Bioequivalence Limits: What They Mean for Generic Drugs and Your Health
When you pick up a generic pill, you’re trusting that it will do the same job as the brand-name version. That trust comes from bioequivalence limits, the strict range of allowed differences in how quickly and completely a drug enters your bloodstream. Also known as therapeutic equivalence standards, these limits are the invisible rulebook that keeps generics safe and effective. If a generic drug doesn’t meet these limits, it might not work as well—or could even cause side effects. That’s not theoretical. Studies show that even small shifts in how a drug is absorbed can change how it controls blood pressure, seizures, or depression in real patients.
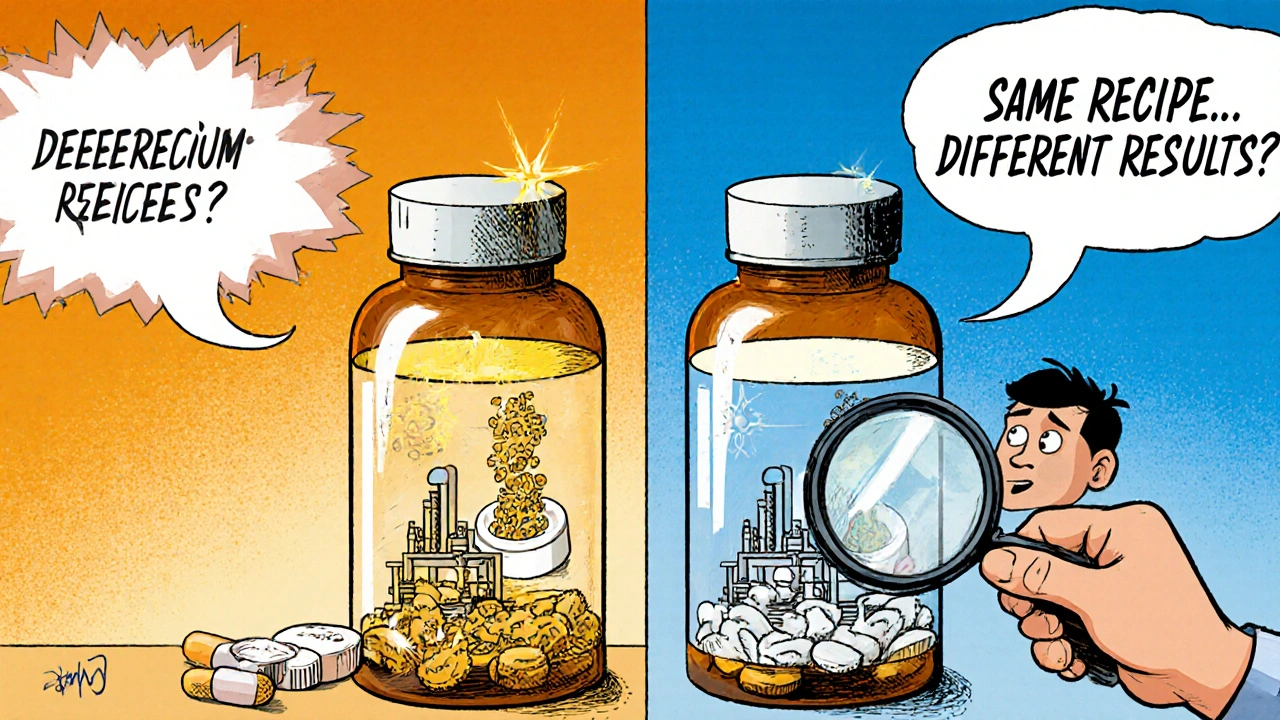
These limits aren’t just about the active ingredient. They also account for how the drug is made—its coating, filler, or how fast it dissolves. Two pills can have the same chemical, but if one dissolves too slowly, your body won’t get enough of it. Too fast, and you risk a spike that causes dizziness or nausea. That’s why regulators like the FDA and EMA require generics to deliver between 80% and 125% of the brand-name drug’s absorption rate. Anything outside that range fails the test. This isn’t about cutting corners. It’s about making sure your blood levels stay steady, day after day.
And it’s not just about the drug itself. generic drugs, medications that copy brand-name drugs after patents expire. Also known as copycat medicines, they rely entirely on these limits to prove they’re interchangeable. If a generic passes bioequivalence testing, your pharmacist can swap it without asking. But if the limits are stretched too thin—say, because of a new manufacturer or a cheaper filler—it can throw off your whole treatment. That’s why some patients report feeling different on a new batch of generics, even when the label says it’s the same. It’s not in their head. It’s in the numbers.
Related to this are drug absorption, how your body takes in and uses a medication after swallowing it. Also known as pharmacokinetics, it’s the core reason bioequivalence limits exist. If your body doesn’t absorb the drug properly, it won’t reach the right spot in your system. For drugs like warfarin, levothyroxine, or epilepsy meds, even a 10% drop in absorption can mean the difference between control and crisis. That’s why doctors watch for changes when switching brands—and why patients should speak up if they feel off after a refill.
What you’ll find in the posts below isn’t just theory. It’s real stories from people who’ve seen the impact of these limits firsthand—from unexpected side effects when switching generics, to how patient trust gets shaken when a pill that used to work suddenly doesn’t. You’ll see how inactive ingredients, dosing timing, and even how a pill is split can tie back to bioequivalence. These aren’t abstract rules. They’re the quiet foundation of your daily health. And if you’ve ever wondered why your doctor asks if you switched pharmacies or brands, now you know why.