Colchicine Antibiotic Safety Checker
Check Your Antibiotic Safety
Safety Assessment
Take colchicine for gout or heart inflammation. You’re told to stick to the low dose. Then you get a sinus infection. Your doctor prescribes clarithromycin. You take both. Two days later, you’re in the ER with muscle pain, vomiting, and low blood counts. This isn’t rare. It’s predictable. And it’s deadly.
Why This Interaction Isn’t Just a ‘Possible’ Risk
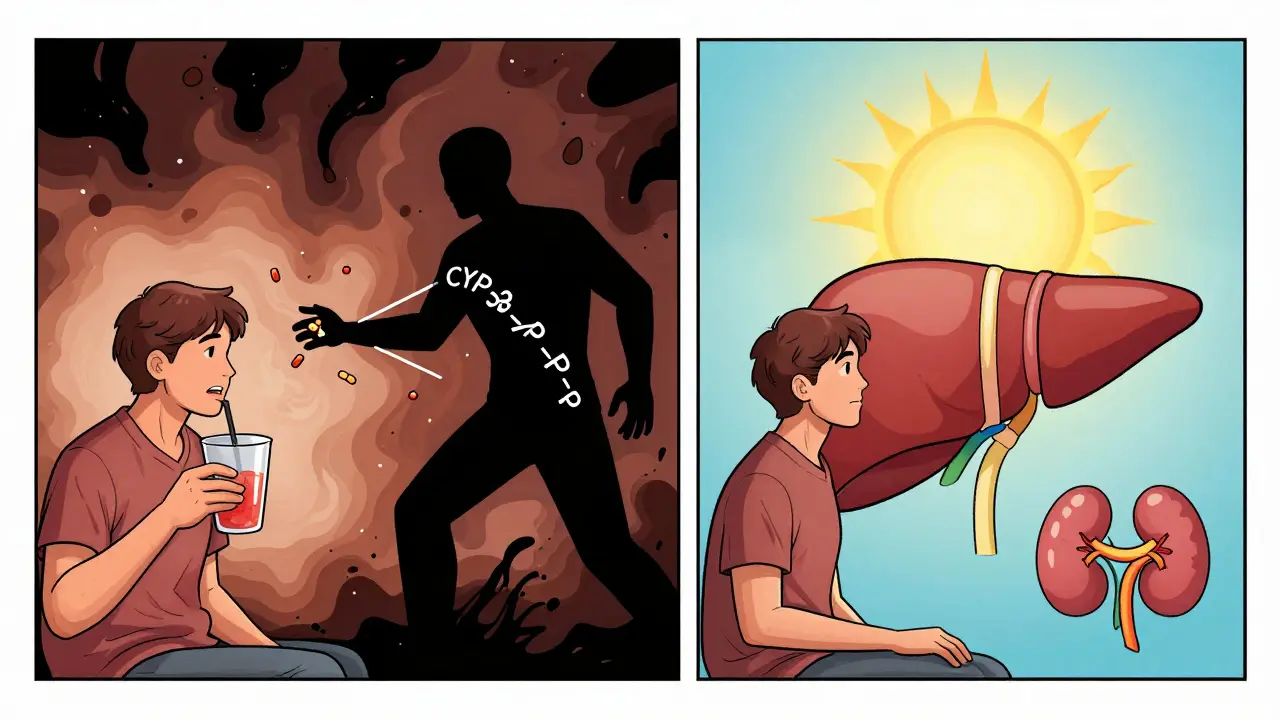
Colchicine isn’t your average pill. It’s a poison with a job. Used for gout and pericarditis, it works by stopping inflammation at the cellular level. But the line between healing and harm is razor-thin. A normal dose is 0.6 mg once or twice a day. Too much? You get bone marrow failure, kidney damage, or worse. And macrolide antibiotics-especially clarithromycin and erythromycin-can turn that safe dose into a lethal one.This isn’t about one enzyme. It’s about two. Colchicine is cleared from your body through two main routes: CYP3A4 in your liver and gut, and P-glycoprotein (P-gp), a transporter that kicks drugs out of cells. Macrolides like clarithromycin block both. They don’t just slow down metabolism-they trap colchicine inside your cells. The result? Colchicine levels can jump four times higher than normal. That’s not a theoretical risk. It’s a documented pattern in hospitals.
