When someone loses a limb, their body doesn’t just lose muscle and bone-it loses a part of how the brain understands the body. Phantom limb pain (PLP) isn’t in your head. It’s in your nervous system. You feel pain in a foot that’s no longer there, a hand that’s gone, because your brain still expects signals from that area. And when those signals don’t come, the system glitches. The pain isn’t fake. It’s real. And it’s common. Between 60% and 85% of amputees experience it. For many, it starts within days. For others, it creeps in months later. And once it sticks around past six months, it rarely goes away on its own.
What Phantom Limb Pain Really Feels Like
People describe it in different ways: burning, electric shocks, cramping, or like a claw digging into the missing limb. The pain usually centers in the farthest part-the toes, the fingers-where the limb used to end. It’s not the same as stump pain, which happens at the cut site. Stump pain might be from scar tissue or a neuroma. Phantom pain? That’s the brain misfiring.
Studies using MRI and PET scans show this clearly. When someone with PLP feels pain, the same brain areas that once handled sensation from the lost limb light up. It’s like the brain’s map of the body got scrambled. Nearby areas-like the face or the other leg-start to take over the unused space. So when you touch your cheek, your brain might interpret that as pain in your missing foot. That’s cortical remapping. It’s not psychology. It’s neurology.
Why Medications Are the First Line of Defense
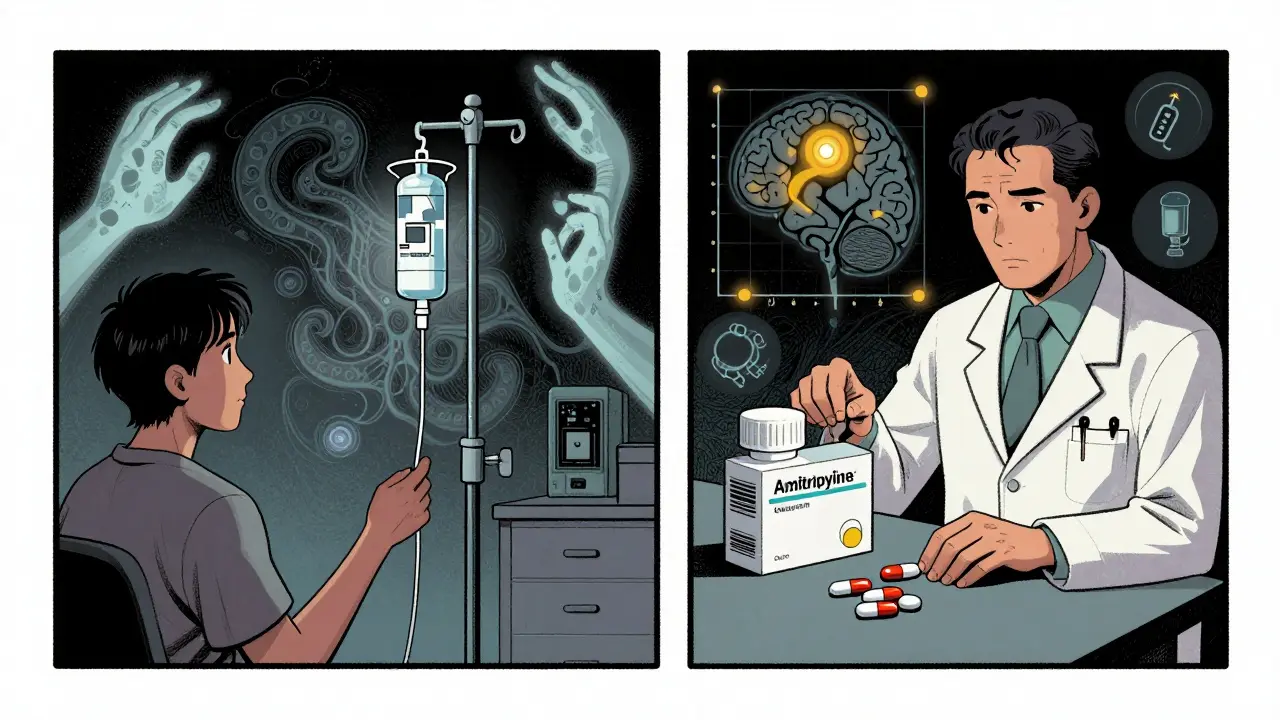
Doctors start with meds because they’re fast, measurable, and backed by decades of use. The most common? Tricyclic antidepressants. Not because you’re depressed, but because they calm overactive nerves. Amitriptyline, usually started at 10 mg at bedtime, is the go-to. It doesn’t knock you out like it used to, but it does help. About 45% of users report moderate pain relief. Side effects? Drowsiness, dry mouth, weight gain. But for many, it’s worth it.
Gabapentin and pregabalin come next. These are anticonvulsants, originally for seizures, but they work wonders on nerve pain. Gabapentin starts at 300 mg a day, slowly climbed to 900-3600 mg. Pregabalin is stronger, dosed at 75-600 mg daily. Reddit users in the r/amputee community report 72% found gabapentin helpful-but 58% quit because of dizziness or brain fog. That’s the trade-off: relief vs. side effects.
NSAIDs like ibuprofen or naproxen? They help a little at first. About 65% of patients feel some relief early on. But for 80% of them, it fades after three to six months. They’re not the answer for chronic pain. Opioids? Oxycodone, morphine. They work, but they’re risky. The American Pain Society warns against using more than 30-50 morphine milligram equivalents daily. Long-term use leads to dependence. One in three long-term users on pain forums report addiction struggles. So opioids are a last resort.
Then there’s ketamine. An IV drip at 0.1-0.5 mg/kg. Used only when everything else fails. It blocks NMDA receptors-the brain’s pain amplifier. It’s not for everyone. It can cause hallucinations, dizziness, or high blood pressure. But for those with severe, treatment-resistant pain? It can be life-changing.
