DOAC Kidney Function Calculator
Calculate Your Kidney Function
Accurate kidney function measurement is critical for safe DOAC dosing. The Cockcroft-Gault formula is the only method recommended by the FDA, AHA, ESC, and KDIGO for DOAC dosing guidance.
Enter your values above to see your creatinine clearance.
Note: This calculator uses the Cockcroft-Gault formula, which is the only recommended method for DOAC dosing. eGFR is not appropriate for determining DOAC doses in kidney impairment.
Why DOACs Need Special Care in Kidney Problems
Direct Oral Anticoagulants, or DOACs, are the go-to blood thinners for millions of people with atrial fibrillation. They’re easier to use than warfarin - no weekly blood tests, fewer food interactions, and more predictable results. But here’s the catch: if your kidneys aren’t working well, these same benefits can turn into serious risks. About 1 in 4 people on DOACs have some level of kidney impairment. And if you don’t adjust the dose correctly, you could end up with a life-threatening bleed - or worse, a stroke because the drug didn’t work.
The problem isn’t that DOACs are dangerous. It’s that they leave your body mostly through your kidneys. When kidney function drops, the drug builds up. Too much? Bleeding risk skyrockets. Too little? Clots form. It’s a tightrope walk. And unlike warfarin, where you can check your blood levels with a simple INR test, DOACs don’t have a routine monitoring tool. That means getting the dose right the first time isn’t optional - it’s critical.
Which DOACs Are Safe, and Which Are Risky?
Not all DOACs are created equal when it comes to kidney function. Four are approved for atrial fibrillation: apixaban, rivaroxaban, dabigatran, and edoxaban. Each has different rules for kidney impairment.
- Apixaban (Eliquis) is the safest for people with poor kidneys. It’s the only DOAC that doesn’t require a dose change just because of kidney function alone. Even if you’re on dialysis, apixaban can still be used - as long as you meet the other criteria: age 80 or older, weight under 60 kg, or creatinine above 133 μmol/L. Then you drop from 5 mg twice daily to 2.5 mg twice daily. It’s the only DOAC with real-world data showing lower bleeding rates than warfarin in end-stage kidney disease.
- Rivaroxaban (Xarelto) is not recommended if your creatinine clearance falls below 15 mL/min. That’s stage 5 chronic kidney disease or dialysis. Studies show it builds up dangerously in these patients. Many cardiologists avoid it entirely if CrCl is under 30 mL/min.
- Dabigatran (Pradaxa) is mostly cleared by the kidneys. If your CrCl is between 15 and 30 mL/min, reduce the dose to 75 mg twice daily. Below 15 mL/min? Don’t use it. The risk of bleeding jumps sharply.
- Edoxaban (Savaysa) gets cut in half if CrCl is between 15 and 50 mL/min - from 60 mg to 30 mg daily. Below 15 mL/min? Avoid it. It’s less effective in advanced kidney disease, and the bleeding risk isn’t worth it.
Here’s the bottom line: if you have advanced kidney disease, apixaban is your best bet. The others carry higher risks. Many doctors still prescribe rivaroxaban or dabigatran in CKD patients - often because they forget the rules. That’s a mistake.
How to Calculate Your Kidney Function - The Right Way
You might think your doctor checks your eGFR to decide your dose. They shouldn’t. That’s a common error.
eGFR is great for tracking general kidney health. But for DOAC dosing, you need creatinine clearance (CrCl) calculated using the Cockcroft-Gault formula. The FDA, AHA, ESC, and KDIGO all say so. Why? Because eGFR underestimates kidney function in older, thinner, or muscle-wasted patients - exactly the people on DOACs.