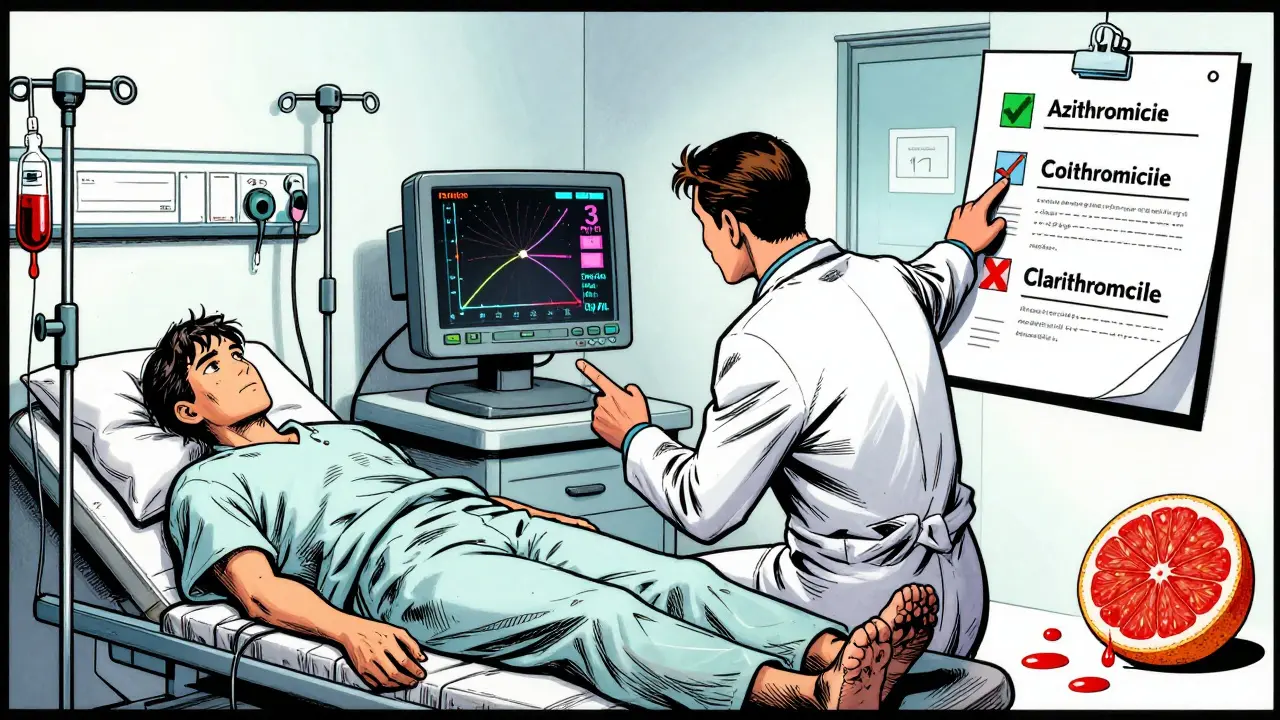
Not All Macrolides Are the Same
You might think all antibiotics in the macrolide family are equal. They’re not. Clarithromycin is the worst offender. It’s a strong double inhibitor-powerful against both CYP3A4 and P-gp. Erythromycin is a step down, but still risky. Azithromycin? It barely touches either system. Studies show it doesn’t raise colchicine levels at all.That’s critical. If you need an antibiotic while on colchicine, azithromycin is your safest bet. It’s not just a minor difference-it’s the difference between going home and ending up in the ICU. A 2022 study of over 12,000 patients found that those taking clarithromycin or erythromycin with colchicine had more than double the risk of toxicity. Azithromycin? No increased risk. The choice isn’t subtle. It’s life-or-death.
The Numbers Don’t Lie
The FDA got serious about this in 2010. They added a black box warning-the strongest possible-to colchicine labels. Since then, the Adverse Event Reporting System has logged 147 cases of toxicity linked to macrolides between 2015 and 2020. Sixty-three percent involved clarithromycin. Twenty-eight percent involved erythromycin. Three patients died in a single case series.Real-world data backs this up. A 2023 survey of 245 doctors found that 68% had seen at least one case of this interaction. Emergency room doctors saw it more than rheumatologists-82% versus 54%. Why? Because ER docs are the first to see the fallout. Patients don’t always tell their doctors they’re on colchicine. They might be taking it for heart inflammation and think it’s just a ‘regular anti-inflammatory.’
