Every year, tens of thousands of people end up in the emergency room because they took too much acetaminophen - not because they meant to, but because they didn’t realize how easy it is to go over the limit. You might think of acetaminophen as harmless. It’s in your medicine cabinet, sold next to aspirin, and labeled "extra strength" like it’s just a stronger version of the same thing. But here’s the truth: acetaminophen is one of the most dangerous drugs you can take if you don’t know the rules. It’s safe when used right. Deadly when used wrong. And most people have no idea how close they are to crossing the line.
Why Acetaminophen Is So Easy to Overdose On
Acetaminophen (also called paracetamol) is in more than 600 different medicines. That’s not a typo. It’s in your pain reliever, your cold medicine, your sleep aid, your prescription opioid combo like Vicodin or Percocet, and even some herbal supplements. The problem isn’t the drug itself - it’s how hidden it is. You take one Tylenol for a headache. Then you take a cold tablet because you’re congested. Then you take another Tylenol because the headache’s still there. You didn’t mean to overdose. You just didn’t know you were doubling up.
Each extra-strength Tylenol tablet has 500 mg of acetaminophen. The maximum daily dose for adults is 4,000 mg - that’s eight tablets. But if you’re also taking a cold medicine like NyQuil or DayQuil, that’s another 325 mg per dose. Two doses of that, plus four Tylenol tablets? You’re already at 3,000 mg. Add one more Tylenol and you’re over the edge. And you didn’t even feel anything yet.
The real danger? You won’t feel sick right away. In fact, most people feel fine for 12 to 24 hours after taking too much. Nausea, vomiting, sweating - those might show up early, but they’re easy to ignore. By the time your liver starts failing - which can happen in as little as 48 hours - it’s often too late to reverse the damage. This isn’t like a stomach bug. This is silent, slow, and deadly.
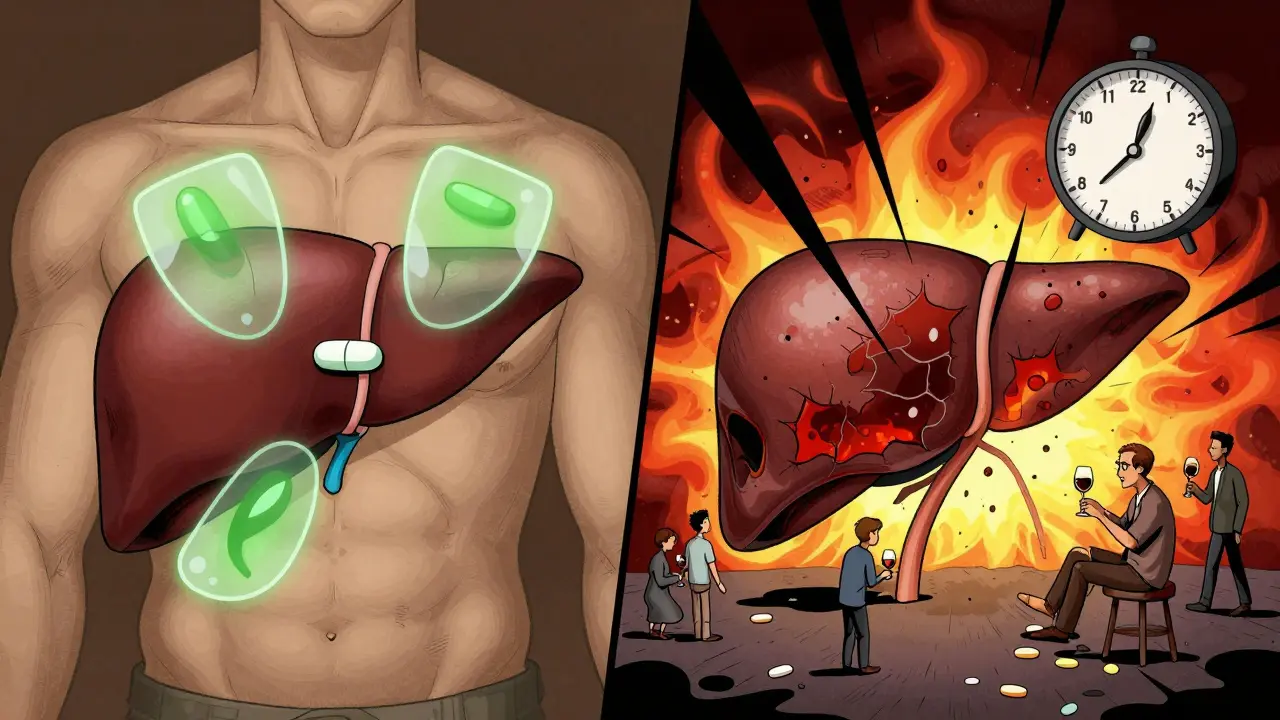
What Happens to Your Liver When You Take Too Much
Your liver is the main organ that breaks down acetaminophen. At normal doses, it handles it easily. But when you take more than your liver can process - usually over 7.5 grams in one go, or more than 4 grams spread over a couple of days - something dangerous happens. A toxic byproduct called NAPQI builds up. Normally, your liver has a buffer called glutathione to neutralize it. But when you overload the system, that buffer runs out. Then NAPQI starts eating away at liver cells.
