When a teenager starts taking an antidepressant, parents often face a terrifying choice: risk untreated depression or risk a medication that might increase suicidal thoughts. The FDA’s black box warning on antidepressants for children and teens has made this decision even harder. Since 2005, every prescription bottle of fluoxetine, sertraline, escitalopram, and other antidepressants has carried a bold, black-bordered warning: antidepressants increase the risk of suicidal thinking and behavior in children and adolescents. It’s the strongest safety alert the FDA can issue. But what does that really mean? And has it helped-or hurt-kids more than it’s protected them?
What the Black Box Warning Actually Says
The FDA’s black box warning doesn’t say antidepressants cause suicide. It says they may increase the risk of suicidal thinking and behavior-called suicidality-in young people under 25. This warning came after a review of 24 clinical trials involving over 4,400 children and teens with depression, OCD, or anxiety. In those studies, about 4% of kids on antidepressants showed signs of increased suicidal thoughts or behaviors, compared to 2% on placebo. No one died in those trials. But the difference was enough for the FDA to act.
The warning applies to all prescription antidepressants, not just SSRIs. That includes fluoxetine (Prozac), sertraline (Zoloft), escitalopram (Lexapro), venlafaxine (Effexor), and others. The language on the label is strict: "Anyone considering the use of an antidepressant in a child or adolescent must balance the risk of increased suicidality with the clinical need." It also says patients should be watched closely for worsening depression, agitation, or unusual behavior-especially in the first few weeks of treatment.
Along with the warning, pharmacists are required to hand out a MedGuide to every patient and caregiver. It explains the risk in plain language. But here’s the problem: the warning doesn’t say how often to monitor, what signs to look for, or who’s most at risk. It’s a blanket alert for every kid, regardless of their history, severity of depression, or family support.
The Unintended Consequences
What happened after the warning went into effect? Prescriptions dropped. Fast.
In the two years after the 2005 warning, antidepressant prescriptions for 10- to 19-year-olds fell by 31%. That’s over a million fewer prescriptions a year. By 2007, after the warning was expanded to include young adults up to age 24, prescriptions for that group dropped another 24.5%. Meanwhile, diagnoses of depression in teens actually went up by 14% during the same time.
And then the suicide rates started climbing.
From 2003 to 2007, the suicide rate among 10- to 19-year-olds in the U.S. jumped from 2.0 to 3.5 per 100,000-a 75% increase. A 2023 study in Health Affairs that tracked 1.1 million adolescents found that the number of psychotropic drug poisonings (a strong proxy for suicide attempts) rose by 21.7% after the 2005 warning. Among young adults 20-24, the spike was even higher: 33.7%. These weren’t random fluctuations. The same spike didn’t happen in adults over 25, who weren’t affected by the warning.
Researchers like Dr. Stephen Soumerai from Harvard Pilgrim Health Care Institute say the evidence is clear: when you scare families away from treatment, kids with severe depression get worse. A 2021 study from Sweden looked at 845 suicides among 10- to 19-year-olds before and after the warning. The authors found no drop in suicide after the warning-only an increase. Their conclusion? The warning may have left suicidal teens without the treatment that could have saved them.
What Parents Are Really Thinking
On Reddit’s r/mentalhealth, a thread titled "FDA Black Box Warning on Antidepressants for Teens-Should I be worried?" had 287 comments. Two-thirds of parents said they were too scared to fill the prescription. One wrote: "My daughter’s therapist said she needed medication, but I couldn’t sleep at night thinking I might be putting her in danger."
A survey of 1,243 parents on HealthUnlocked found that 74% delayed or refused antidepressants because of the warning. The most common reason? "Fear of making suicidal thoughts worse."
