Drug Safety: What You Need to Know About Medication Risks and Protection
When you take a pill, you trust it will help—not harm. But drug safety, the practice of preventing harm from medications through proper use, monitoring, and awareness. Also known as medication safety, it's not just about following labels—it's about understanding hidden risks, unexpected reactions, and what happens after the pharmacy door closes. Every year, thousands end up in emergency rooms not because they took too much, but because they didn’t know a common painkiller could clash with their blood pressure pill, or that a generic version might contain an inactive ingredient that triggered a rash. Drug safety isn’t a one-time check. It’s a chain: from how a drug is made, to how it’s prescribed, to what your body does with it.
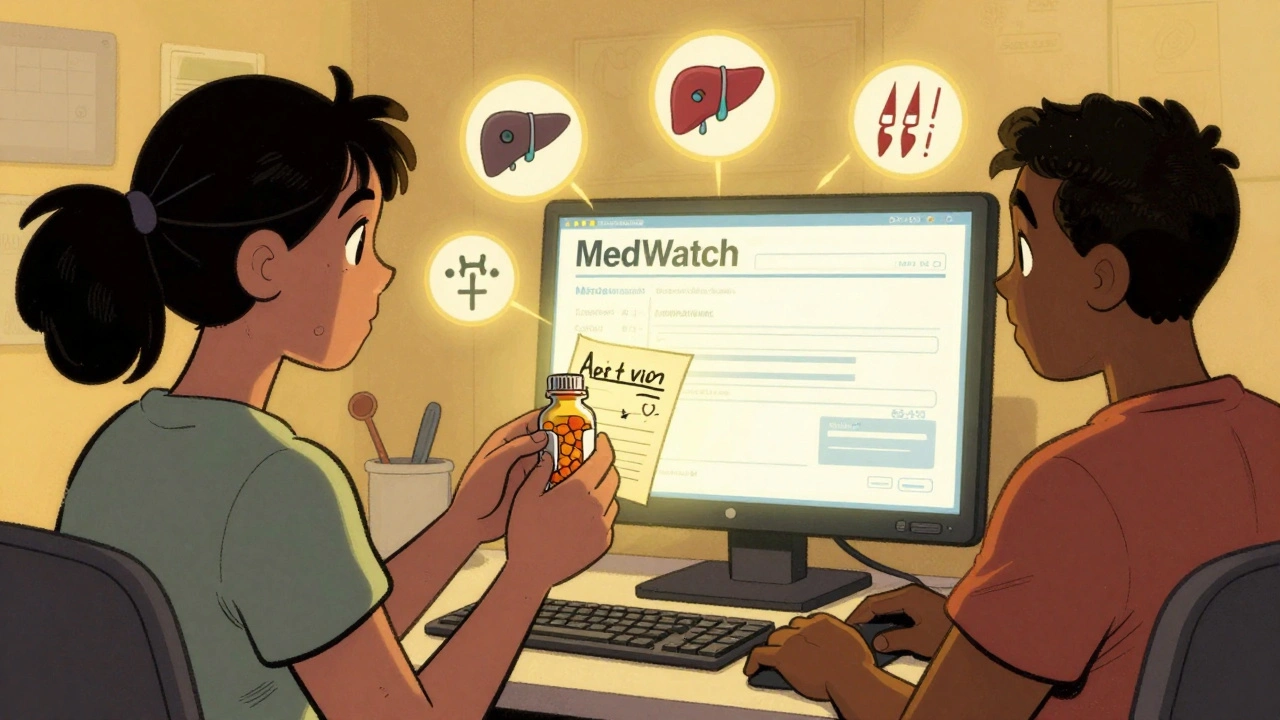
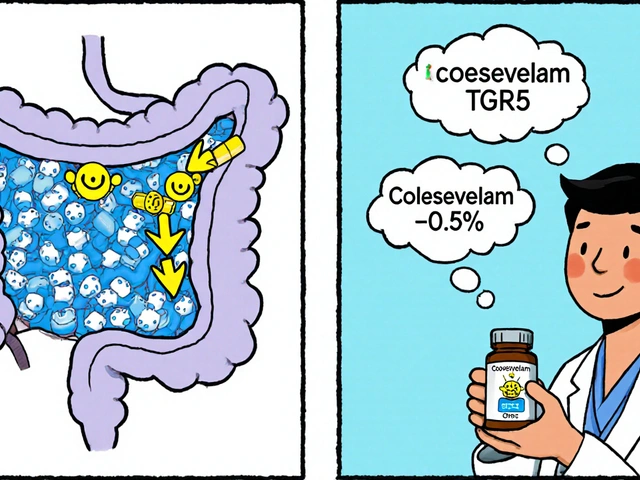
One major piece of this chain is reversal agents, special drugs designed to undo the effects of anticoagulants and other high-risk medications in emergencies. Think of them as emergency brakes for blood thinners—idarucizumab for dabigatran, andexanet alfa for factor Xa inhibitors. These aren’t just hospital tools; they’re life-saving options when someone bleeds internally after a fall or surgery. Then there’s medication overdose, a preventable crisis where the body can’t process a drug safely. Naloxone reverses opioid overdoses in minutes. NAC can save your liver after an acetaminophen mistake. These antidotes work fast—but only if you know they exist and where to find them. And while we’re on the topic of generics, don’t assume they’re risk-free. generic drug safety, the ongoing monitoring of lower-cost versions of brand-name drugs for hidden side effects and variability. The FDA tracks them after approval, but batch differences, filler ingredients, and manufacturing shifts can change how a pill behaves in your body. That’s why some people report strange side effects with a generic even when the active ingredient matches the brand.
Drug interactions aren’t always obvious. Cinnarizine and alcohol? A dangerous combo. High-protein meals blocking Parkinson’s meds? A silent motor crash. Even herbal remedies like Rumalaya can interfere with prescription drugs you didn’t even think to mention to your doctor. And when supply chains break—like during COVID—drug shortages force people onto unfamiliar substitutes, increasing the chance of error. Drug safety isn’t just about avoiding bad pills. It’s about knowing when timing matters, when to question a refill, and when to speak up if something feels off. You don’t need to be a pharmacist to protect yourself. You just need to know what questions to ask.
Below, you’ll find real-world stories and science-backed guides on exactly how these risks show up—and how to stop them before they hurt you. From reversing blood thinners in emergencies to spotting dangerous interactions in everyday meds, these posts cut through the noise and give you what actually works.