Bioequivalence Standards: What Makes Generic Drugs Truly Equal
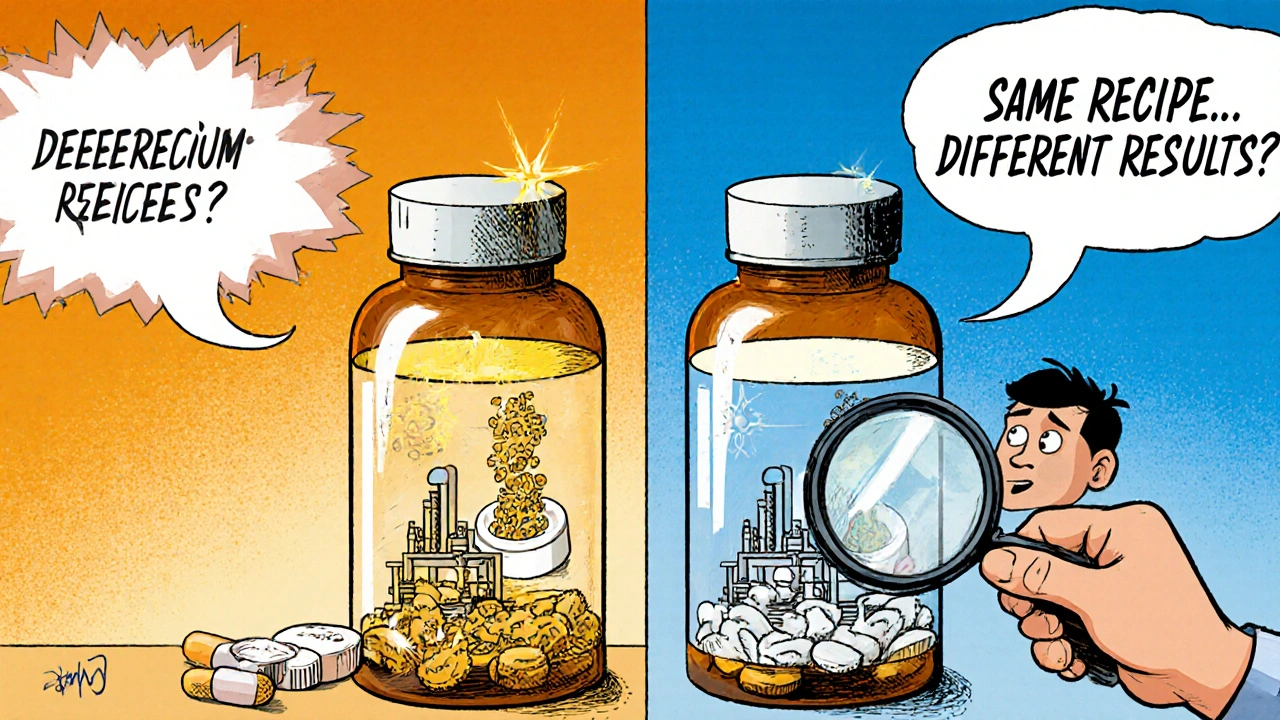
When you pick up a generic pill, you’re counting on it to do the same job as the brand-name version. That’s not guesswork—it’s enforced by bioequivalence standards, a set of scientific rules that prove a generic drug releases the same amount of active ingredient into the body at the same rate as the original. Also known as drug equivalence criteria, these standards are the reason your pharmacist can legally swap your prescription without your doctor’s approval. But here’s the catch: just because two pills have the same active ingredient doesn’t mean they feel the same. Bioequivalence isn’t about chemistry alone—it’s about how your body absorbs and uses the drug. The FDA and other global regulators require generics to show they deliver between 80% and 125% of the brand’s blood concentration levels. That’s a tight window. If a generic falls outside it, it doesn’t get approved.
Behind every approved generic is a clinical study—usually done on healthy volunteers—measuring blood levels over time. These aren’t theoretical numbers. They’re real, measured results from people who took the drug and had their blood drawn repeatedly. The same applies to extended-release versions: if the brand releases the drug slowly over 12 hours, the generic must match that pattern exactly. This is why some people notice differences—not because the active ingredient changed, but because the inactive ingredients, fillers, coatings, and binders that help the pill dissolve or stay stable can affect how quickly the drug enters your system. A pill with a thicker coating might delay absorption just enough to cause a slight change in how you feel, especially with drugs that have narrow therapeutic windows, like warfarin or thyroid meds.
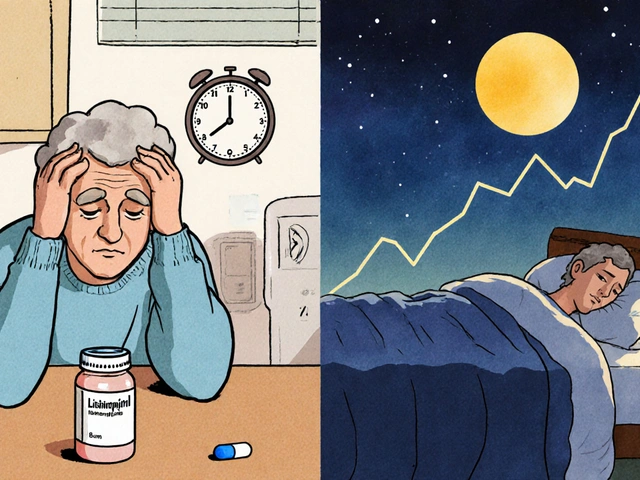
These standards don’t just protect patients—they keep the system running. Without them, pharmacies couldn’t reliably substitute generics, and drug costs would stay sky-high. But they also explain why some patients still distrust generics. If you’ve ever switched from brand to generic and felt off, it’s not all in your head. The pharmaceutical standards, the rules governing how drugs are tested and approved are strict, but human bodies aren’t perfectly uniform. That’s why doctors and pharmacists now track patient feedback more closely, especially for conditions like epilepsy or heart disease where tiny changes matter. The system works—but it’s not perfect. And that’s why you’ll find real stories in the posts below: people who had unexpected reactions, others who saved hundreds without issue, and the science that explains why both can be true.
What follows isn’t just a list of articles. It’s a collection of real-world experiences and clear explanations about how generic drugs behave in the body, why some cause side effects others don’t, and how to know when a switch is safe—or when you should push back. Whether you’re managing high blood pressure, depression, or chronic pain, understanding bioequivalence standards helps you ask the right questions and make smarter choices about your meds.