Alcohol-Medication Interaction Checker
Check if it's safe to consume alcohol with your medications. This tool is based on FDA warnings and medical research about dangerous interactions.
Enter a medication name to check if it's safe to consume with alcohol.
Every year, thousands of people end up in emergency rooms not because of a fall, a car crash, or a bad infection - but because they drank alcohol while taking their medicine. It’s not always obvious. You might think a glass of wine with your painkiller is harmless. Or that a beer after your antibiotic won’t hurt. But the truth is, alcohol and medications don’t mix safely in most cases - and the risks are far worse than most people realize.
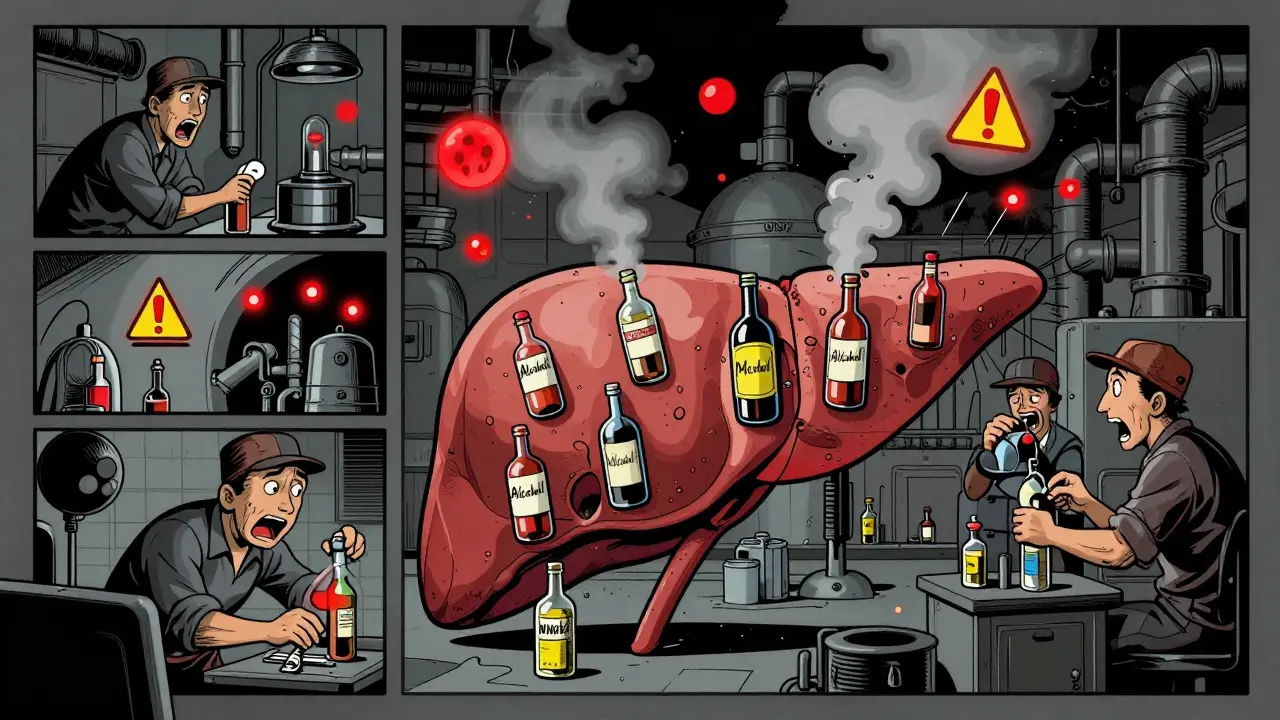
Why Alcohol and Medications Don’t Mix
Your liver is the main factory that breaks down both alcohol and most medications. When you drink while on meds, your liver gets overloaded. It can’t handle both at once. So one or both substances build up in your system. That can make side effects stronger, turn a safe drug into a toxic one, or even stop your medicine from working at all. Alcohol doesn’t just sit there. It changes how your body absorbs, moves, and gets rid of drugs. It also teams up with some medications to make their effects way stronger - especially on your brain and breathing. This is called a synergistic effect. Think of it like turning up the volume on a song you’re already listening to. Suddenly, it’s deafening.Deadly Combinations: Opioids, Benzodiazepines, and Alcohol
Some combinations can kill you in minutes. The worst offenders are opioids like oxycodone, hydrocodone, and methadone, and benzodiazepines like Xanax, Valium, and Klonopin. Both types slow your breathing. Alcohol does the same. Together, they can shut down your respiratory system completely. The FDA removed the extended-release opioid Palladone from the market in 2005 after studies showed that drinking alcohol with it caused a dangerous “dose-dumping” effect - the drug released all at once, flooding the body with a lethal dose. In 2020, 20% of opioid overdose deaths in the U.S. also involved alcohol. For people taking benzodiazepines, mixing with alcohol increases overdose risk by 24 times, according to a 2019 study. If you’re on one of these drugs, even one drink can be too much. And if you’re unsure, assume it’s dangerous. Don’t guess. Ask your pharmacist.Acetaminophen and Alcohol: A Silent Liver Killer
Many people think Tylenol is safe. It’s in almost every medicine cabinet. But take it with alcohol - even a few drinks over a few days - and you’re putting your liver at serious risk. When alcohol and acetaminophen are processed together, your liver creates a toxic chemical called NAPQI. Normally, your body neutralizes it with glutathione. But alcohol depletes glutathione fast. Without it, NAPQI starts destroying liver cells. This isn’t a slow process. It can cause acute liver failure in under 48 hours. The FDA says acetaminophen overdoses - often triggered by alcohol - cause 56,000 ER visits, 26,000 hospitalizations, and nearly 500 deaths every year in the U.S. If you take Tylenol regularly for pain or fever, avoid alcohol entirely. Even one drink on the same day can tip the balance.NSAIDs, Alcohol, and Your Stomach