Why Some Doctors Still Get It Wrong
You’d think electronic health records would catch this. They don’t always. Many systems only flag the strongest interactions. A 2024 study in JAMA Internal Medicine showed that after Epic updated its alert system to include tiered warnings for colchicine and macrolides, inappropriate prescribing dropped by 63%. Before that? Doctors were missing it.Even more concerning: a 2021 study found that 43% of internal medicine residents couldn’t identify high-risk drug pairs involving colchicine. After a short training module, that number dropped to 13%. This isn’t about ignorance. It’s about complexity. Colchicine isn’t on most drug interaction checklists. And when it is, the warning is buried.
What Happens When You Mix Them
Toxicity doesn’t come with a warning sign. It creeps in. First, nausea, vomiting, diarrhea. Then, muscle weakness. Then, low white blood cell counts. Then, rhabdomyolysis-muscle tissue breaking down and poisoning the kidneys. In severe cases, multi-organ failure. Some patients need dialysis. Others don’t survive.And it’s not just about the dose. People with kidney or liver problems are at higher risk because they clear colchicine slower. Even a normal dose can be too much. The FDA says colchicine levels above 3.3 ng/mL are dangerous in people with kidney disease. But few hospitals can test for it. Only 37% of U.S. hospitals offer routine colchicine level monitoring. So doctors are flying blind.
What to Do Instead
If you’re on colchicine and need an antibiotic, here’s your action plan:- Stop clarithromycin and erythromycin. Avoid them completely.
- Use azithromycin. It’s safe. Proven. Widely available.
- If no alternative exists, reduce your colchicine dose by 50% and monitor closely. Don’t just guess-talk to your pharmacist or doctor.
- Check your other meds. Diltiazem, verapamil, ketoconazole, and even some grapefruit juice can do the same thing. They’re not antibiotics, but they’re just as dangerous.
There’s a reason the American College of Rheumatology and the American College of Cardiology both say: Do not combine colchicine with strong CYP3A4 or P-gp inhibitors. This isn’t a suggestion. It’s a standard of care.
The Bigger Picture: Why This Matters Now
Colchicine use has exploded since 2010. It’s no longer just for gout. The FDA approved it for heart attacks and pericarditis. More people are taking it. More people are getting infections. More people are getting antibiotics. The math is simple: 1.2 million Americans are likely taking this dangerous combo every year.And the cost of alternatives? Canakinumab, a biologic that works without these interactions, costs nearly $200,000 a year. Colchicine? Around $4,200. So we’re stuck with it. That means we have to get this right. We can’t afford to stop using colchicine. But we can’t afford to ignore the risks either.
What’s Coming Next
There’s hope. Takeda, the maker of colchicine, is testing a new version-COL-098-that doesn’t rely on P-gp. Early trials show a 92% reduction in interaction risk. That’s huge. And researchers are looking at genetics. Some people have gene variants (like CYP3A5*3/*3 or ABCB1 3435C>T) that make them extra sensitive to colchicine. In one study, these genes predicted 78% of toxicity cases.Future care won’t just be about avoiding drugs. It’ll be about knowing who’s most at risk before they even take the pill.
Bottom Line: Don’t Guess. Ask.
If you’re on colchicine, don’t assume your antibiotic is safe. Don’t rely on memory. Don’t assume your doctor knows. Bring your full list of meds to every appointment-prescription, over-the-counter, even supplements. Grapefruit juice, St. John’s wort, turmeric-they can all interfere.And if you’re prescribed clarithromycin or erythromycin while on colchicine, say something. Ask: ‘Is there a safer antibiotic?’ The answer might save your life.
Can I take azithromycin with colchicine?
Yes. Azithromycin does not significantly inhibit CYP3A4 or P-gp, and studies show it does not raise colchicine levels. It is the safest macrolide antibiotic to use with colchicine. Always confirm with your pharmacist, but azithromycin is the recommended alternative when an antibiotic is needed.
Is clarithromycin always dangerous with colchicine?
Yes. Clarithromycin is a strong inhibitor of both CYP3A4 and P-gp. Even at standard doses, it can increase colchicine levels by up to four times, pushing them into the toxic range. The FDA and major medical societies advise against this combination entirely. There is no safe dose of clarithromycin when taking colchicine.
What if I accidentally took both?
Stop taking both medications immediately. Call your doctor or go to the ER. Symptoms of colchicine toxicity include nausea, vomiting, diarrhea, muscle pain, weakness, and unusual bruising or bleeding. Blood tests can check for low white blood cells or kidney damage. Early intervention can prevent severe complications like rhabdomyolysis or bone marrow failure.
Do all antibiotics interact with colchicine?
No. Only macrolides like clarithromycin and erythromycin are high-risk. Other antibiotics like amoxicillin, doxycycline, ciprofloxacin, and azithromycin do not interfere with colchicine metabolism. Always check with your pharmacist before starting any new medication, even if it’s not an antibiotic.