That’s when things get serious. Liver enzymes (AST and ALT) spike. Jaundice appears - your skin and eyes turn yellow. Your abdomen swells. You get confused. Your blood doesn’t clot right. In severe cases, your kidneys fail too. At this stage, you need a liver transplant to survive. In the U.S., acetaminophen overdose is the number one cause of acute liver failure. It accounts for nearly half of all cases. And about 500 people die from it every year.
What makes this even scarier? It’s not just about taking 10 pills at once. Chronic use - like taking 3,000 mg a day for a week - can do the same damage. People with existing liver problems, heavy drinkers, or those on certain medications are at even higher risk. Even three alcoholic drinks a day can make your liver more vulnerable. You don’t have to be an alcoholic. Just one glass of wine with your nightly painkiller? That’s enough to tip the scale.
The Four Stages of Acetaminophen Toxicity
There’s a clear timeline to how this unfolds - and knowing it could save your life.
Stage 1 (0-24 hours): You might feel a little off. Nausea, vomiting, loss of appetite, sweating. Your liver enzymes? Still normal. You think it’s just a stomach bug. You go to bed. Big mistake.
Stage 2 (24-72 hours): The pain starts. Dull, constant ache under your right ribs. Your skin feels clammy. You’re tired. Blood tests now show rising liver enzymes - but you still feel okay. Most people don’t go to the doctor until now. By then, the damage is already done.
Stage 3 (72-96 hours): This is the crisis. Jaundice. Confusion. Swelling in your belly. Your blood can’t clot. Your kidneys start shutting down. Liver enzymes can be 10,000 IU/L or higher (normal is under 40). You’re in intensive care. This is where many people need a transplant.
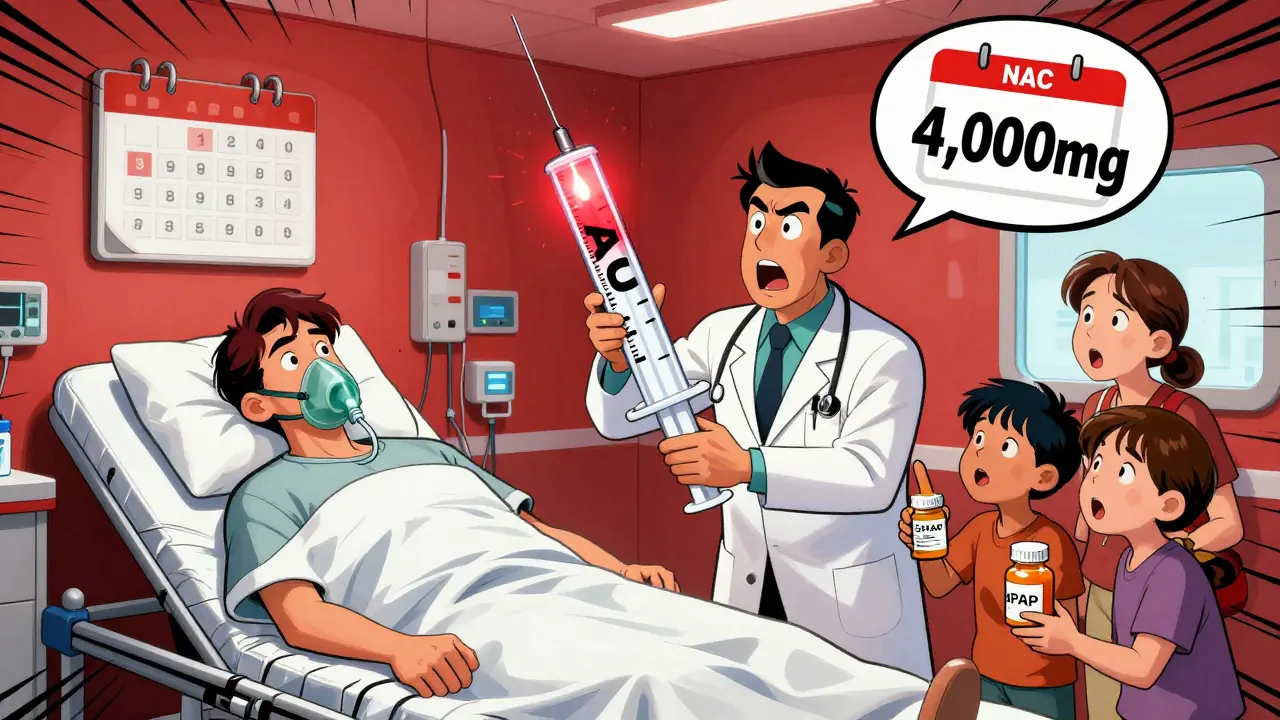
Stage 4 (after 5 days): Either you recover - or you don’t. If you got treatment with N-acetylcysteine (NAC) within 8 hours, your chances of full recovery are 90%. After 16 hours? That drops to 60%. If you waited until you felt sick? Your odds drop below 30%.
How to Prevent an Overdose - For Real
Here’s what actually works. Not vague advice. Specific, actionable steps.
- Know your limit: Never take more than 3,000 mg per day if you’re over 65, have liver disease, or drink alcohol. Stick to 4,000 mg max if you’re healthy - and even then, avoid it daily. Use the lowest effective dose.