Ibuprofen, naproxen, aspirin - these common pain relievers are fine for occasional use. But add alcohol, and you’re playing Russian roulette with your digestive tract. Both alcohol and NSAIDs irritate the stomach lining. Together, they dramatically increase the chance of bleeding ulcers. A 2017 meta-analysis found that combining them raises the risk of gastrointestinal bleeding by 3 to 5 times. For older adults or those with a history of ulcers, this isn’t just uncomfortable - it’s life-threatening. If you take these meds daily for arthritis or chronic pain, skip the beer. If you’re having a drink on the weekend, wait at least 6 hours after your last pill. And never take NSAIDs on an empty stomach if you’ve been drinking.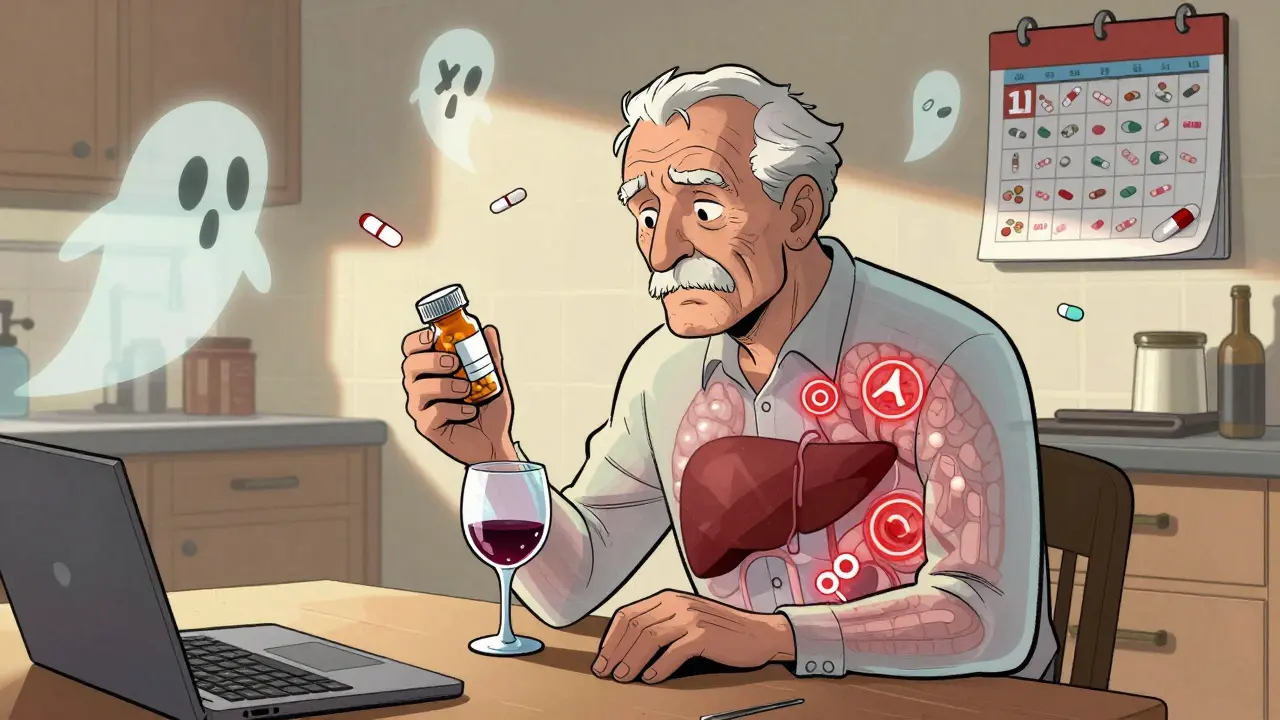
Antibiotics: Not All Are Equal
You’ve probably heard not to drink alcohol while on antibiotics. But not all antibiotics react the same way. Metronidazole (Flagyl) and tinidazole cause a severe reaction called disulfiram-like reaction. Within minutes of drinking, you’ll get intense nausea, vomiting, flushing, rapid heartbeat, and dizziness. It’s terrifying - and it can land you in the ER. The Illinois Poison Center says to wait at least 72 hours after your last dose before having any alcohol. Other antibiotics like azithromycin or doxycycline don’t cause this reaction. But alcohol can still make nausea, dizziness, and stomach upset worse. It also weakens your immune system, making it harder for your body to fight off the infection you’re trying to treat. Bottom line: If your prescription label says “avoid alcohol,” don’t test it. If it doesn’t say anything, ask your pharmacist. Don’t assume it’s safe.Diabetes Medications and Alcohol: The Hidden Danger
People with diabetes are often told to limit alcohol. But the reason isn’t just about sugar. It’s about blood sugar crashes. Drugs like sulfonylureas (glyburide, glipizide) and meglitinides (repaglinide) push your pancreas to release insulin. Alcohol blocks your liver from releasing glucose to balance it out. The result? Severe hypoglycemia - low blood sugar - that can cause confusion, seizures, or coma. GoodRx reports that combining alcohol with sulfonylureas increases hypoglycemia risk by 300%. Even if you’re on metformin, alcohol raises your risk of lactic acidosis - a rare but deadly buildup of acid in the blood. The advice? If you have diabetes and take these meds, limit alcohol to one drink a day at most. Never drink on an empty stomach. Always check your blood sugar before and after.Antidepressants, Antihistamines, and Your Brain