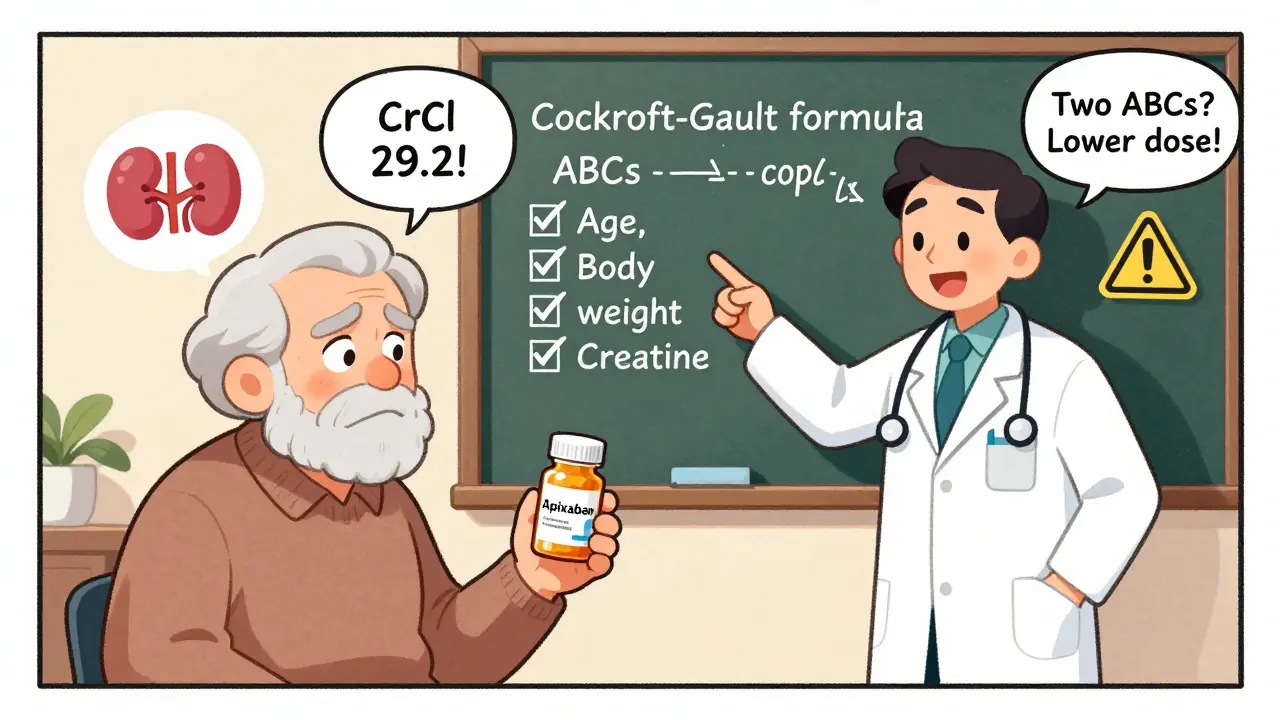
The Cockcroft-Gault formula looks like this:
CrCl (mL/min) = [(140 - age) × weight (kg) × (0.85 if female)] / (72 × serum creatinine in mg/dL)
Let’s say you’re a 78-year-old woman, weighing 55 kg, with a creatinine of 1.4 mg/dL:
CrCl = [(140 - 78) × 55 × 0.85] / (72 × 1.4) = [62 × 55 × 0.85] / 100.8 = 29.2 mL/min
That’s severe kidney impairment. For apixaban, you’d drop to 2.5 mg twice daily. For rivaroxaban? You shouldn’t be on it at all.
Most electronic health records auto-calculate eGFR. But they rarely auto-calculate CrCl. That means your doctor or pharmacist has to do it manually. If you’re over 70, under 60 kg, or have low muscle mass - ask them to double-check the CrCl. Don’t assume it’s right.

The ABCs of Apixaban Dosing
Apixaban is the most forgiving DOAC - but only if you follow the rules. The ABCs mnemonic helps remember when to reduce the dose:
- Age ≥80 years
- Body weight ≤60 kg
- Creatinine ≥133 μmol/L (1.5 mg/dL)
If you meet any two of these, reduce apixaban from 5 mg twice daily to 2.5 mg twice daily. Even if your CrCl is above 30 mL/min, you still need the lower dose.
