed the same.Another concern: nighttime urination. If you already wake up to pee, adding a diuretic at night might make it worse. But here’s the trade-off: 41% of patients who switched to bedtime said they preferred the nighttime bathroom trips over daytime ones. They’d rather wake up once than be stuck in a meeting with an urgent need.
Cognitive decline? Worried that lowering blood pressure too much at night might hurt your brain? The BedMed-Frail trial checked this. No difference in memory or thinking between morning and bedtime groups.

What Do Doctors Recommend Now?
The American Heart Association says timing doesn’t affect heart attack risk. That’s true. But they also say: “If side effects are causing you to skip doses, change the timing.”Here’s what leading clinics are doing in 2025:
- Cleveland Clinic: “Take your first dose at bedtime until dizziness goes away, then switch to morning if you prefer.”
- British Heart Foundation: “Some medications make you dizzy at first. Take your first dose at night.”
- AAFP: “Choose timing based on your side effects, not a rule.”
- ESC 2024: “Take your pill when you’re least likely to forget.”
That last one is important. Adherence is the #1 problem in hypertension. If you forget your pill every morning because you’re rushing out the door, taking it at night - right before bed - might be the best choice, even if it doesn’t reduce side effects.
How to Test It Safely
Don’t just switch on your own. Talk to your doctor. But here’s how to approach it:- Write down your side effects: When do they happen? How bad are they?
- Ask your doctor if your medication is a good candidate for bedtime dosing. ACE inhibitors, ARBs, and diuretics usually are.
- Start the switch on a Friday night. That way, if you feel weird, you’re home.
- Track your symptoms for two weeks. Use a simple note on your phone: “Dizzy? Yes/No. Bathroom? # times.”
- Compare: Did daytime dizziness drop? Did nighttime urination spike?
- Go back to your doctor. If it helped, keep it. If not, switch back.
Some people feel better right away. Others need a few weeks. Give it time. And remember: if you feel faint, dizzy, or confused after switching - call your doctor. Don’t ignore it.
The Bottom Line
There’s no magic time to take your blood pressure pill. But there is a best time for you.If you’re tired of feeling dizzy at noon, or constantly dodging bathroom breaks during work, bedtime dosing might be the quiet fix you’ve been looking for. It won’t save your life - the studies don’t show that. But it might help you live better. And that’s worth trying.
Don’t accept side effects as normal. Ask your doctor: “Could taking this at night help me feel better during the day?” Most will say yes - and help you test it.
Can I switch my blood pressure medication from morning to bedtime on my own?
No. Never change your medication timing without talking to your doctor first. Some drugs can cause sudden drops in blood pressure, especially if you’re on multiple medications or have kidney issues. Your doctor can check if your specific pill is safe to take at night and help you monitor for side effects.
Will taking my blood pressure pill at night cause me to wake up to pee too often?
It might - especially if you’re on a diuretic like hydrochlorothiazide. But many patients find nighttime urination easier to manage than daytime disruptions. If you already wake up once or twice to pee, adding a nighttime dose might not make it worse. If you’re waking up three or more times, your doctor might suggest switching back or changing the medication.
Does bedtime dosing lower my risk of heart attack or stroke?
Large studies like BedMed and TIME show no significant difference in heart attacks or strokes between morning and bedtime dosing. The main benefit of bedtime dosing isn’t preventing events - it’s improving how you feel during the day. Better side effect control means you’re more likely to take your pills consistently, which does lower long-term risk.
Which blood pressure meds work best at night?
ACE inhibitors (like lisinopril), ARBs (like losartan), and diuretics (like hydrochlorothiazide) are often the best candidates for bedtime dosing. They tend to smooth out your blood pressure overnight and reduce daytime dizziness. Calcium channel blockers like amlodipine can cause leg swelling at night for some people, so they’re less predictable. Always check with your doctor.
I’m older and take several meds. Is bedtime dosing safe for me?
Yes - but carefully. The BedMed-Frail trial studied frail older adults in nursing homes and found no increase in falls, fractures, or dangerous low blood pressure with bedtime dosing. Still, older adults often take multiple drugs that can interact. Your doctor should review all your medications before changing timing. Watch for confusion, dizziness, or weakness after switching.
How long should I try bedtime dosing before deciding if it works?
Give it at least two weeks. Blood pressure medications can take time to stabilize in your system. Side effects like dizziness or swelling may improve after a few days, but full effects can take up to four weeks. Track your symptoms daily. If you feel worse or have new issues, contact your doctor sooner.
I’ve heard bedtime dosing helps with sleep. Is that true?