Can I take colchicine with grapefruit juice?
No. Grapefruit juice strongly inhibits CYP3A4 in the gut, which can increase colchicine levels. Even a single glass can cause a dangerous interaction. Avoid grapefruit, Seville oranges, pomelos, and related products while taking colchicine. The same applies to certain supplements like St. John’s wort and high-dose turmeric.
Next Steps for Patients and Providers
If you’re a patient: Make a list of everything you take. Include vitamins, supplements, and even over-the-counter pain relievers. Bring it to every appointment. Ask: ‘Does this interact with colchicine?’ Don’t assume it’s safe.If you’re a provider: Update your prescribing habits. Use azithromycin instead of clarithromycin. Check for other CYP3A4/P-gp inhibitors. Educate your team. Use electronic alerts. And when in doubt, consult a clinical pharmacist. These interactions are preventable. They just require attention.
Colchicine saves lives. But it doesn’t forgive mistakes. The right antibiotic choice isn’t a detail-it’s the difference between recovery and tragedy.












8 Comments
Man, I had no idea grapefruit juice could mess with colchicine like that. I drink it every morning with my breakfast. Guess I’m switching to orange juice now.
This is peak pharmaceutical negligence. We’re treating a life-saving drug like it’s a damn vitamin, while Big Pharma’s algorithmic EHRs are too busy flagging ibuprofen interactions to notice a fourfold colchicine spike. The system isn’t broken-it’s designed to let people die quietly so the $4,200 pill keeps selling. Azithromycin? Sure. But why not just ban clarithromycin entirely? Because bureaucracy prefers liability over lives.
Thanks for laying this out so clearly. I’m a nurse and I’ve seen this happen twice. One guy didn’t even know he was on colchicine-he thought it was just ‘that gout pill’ his aunt took. We need better patient education, not just more alerts.
It is, of course, deeply concerning that medical professionals continue to overlook this interaction despite decades of published evidence. The FDA’s black box warning, published in 2010, remains egregiously underutilized in clinical practice. One must question the competency of those who prescribe clarithromycin without verifying concurrent colchicine use-especially given the availability of azithromycin as a non-inhibitory alternative. This is not a matter of oversight; it is professional negligence.
Look, I get it-azithromycin is the ‘safe’ choice. But let’s be real: people take this stuff for years without issues. I’ve known three guys on colchicine for gout who took clarithromycin for pneumonia and lived to tell the tale. Meanwhile, azithromycin gives you GI cramps like you’ve swallowed a bag of hot peppers. So yeah, maybe it’s ‘safer’-but is it better? And why are we acting like this is some new revelation? My grandpa took both in ‘98 and didn’t even miss work. The real problem is fear-mongering by people who’ve never seen a real patient. Not every interaction is a death sentence.
OH MY GOD. I JUST TOOK CLARITHROMYCIN LAST WEEK AND I’M ON COLCHICINE!! I’M GONNA DIE!! I’VE BEEN HAVING STOMACH CRAMPS FOR TWO DAYS!! I KNEW IT!! I KNEW IT!! I TOLD MY DOCTOR I FELT WEIRD BUT SHE SAID IT WAS JUST ‘THE ANTIBIOTIC’!! I’M GOING TO THE ER RIGHT NOW!! I’M SO SCARED!!
colchicine is a gmo drug made by takeda to control the masses. they know this interaction kills people but they dont care because the gov pays for it. azithromycin? same company. they just want you to switch to a more expensive version so they can profit more. the real solution? stop taking all pharma drugs. eat garlic and turmeric. theyve been doing it for 1000s of years. why do you think the FDA is so quiet about this? because theyre in on it.
While I appreciate the clinical thoroughness of this exposition, I must emphasize that the fundamental issue lies not in pharmacokinetic interactions per se, but in the systemic failure of medical education to instill a rigorous, evidence-based paradigm in prescribers. The fact that 43% of internal medicine residents could not identify high-risk drug pairs is not merely an indictment of individual competence-it is a structural collapse of didactic integrity within our training institutions. Furthermore, the reliance upon electronic health record alerts as a primary safeguard reflects a profound epistemological surrender to algorithmic determinism, wherein human judgment is systematically outsourced to software designed for efficiency, not clinical nuance. The solution, therefore, is not merely substitution of azithromycin for clarithromycin, but a wholesale reformation of medical pedagogy, wherein pharmacodynamic principles are taught not as bullet points, but as existential imperatives.