I’ve seen patients on full-dose apixaban who are 82, weigh 58 kg, and have a creatinine of 1.6 - and they’re bleeding. They didn’t meet the full criteria for kidney failure, but they met two of the three ABCs. That’s enough to double the bleeding risk.
Doctors sometimes miss this because they focus only on CrCl. But the FDA label says: use the ABCs. It’s not optional. It’s built into the prescribing information for a reason.
What Happens When Doses Are Wrong?
Wrong DOAC dosing in kidney patients isn’t rare - it’s common. A 2022 study in JAMA Internal Medicine found that 37.2% of DOAC prescriptions in CKD patients were dosed incorrectly. That’s nearly 4 in 10.
Most errors? Too high a dose. People assume “more is better” for preventing clots. But with DOACs, that’s deadly. In one case, a 78-year-old man on dialysis was prescribed 5 mg of apixaban twice daily. He had no signs of kidney failure - just low weight and old age. He bled into his stomach. He nearly died.
On the flip side, some patients get too low a dose. I’ve seen elderly patients with CrCl of 25 mL/min put on 2.5 mg of apixaban - but they’re only 65, weigh 75 kg, and have no other risk factors. They’re at higher risk of stroke because the drug isn’t working.
The consequences are brutal: intracranial hemorrhage, gastrointestinal bleeding, clots in the lungs or legs. And once it happens, reversing DOACs is harder than reversing warfarin. There’s an antidote for dabigatran (idarucizumab), and one for apixaban/rivaroxaban (andexanet alfa) - but they’re expensive, not always available, and don’t guarantee survival.

What About Dialysis Patients?
There’s no perfect answer here. The evidence is thin. Most trials excluded dialysis patients. But real-world data is growing.
A 2023 report from nephrologists in the U.S. found that apixaban 2.5 mg twice daily was used safely in over 120 dialysis patients with atrial fibrillation. Major bleeding was 1.8% per year - lower than warfarin’s 3.7%. No strokes occurred in that group.
That’s why the American Heart Association and American College of Cardiology now say apixaban is an option for dialysis patients. Warfarin is still used, but it’s not better. In fact, warfarin causes more bleeding and more calcium buildup in blood vessels in kidney failure.
Don’t expect a magic number. Some dialysis patients get apixaban 2.5 mg once daily. Others get it twice. There’s no official guideline. But the trend is clear: apixaban at 2.5 mg twice daily is the most supported choice.
What You Can Do - A Simple Checklist
If you’re on a DOAC and have kidney disease, here’s what to ask your doctor:
- What’s my creatinine clearance (CrCl) using the Cockcroft-Gault formula? (Not eGFR.)
- Do I meet any two of the ABCs for apixaban? (Age 80+, weight ≤60 kg, creatinine ≥1.5 mg/dL.)
- Is my DOAC dose approved for my level of kidney function?
- Am I on a DOAC that’s even recommended for my stage of kidney disease? (Avoid rivaroxaban and dabigatran if CrCl <30.)
- Will my dose be checked every 3-6 months? Kidney function changes - especially in older adults.
Write this down. Bring it to your next appointment. If your doctor says, “We just use eGFR,” ask them to check the AHA or KDIGO guidelines. They’re out there. And they’re clear.
The Future: What’s Coming Next?
By 2026, we’ll have better answers. Two major trials are wrapping up:
- RENAL-AF is comparing apixaban to warfarin in patients with severe kidney disease. Results expected in 2025.
- AXIOS (though it ended early) will release data on apixaban in dialysis patients in late 2024.
Right now, we’re making decisions with incomplete data. But we’re not flying blind. We have enough evidence to know what works - and what doesn’t.
By 2026, apixaban will likely be the only DOAC routinely recommended for advanced kidney disease. The others? They’ll be restricted to mild or moderate impairment. And warfarin? It’ll still be used - but only when DOACs aren’t an option.
The message is simple: if you have kidney problems, don’t assume your DOAC dose is right. Ask for the CrCl. Know the ABCs. Choose apixaban if you can. And never let someone use eGFR to make this decision.