SSRIs like Prozac and Zoloft don’t cause dangerous chemical reactions with alcohol - but they don’t help you either. Alcohol makes depression and anxiety worse. It also increases drowsiness and dizziness, which can lead to falls, especially in older adults. Over-the-counter antihistamines like diphenhydramine (Benadryl) and doxylamine (Unisom) are already sedating. Add alcohol, and you’re not just sleepy - you’re impaired. Reaction times slow. Judgment fades. Driving? Not even close to safe. Even non-drowsy antihistamines like loratadine (Claritin) can cause unexpected side effects when mixed with alcohol. Your body just doesn’t handle the load well.
Who’s Most at Risk?
You might think this only affects heavy drinkers. It doesn’t. Older adults are the most vulnerable. By age 65, the body processes alcohol slower. Liver function declines. Kidneys don’t clear drugs as well. And most people over 65 take an average of 14 prescriptions a year. That’s a lot of chances for dangerous overlaps. The Beers Criteria - a guide for safe prescribing in seniors - lists 30 medications that should be avoided if you drink, including benzodiazepines, muscle relaxants, and first-gen antihistamines. Women are also at higher risk. They have less body water and more body fat than men. That means alcohol concentrates more in their bloodstream after the same amount of drinking. A woman who drinks the same as a man will have a higher blood alcohol level - and a higher chance of drug interactions. Veterans and people with mental health conditions are another high-risk group. The VA found that 30% of veteran suicides involved alcohol and prescription drugs. People with co-occurring substance use and mental health disorders are 3.5 times more likely to have dangerous interactions.What You Can Do
You don’t have to give up alcohol entirely. But you do need to be smart.- Read every label. The FDA requires alcohol interaction warnings on 100 prescription drugs and 700 over-the-counter products. Look for phrases like “avoid alcohol” or “may cause drowsiness.”
- Ask your pharmacist. They’re trained to spot interactions. When you pick up a new prescription, ask: “Can I drink alcohol with this?” Don’t wait until you’re at home.
- Keep a list. Write down all your meds - including supplements and herbal remedies. Bring it to every doctor’s visit.
- Wait it out. If you’ve taken metronidazole, wait 72 hours. If you’ve had an opioid, avoid alcohol for the entire course of treatment - and then some.
- Use the AUDIT-C tool. It’s a simple 3-question screen doctors use to check for risky drinking. If you’re on high-risk meds, ask your provider to use it.
Final Warning
There’s no safe amount of alcohol when you’re on certain medications. For some, even one drink is too much. The risk isn’t theoretical. It’s documented. It’s in hospital records. It’s in FDA warnings. It’s in the stories of people who thought they were being careful - until they weren’t. If you’re unsure, skip it. Your body doesn’t need the risk. Your medicine doesn’t need the competition. And your life? It’s worth more than a drink.Can I have one drink while taking antibiotics?