Mirror Therapy: Seeing Is Believing
Mirror therapy is simple. You sit with a mirror standing upright between your arms or legs. Your intact limb is on one side. The stump is hidden behind the mirror. You move the good limb, watching its reflection as if it’s the missing one. Your brain sees movement. It sees symmetry. And slowly, it starts to unlearn the pain.
This isn’t magic. It’s based on work by Dr. V.S. Ramachandran in the 1990s. He noticed that when amputees moved their phantom limb, they felt pain. But when they saw a reflection of their real limb moving-like the phantom was moving too-the pain lessened. The brain was being tricked into correcting its own map.
How often? Daily. Fifteen to thirty minutes. You wiggle your fingers. Make a fist. Touch your nose. Move your foot. The mirror doesn’t lie. And your brain starts to believe it again. Studies show about 50-70% of people who stick with it see improvement. But here’s the catch: 40% quit within eight weeks. It’s boring. It’s repetitive. It takes discipline.
Some now use virtual reality instead of mirrors. VR headsets show a digital limb moving in sync with the real one. Early trials suggest it boosts adherence. By 2027, experts predict over 85% of users will stick with VR-based versions-compared to just 60% with mirrors.
Other Non-Medication Options
Transcutaneous electrical nerve stimulation (TENS) is another tool. Electrodes on the stump deliver low-voltage pulses. It doesn’t fix the brain’s map, but it distracts the nerves. Studies show 30-50% effectiveness in moderate cases. You need proper placement-frequency between 2-150 Hz, pulse duration 50-250 microseconds. Most people need two or three sessions to learn how to use it right.
Botox injections? Yes, really. Injected into neuromas (tangled nerves at the stump), 20-50 units can reduce both pain and sweating. One 2023 case study saw pain drop from 8/10 to 3/10 for 12 weeks. It’s not permanent, but it’s a bridge.
Spinal cord stimulators? Tiny electrodes implanted near the spine. They send pulses that block pain signals. Response rates? 40-60%. The FDA approved a new closed-loop system in January 2024 called Evoke. It adjusts automatically based on your movement. In trials, it cut pain by 65% on average.

What Doesn’t Work-and What Might
Some myths still linger. Epidural anesthesia during surgery? It was thought to prevent PLP. But research now says no. It doesn’t. Pain still comes. Early intervention is key. Waiting six months? That’s too late. The brain’s rewiring hardens. The longer you wait, the harder it is to reverse.
What’s promising? Combination therapy. Medication + mirror therapy + TENS. Not one, not the other. All three. A 2024 study in the Journal of Neurosurgery showed 70% pain reduction in patients who got targeted muscle reinnervation (TMR) plus osseointegration. TMR reroutes nerves to muscle groups, so when you think about moving your hand, your chest muscle twitches instead. Sensors pick that up and move a prosthetic. The brain gets feedback. It stops screaming.
Future treatments? Selective NMDA modulators. New drugs that block pain signals without the hallucinations of ketamine. Phase II trials show 50% pain reduction at lower doses. That’s huge.
Real Talk: What Patients Say
One man in Perth tried amitriptyline. It helped, but he couldn’t drive because of drowsiness. He switched to gabapentin. Better, but he gained 15 pounds. He started mirror therapy. At first, he thought it was silly. After three weeks, he noticed his phantom foot didn’t cramp as much when he moved his real one. He still takes gabapentin. Still does mirror therapy. Still has pain-but it’s manageable.
A woman on a support forum said she tried opioids for three months. She got hooked. She went cold turkey. It took six weeks. She’s now on pregabalin and uses a VR mirror every morning. She says, “I don’t feel like I’m losing my body anymore.”
There’s no cure. But there’s control. And that’s the goal.
Is phantom limb pain psychological?
No. Phantom limb pain is a neurological condition, not a mental one. Brain scans show clear activity in areas that once controlled the missing limb. It’s caused by nerve damage, spinal cord changes, and brain rewiring-not stress or anxiety. While emotions can make it worse, the pain itself is real and physical.
How long does phantom limb pain last?
For many, it fades within six months. But if it lasts longer than that, it’s unlikely to disappear without treatment. Studies show persistent pain after six months has a "slim-to-none" chance of resolving on its own. Early intervention is critical-waiting too long makes treatment harder.
Does mirror therapy really work?
Yes, for about half to two-thirds of people who stick with it. It doesn’t work overnight. You need to do it daily for 15-30 minutes over weeks or months. The key is consistency. Newer versions using virtual reality improve adherence and may boost results. It’s not a cure, but it can significantly reduce pain and improve quality of life.
What’s the best medication for phantom limb pain?
There’s no single "best"-it depends on the person. Tricyclic antidepressants like amitriptyline are most commonly prescribed and work well for many. Gabapentin and pregabalin are next, especially for burning or shooting pain. Ketamine is reserved for severe cases. NSAIDs help a little at first but lose effectiveness over time. Opioids are risky and should only be used short-term if nothing else works.
Can phantom limb pain be prevented?
Not reliably. Even with perfect surgery and pain control during the procedure, PLP still develops in most cases. The best approach is early treatment once pain starts. Some newer techniques like targeted muscle reinnervation (TMR) during amputation show promise in reducing future pain, but they’re not yet standard everywhere.












1 Comments
Hey, I just wanted to say this post made me feel seen. I’ve had PLP for 8 years now, and mirror therapy was the first thing that actually helped me sleep through the night. It felt silly at first-like, really silly-but after 3 weeks of doing it while watching Netflix, the burning in my phantom toes started fading. I still take gabapentin, but now I don’t feel like I’m fighting my own body every day. You’re not crazy for trying. Keep going. 💪❤️