- Read every label: Look for "acetaminophen" or "APAP" - that’s the abbreviation. It’s often printed in small font. If a medicine has it, write it down. Add up all your sources. If you’re taking three different products, you’re likely over the limit.
- Never mix with alcohol: Even one drink a day increases your risk. If you’re on acetaminophen, skip the wine, beer, or whiskey. Period.
- Use a measuring cup: Never use a kitchen spoon for liquid acetaminophen. A teaspoon is 5 mL. A tablespoon is 15 mL. That’s three times too much. CDC data shows 12% of pediatric overdoses happen because of this. Adults do it too.
- Check prescriptions: If you’re on Vicodin, Percocet, or similar, ask your doctor how much acetaminophen is in each pill. Most have 325 mg. If you’re also taking Tylenol, you’re doubling up. Ask for a version without acetaminophen.
- Use one pharmacy: If you fill all your prescriptions at one pharmacy, they can flag dangerous combinations. Most pharmacies have systems to catch this. Use them.
What to Do If You Think You Took Too Much
Don’t wait for symptoms. Don’t hope it’ll pass. Don’t Google it.
If you took more than 6 grams (12 extra-strength tablets) in 24 hours - or if you took more than 4 grams over a few days - call Poison Control immediately at 1-800-222-1222. They’ll ask you how much, when, and what else you took. Then they’ll tell you whether to go to the ER.
If you’re in the ER and you’ve taken too much, ask for N-acetylcysteine (NAC). It’s the antidote. It works best within 8 hours. After 16, it’s still helpful - but not as much. The sooner, the better. And yes, it’s safe. It’s given in IV form or as a pill. Side effects? Maybe nausea. But it saves lives.
And if you’re helping someone else - don’t wait for them to wake up. If they’re unconscious, vomiting, or acting confused after taking painkillers - call 911. Don’t wait. Don’t assume they’re just drunk. They might be dying.
Why Labels Are Failing You
The FDA requires a "Liver Warning" on all acetaminophen products. But here’s the catch: only 38% of people who see it understand it’s talking about acetaminophen. Many think it’s about ibuprofen or aspirin. The font is too small. The wording is too vague. And in combination products, it’s buried under 10 other ingredients.