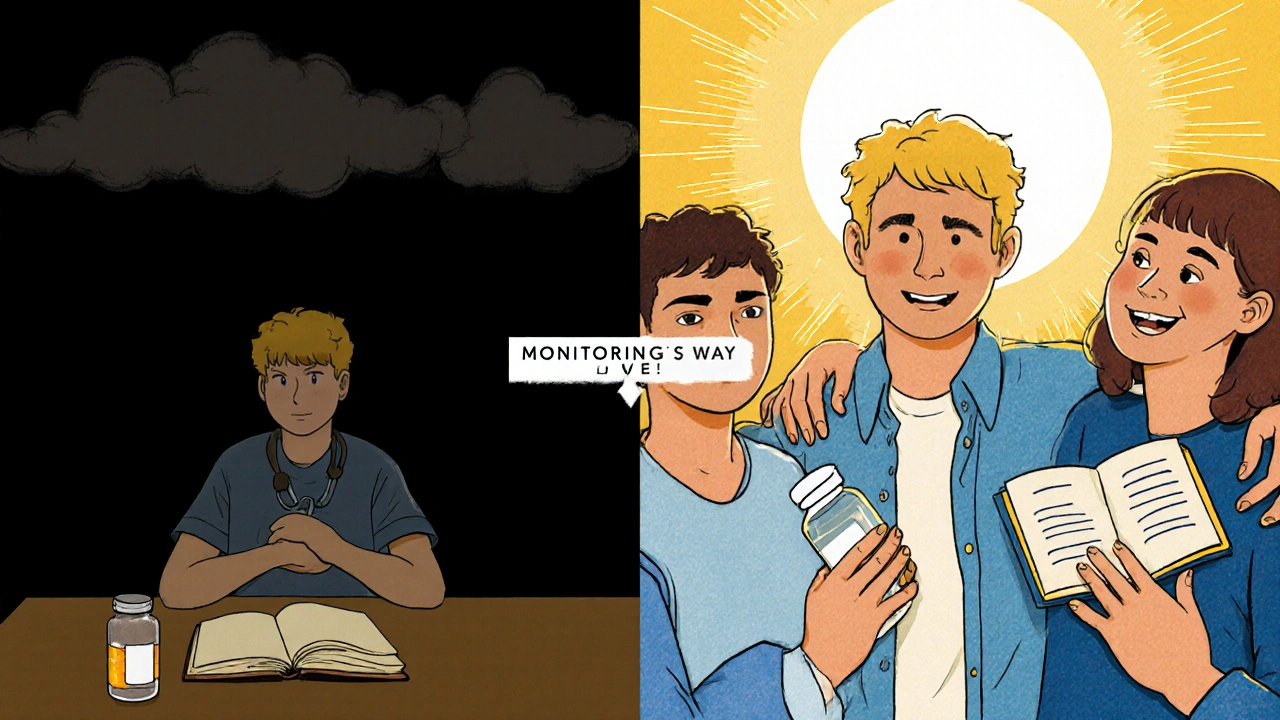
But here’s what those same parents didn’t always hear: the warning was never meant to stop treatment. It was meant to make it safer. The FDA’s goal was to ensure that kids on antidepressants got more check-ins, not fewer. A 2021 survey by NAMI found that 67% of families who did start treatment despite the warning reported positive outcomes. Many said the warning made them more alert. One parent said: "We checked in every day. We noticed she was quieter after two weeks. We called the doctor right away. That saved her."

How Doctors Are Struggling
Child psychiatrists are caught in the middle.
A 2019 survey of 1,200 child psychiatrists found that 87% said the warning made prescribing harder. Parents now demand extra appointments just to talk about the warning. The average time spent explaining it jumped from 8 minutes to over 22 minutes per visit. Nearly all psychiatrists now require signed consent forms specifically about the black box warning.
And the monitoring guidelines? They’re nearly impossible to follow. The American Psychiatric Association says kids should be checked weekly for the first month, then every two weeks for the next month. But a 2020 study in JAMA Network Open found that only 37% of teens actually got that level of follow-up. In rural areas, it was as low as 22%.
Many doctors now avoid prescribing antidepressants altogether. One psychiatrist in Ohio told me: "I’d rather see a kid get worse slowly than risk a lawsuit or a bad outcome. It’s not what I went to med school for, but it’s what I’m forced to do."
The Global Picture
The U.S. isn’t alone in warning about antidepressants-but it’s the only country with this exact black box.
Health Canada has a similar warning, but it includes a line that says: "The benefits of antidepressants may outweigh the risks for some patients." The European Medicines Agency never issued one. And guess what? European countries didn’t see the same spike in youth suicides after 2005.
That’s not a coincidence. A 2022 position statement from the American College of Neuropsychopharmacology called for a reassessment of the warning, pointing out that countries without it didn’t experience the same drop in treatment or rise in suicide.
What’s Next?
The FDA held a public meeting in September 2023 to review the latest data. No decision has been made yet. But pressure is building. Pharmaceutical companies like Eli Lilly and Pfizer have asked the FDA to change the warning. Researchers at the National Institute of Mental Health are working on tools to predict which teens are most at risk-so we can stop using a sledgehammer when we need a scalpel.
For now, the warning stays. But here’s what matters most: the data shows that untreated depression kills. The warning was meant to save lives. But if it’s causing more kids to go without treatment, then it’s doing the opposite.
The real question isn’t whether antidepressants carry risk. They do. But the bigger question is: does the warning help more than it harms? The evidence says no. And if we keep ignoring that, we’re not protecting kids-we’re abandoning them.
What You Can Do Right Now
- Don’t refuse medication out of fear. Talk to your doctor about the actual risk. The increase in suicidality is small-2 percentage points. The risk of untreated depression is far higher.
- Ask for a monitoring plan. Make sure your child has weekly check-ins for the first month. Use a mood tracker app or journal to note changes in sleep, energy, or talk of hopelessness.
- Know the warning signs. Sudden withdrawal, rage, agitation, or talking about death aren’t normal side effects. Call the doctor immediately.
- Don’t stop meds suddenly. Stopping antidepressants abruptly can cause withdrawal symptoms and worsen depression. Always taper under supervision.
- Combine meds with therapy. CBT and other talk therapies reduce relapse and improve outcomes. Medication alone isn’t the full solution.