It depends on the antibiotic. For metronidazole or tinidazole, no - even one drink can cause severe nausea, vomiting, and rapid heartbeat. For others like amoxicillin or azithromycin, alcohol doesn’t cause a direct reaction, but it can worsen side effects like dizziness or stomach upset and slow your recovery. Always check with your pharmacist before drinking.
Is it safe to drink alcohol with painkillers like ibuprofen or Tylenol?
With ibuprofen or other NSAIDs, alcohol increases your risk of stomach bleeding by 3 to 5 times. With Tylenol (acetaminophen), even moderate drinking can cause liver damage - especially if you take it regularly. Neither combination is safe. Avoid alcohol completely while using these meds.
Why are older adults more at risk for alcohol-medication interactions?
As we age, our liver and kidneys process alcohol and drugs more slowly. We also tend to take more medications - on average, 14 prescriptions a year for adults over 65. This increases the chance of dangerous overlaps. Plus, body water decreases with age, so alcohol stays in the bloodstream longer, making side effects stronger.
Can alcohol make my antidepressant less effective?
Yes. While alcohol doesn’t usually cause a dangerous chemical reaction with SSRIs like Prozac or Zoloft, it can worsen depression and anxiety symptoms. It also increases drowsiness and dizziness, making it harder to function. Over time, drinking can reduce the medication’s effectiveness and make recovery slower.
How long should I wait after taking a medication before drinking alcohol?
There’s no universal rule. For metronidazole, wait 72 hours. For opioids or benzodiazepines, avoid alcohol for the entire course of treatment - and longer if you’re still feeling effects. For most medications, waiting 4-6 hours after your last dose reduces risk, but it’s not foolproof. Always check with your pharmacist or doctor. When in doubt, skip it.











11 Comments
Man, I never realized how many meds I’m on that could go sideways with just one beer. I take ibuprofen for my back and a little wine at dinner seems harmless, but now I’m rethinking everything. Thanks for laying it out like this - I’m gonna ask my pharmacist tomorrow.
They don’t want you to know this but the FDA and Big Pharma are secretly pushing alcohol interactions to make you buy more drugs. The liver doesn’t even process alcohol like they say - it’s all about glyphosate in your wine and the 5G signals messing with your CYP450 enzymes. They removed Palladone because it exposed the truth. You think it’s about safety? Nah. It’s about control.
This hit me hard. My dad passed last year from liver failure after years of taking Tylenol for arthritis and having a glass of whiskey every night. He thought he was being careful. He wasn’t. I wish someone had told him this. Please, if you’re reading this and you’re on meds - just say no to the drink. It’s not worth it.
so like... if i take benadryl for allergies and then have a glass of wine cause i'm tired... am i gonna die?? like literally?? also why do they even make these meds if they're so dangerous?? someone's making money off this
In India, we mix alcohol with painkillers all the time - no one dies. Maybe it’s genetics? Or maybe Western medicine overstates risks to sell more tests and pills. I respect the info, but cultural context matters too.
Ugh I just read this and now I feel guilty about my Friday margarita with my celebrex. Can we just... not? Like, why does everything have to be so dramatic? I’m fine.
The real tragedy is not the alcohol or the medication - it’s the loss of personal sovereignty. We have been conditioned to fear the natural, the organic, the human - while corporate entities sell us synthetic solutions wrapped in clinical jargon. The liver is not a factory - it is a temple. When we force it to process poison disguised as medicine and intoxication disguised as leisure, we commit spiritual suicide. The FDA does not protect you - it pacifies you with compliance.
It’s irresponsible to imply that all alcohol-medication interactions are equally dangerous. For example, occasional alcohol use with azithromycin carries negligible risk - the real danger lies in chronic misuse or ignorance. This post is broadly accurate but dangerously oversimplified. Always consult your prescriber, not Reddit.
While the data presented is statistically valid and clinically sound, one must consider the global pharmacovigilance disparity. In low-resource settings, adherence to alcohol-medication guidelines is often secondary to access to medication itself. The ethical imperative lies not in prohibition, but in equitable education and pharmaceutical accessibility. One cannot admonish a man without medicine for abstaining from alcohol when he has no access to safer alternatives.
so like... if i drink and take my anxiety meds... am i just a dumbass? 🤦♀️
People think they’re being rebellious by having a drink with their meds... but really they’re just handing their liver a one-way ticket to oblivion. And then they wonder why they feel worse. The body doesn’t care about your intentions. It just does the math. And the math always wins. You don’t need to be a saint - just be smart. One drink isn’t worth becoming a statistic.