Studies show that 25% of accidental overdoses happen because people didn’t realize two different medicines had the same ingredient. One woman took Tylenol for back pain and NyQuil for a cold. She took four doses of each over two days. Her liver enzymes went through the roof. She didn’t know NyQuil had acetaminophen. The label said "APAP" - but she didn’t know what that meant.
That’s why experts are pushing for bigger, bolder labels. The FDA is considering requiring "ACETAMINOPHEN" in bold, capitalized letters on the front of every package. That’s a start. But until then, you have to be your own safety net.
Who’s Most at Risk?
- Adults 30-50: This group is most likely to take multiple medications for chronic pain, colds, and sleep. They’re not trying to overdose - they’re trying to feel better.
- People with liver disease: Even mild fatty liver or hepatitis increases risk. The liver can’t handle the extra load.
- Heavy drinkers: Alcohol depletes glutathione. Even moderate drinking - three drinks a day - makes your liver more vulnerable.
- Older adults: Metabolism slows with age. The liver processes acetaminophen slower. Doses that were fine at 40 can be dangerous at 65.
- Parents giving kids adult medicine: Children’s dosing is based on weight. Using adult tablets? A common mistake. Always use pediatric formulations and a measuring device.
If any of this sounds like you - stop. Re-read your medicine cabinet. Write down every product with acetaminophen. Add up the total. If it’s over 3,000 mg a day - cut back. Talk to your doctor. Switch to something else if you need to.
Alternatives to Acetaminophen
Not everyone needs acetaminophen. If you’re worried about liver damage, consider:
- Ibuprofen or naproxen: These are NSAIDs. They’re harder on the stomach and kidneys, but safe for the liver. Good for inflammation, fever, and pain. Avoid if you have ulcers, kidney disease, or take blood thinners.
- Topical pain relievers: Creams with menthol, capsaicin, or lidocaine. No systemic absorption. Great for joint or muscle pain.
- Physical therapy or heat/cold packs: For chronic pain, these are often more effective long-term than pills.
- Acetaminophen-free cold medicines: Look for products labeled "acetaminophen-free" or "non-drowsy." Many exist.
There’s no perfect substitute. But there are safer choices if you’re at risk.
Can you overdose on acetaminophen by taking it for a few days?
Yes. While most overdoses happen from taking too much in one go, taking more than 4,000 mg per day for several days - even 3,000 mg daily - can cause liver damage. This is called chronic toxicity. It’s slower, harder to notice, and often missed until it’s too late. People who take it daily for back pain or arthritis are especially at risk.
Is Tylenol safer than other painkillers?
It’s safer for your stomach and kidneys than ibuprofen or aspirin, which can cause ulcers or kidney damage. But it’s far more dangerous for your liver. If you have a healthy liver and no alcohol use, acetaminophen is fine at low doses. But if you have any liver issues, drink alcohol, or take other medications - it’s not the safest choice. Always weigh the risks.
How do I know if a medicine has acetaminophen?
Look for "acetaminophen" or "APAP" on the Drug Facts label. It’s usually listed under "Active Ingredients." If you’re unsure, check the brand name. Common products with it include Tylenol, NyQuil, DayQuil, Excedrin, TheraFlu, and many prescription painkillers like Vicodin. If you’re not sure, ask your pharmacist.
Can you take acetaminophen if you drink alcohol?
It’s risky. Even one drink a day can increase your chance of liver damage. Three or more drinks daily? Don’t take acetaminophen at all. The combination lowers your liver’s ability to detoxify the drug. You don’t have to be an alcoholic. Moderate drinking is enough to raise your risk. If you drink, switch to an alternative pain reliever.
What if I took too much but feel fine?
That doesn’t mean you’re safe. Symptoms can take 12 to 24 hours to appear. If you took more than 4,000 mg in 24 hours - or if you’re unsure - call Poison Control immediately. Waiting until you feel sick could cost you your liver. N-acetylcysteine (NAC) works best within 8 hours. Don’t gamble with your health.
Acetaminophen isn’t evil. It’s a powerful tool when used correctly. But it’s not a candy. It’s a drug with a razor-thin line between help and harm. If you’re taking it, you owe it to yourself to know exactly how much you’re using - and what else you’re mixing it with. Your liver can’t warn you. You have to be the one who listens.