The black box warning isn’t going away tomorrow. But you don’t have to let it control your choices. With the right support, antidepressants can be life-saving. The goal isn’t to avoid risk-it’s to manage it wisely.
Do antidepressants cause suicide in teens?
No, antidepressants do not cause suicide. The FDA’s black box warning states they may increase the risk of suicidal thoughts or behaviors-called suicidality-in a small number of children and teens. In clinical trials, about 4% of kids on antidepressants showed signs of suicidality compared to 2% on placebo. No deaths occurred in those trials. The warning exists to ensure closer monitoring, not to discourage treatment.
Why did suicide rates go up after the warning?
After the black box warning was issued in 2005, antidepressant prescriptions for teens dropped by 31%. Research shows that when teens with severe depression go without treatment, their risk of suicide increases. Studies found a 21.7% rise in psychotropic drug poisonings (a proxy for suicide attempts) and a 75% increase in youth suicide rates between 2003 and 2007. The warning may have scared families away from treatment, leading to worse outcomes.
Should I avoid antidepressants for my child?
Not necessarily. Untreated depression carries a much higher risk of suicide than antidepressants. For many teens, medication combined with therapy is the most effective treatment. The key is to work with a doctor who understands the warning and will monitor your child closely during the first few weeks. If your child has severe depression, anxiety, or thoughts of self-harm, avoiding treatment can be dangerous.
How long should my child be monitored after starting antidepressants?
The American Psychiatric Association recommends weekly check-ins for the first month, then every two weeks for the next month, and then regular follow-ups. Real-world data shows this isn’t always followed, but it’s the standard of care. Parents should be actively involved-tracking mood, sleep, energy, and any talk of hopelessness. If your child gets worse or shows new behaviors like agitation or withdrawal, call the doctor immediately.
Are there safer alternatives to antidepressants for teens?
For mild to moderate depression, therapy alone-especially cognitive behavioral therapy (CBT)-can be very effective. But for severe depression, suicidal thoughts, or when therapy hasn’t worked, medication is often necessary. There’s no proven alternative that works as reliably for severe cases. The best approach is often a combination of therapy and medication, with close monitoring. Avoiding treatment because of fear can lead to worse outcomes.










14 Comments
Antidepressants dont cause suicide dumbass the warning is for monitoring not avoidance
Exactly. Fear shouldn't override medical advice. My cousin started on sertraline and her mood stabilized within weeks. We monitored her closely. It worked.
Yessss this!! 🙌 I'm a therapist and I've seen too many kids suffer because parents panicked over a black box. Medication + therapy = life-saving combo. 📈💙
Interesting how you ignore that the 2% placebo group also had suicidal ideation. The FDA’s data is cherry-picked. And why is it only US and Canada with this warning? Coincidence? I think not.
Let us not forget the pharmaceutical industry’s influence on the FDA’s decision-making apparatus. The black box warning was never about safety-it was about liability mitigation disguised as public health policy. The data shows correlation, not causation, and yet the narrative is weaponized.
Oh, so now we’re blaming Big Pharma for the rise in teen suicide rates? How quaint. The real villain here is the refusal to accept that mental illness is medical, not moral. We’ve turned a clinical tool into a moral panic-and kids are dying because we’re too scared to be rational.
Have you ever sat in a waiting room with a teenager who just whispered, 'I don’t want to wake up tomorrow'? I have. And then I watched their parent hand back the prescription because of a black box warning. That’s not fear-that’s negligence dressed up as caution. The system failed them. Again. And now the kid’s in a hospital bed. Again. And the doctor’s too scared to prescribe again. Again. When does it end?
just a heads up-weekly check ins are ideal but most families cant afford them. insurance barely covers 1 visit a month. so the warning is good but the support system isnt there. its like telling someone to run a marathon but taking away their shoes.
The pharmacokinetic profiles of SSRIs in adolescent populations necessitate heightened vigilance during the initial titration phase due to neurodevelopmental variability in CYP450 enzyme expression. The black box is a risk mitigation protocol, not a contraindication.
Why are we even having this conversation? The FDA has been wrong before. Thalidomide. Vioxx. Now this. They’re bureaucrats, not doctors. Let the doctors decide. Not a panel of lawyers and statisticians.
You people are reckless. You think it's 'just depression'-but suicide is permanent. One mistake and your child is gone. No second chances. I'd rather have a depressed child alive than a dead one who was 'treated properly.' You're playing God with lives.
The Swedish study referenced is methodologically flawed. Its cohort lacked control for socioeconomic confounders and did not adjust for changes in diagnostic criteria post-2005. The conclusion is not statistically robust.
I’m a parent. My daughter was suicidal. We started her on fluoxetine. We checked in every day. We kept a journal. We called the doctor when she got quiet. She’s okay now. The warning didn’t scare me away-it made me more careful. That’s what it’s for.
It's not about the warning. It's about the absence of mental health infrastructure. No therapists. No school counselors. No funding. The black box is a distraction. We're treating symptoms while the house burns down.