Not directly. But if you’re not waking up dizzy or needing to pee every hour, you’ll sleep better. Some patients report feeling more rested because they’re not fighting the morning blood pressure spike. It’s an indirect benefit - not a sleep aid, but a quality-of-life improvement.
What if I forget to take my pill at night?
If you miss a bedtime dose, don’t double up in the morning. Skip it and take your next dose at the regular time. Consistency matters more than perfect timing. If you forget often, consider a pill organizer or phone reminder. If you’re still struggling, talk to your doctor - they might switch you to a once-daily pill with a longer half-life.





11 Comments
Just take it at night. Done.
Let's be clear: the BedMed trial's null result on cardiovascular endpoints is precisely why we need to stop treating this like a clinical equivalence problem. The primary endpoint isn't mortality-it's functional autonomy. Dizziness-induced falls in the elderly are a leading cause of institutionalization, not death. The 36.4% reduction in daytime diuresis isn't statistically significant? That's because they're using parametric tests on ordinal patient-reported outcomes. Real-world impact ≠ p-value. If your patient can't finish a meeting without a bathroom pass, that's a clinical failure. Period.
i switched my amlodipine to night and my legs swelled up so bad i looked like i was wearing water wings. went back to morning. still get dizzy but at least my ankles dont look like balloons. maybe its just me idk
Oh wow. So after 20 years of medicine, we're finally admitting that maybe the patient's lived experience matters more than a randomized trial? Shocking. The real scandal? That this isn't standard practice. You want to reduce non-adherence? Stop treating patients like lab rats. Give them agency. Let them choose timing based on what makes them feel human. If your doctor doesn't get that, find a new one. This isn't rocket science-it's basic damn respect.
They're hiding something. Why does every study funded by Big Pharma say 'no difference'? But the moment someone switches to nighttime, they report feeling better? Coincidence? Nah. The FDA doesn't care if you're dizzy at work-they care if you die. But if you're too dizzy to drive, who's paying for your insurance claim? They want you to keep taking it, not feel good. This is about control, not care.
The question isn't whether bedtime dosing works better-it's whether we've been asking the wrong question entirely. We've reduced hypertension management to a pharmacological optimization problem when it's fundamentally a rhythm problem. The body isn't a machine that needs a fixed dose at a fixed hour. It's a symphony. The timing of medication should harmonize with circadian biology, not impose a rigid schedule on a dynamic system. The fact that we're only now recognizing this speaks to how deeply we've misunderstood the nature of chronic illness. It's not about curing-it's about coexisting.
I switched my lisinopril to bedtime after years of dreading lunchtime meetings because I felt like I was going to pass out. The first week I cried because I actually slept through the night without needing to pee. I didn’t think it was possible to feel this normal again. I’m 68 and I just went hiking with my grandkids. I didn’t need a miracle. I just needed to stop taking my pill at 7 a.m. and start taking it at 10 p.m. Why isn’t this the first thing doctors say? Why do we make people suffer for years before someone says, ‘Try it at night’? I’m so mad I wasted so much time. But also… so grateful I finally listened to my body.
bro i switched to night and now i wake up once to pee but i dont feel like a zombie at 2pm 😎💊 #lifechanger
Let’s be honest-the real reason this isn’t mainstream is because it requires patient involvement. Doctors love protocols. They hate individualized care. It’s easier to say ‘take it in the morning’ than to ask, ‘When do you feel worst?’ and then track symptoms for two weeks. The fact that the AAFP says ‘choose timing based on side effects’ is revolutionary. But who has the time or energy to advocate for themselves? This isn’t medical advice-it’s a social justice issue. If your side effects make you feel like a burden, you’re not broken. The system is.
They're testing this on 'frail elderly' but what about the NSAIDs? The beta blockers? The anticoagulants? Nobody talks about the drug interactions. What if your nighttime pill causes a dangerous drop when mixed with your arthritis med? The studies don't cover polypharmacy. They're just giving you a single drug and calling it science. But real people? We're on seven pills. This is dangerous. And they won't tell you because they don't want to admit they don't have answers.
MY HUSBAND SWITCHED TO BEDTIME AND NOW HE'S A NEW MAN. HE ACTUALLY TALKS TO ME AT DINNER. HE'S NOT GROANING. HE'S NOT FIDGETING. HE'S NOT ASKING IF WE CAN SKIP THE WALK BECAUSE HE'S 'TOO DIZZY'. I CRIED. I DIDN'T KNOW I COULD MISS SOMEONE WHO WAS STILL IN THE HOUSE. THIS ISN'T JUST MEDICINE. IT'S RELATIONSHIP RESCUE.