When you pick up a prescription at the pharmacy, you might see two options: the brand-name drug you asked for, or a cheaper generic version. Many people wonder-are generic drugs really as safe and effective as the brand-name ones? The answer isn’t just yes-it’s backed by a detailed, science-driven system that’s been refined over 40 years. The U.S. Food and Drug Administration (FDA) doesn’t just approve generics because they’re cheaper. They approve them because they must meet the same exact standards for safety, strength, quality, and performance as the original brand-name drug.
What the FDA Actually Requires for Generic Drugs
The FDA doesn’t treat generic drugs like second-class products. Every generic must prove it’s a true copy-not just in appearance, but in how it works inside your body. This process starts with three non-negotiable requirements: identical active ingredient, same strength, same dosage form, and same route of administration. If your brand-name pill is 50 mg taken by mouth, the generic must be exactly that. No exceptions.
But here’s where most people get confused: generics don’t have to look the same. They can be a different color, shape, or size. They can use different fillers, dyes, or flavors. These are inactive ingredients-things that help with manufacturing or taste, but don’t affect how the drug works. The FDA allows these differences because they don’t change the drug’s effect. But if those inactive ingredients cause an allergic reaction? That’s flagged and tracked.
How Bioequivalence Proves a Generic Works the Same Way
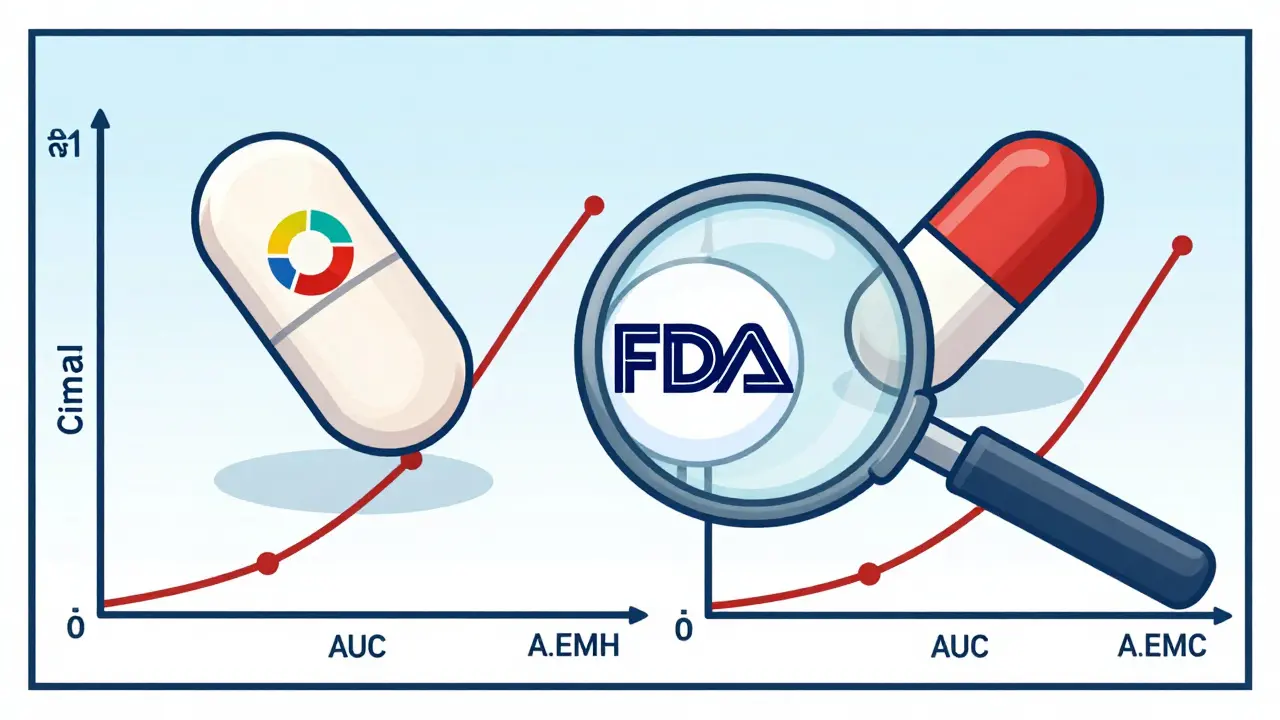
The real test isn’t just chemistry-it’s biology. The FDA requires every generic to prove bioequivalence. That means the generic must deliver the same amount of active ingredient into your bloodstream at the same rate as the brand-name drug. This is measured using two key metrics: Cmax (how high the drug peaks in your blood) and AUC (how much of the drug is absorbed over time).
The FDA’s rule is strict: the 90% confidence interval for both Cmax and AUC must fall between 80% and 125% of the brand-name drug’s values. That’s not a guess. It’s based on decades of clinical data showing this range ensures the same therapeutic effect. For most drugs, this works perfectly. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, or phenytoin-the bar is higher. Here, the acceptable range tightens to 90-111%. Why? Because even a small difference in blood levels can cause serious side effects or make the drug ineffective.
These tests are done in healthy volunteers, usually 24-36 people per study. Each study costs between $1 million and $2 million. That’s not cheap. But it’s cheaper than running full clinical trials-which is exactly why generics are affordable. The brand-name company already did the heavy lifting. The generic maker just has to prove they can match it.
Manufacturing Standards Are Just as Strict
It doesn’t matter how well a drug works in a lab if it’s made in a dirty factory. That’s why the FDA requires all generic manufacturers to follow Current Good Manufacturing Practices (cGMP). These rules cover everything: how equipment is cleaned, how raw materials are tested, how batches are recorded, and how quality control is maintained.
Every generic drug factory-whether it’s in Ohio, India, or China-must pass an FDA inspection before it can ship products to the U.S. The agency conducts over 3,500 inspections a year, and nearly half of them are overseas. In 2022, the FDA launched a Risk-Based Facility Assessment program that increased inspection coverage of foreign plants by 22%. That’s not a coincidence. It’s a response to past issues with contaminated or substandard products.
Impurities are another big focus. The FDA follows international guidelines (ICH Q3B and ICH M7) to set limits on harmful byproducts. For example, any potential carcinogen must stay below 1.5 micrograms per day. That’s a tiny amount-about the weight of a grain of salt split into 600 parts. The FDA uses advanced testing to detect even trace levels, and any batch that fails is rejected.

Labeling: Same Warnings, Same Instructions
Generic drug labels must be identical to the brand-name label in every way that matters-dosage instructions, side effects, warnings, contraindications. The only allowed differences are the manufacturer’s name, package size, and inactive ingredients. No hiding risks. No downplaying side effects. If the brand-name label says “may cause dizziness,” so does the generic.
In 2022, the FDA proposed a major change: allowing generic manufacturers to update safety labels on their own, without waiting for the brand-name company to act first. Before this, only the original drugmaker could submit a “Changes Being Effected” (CBE-0) supplement. That meant patients could be exposed to outdated warnings for years. This change-still under review as of 2025-could make generics safer than ever.
Complex Drugs Are the New Challenge
Not all drugs are created equal. Simple pills? Easy to copy. Inhalers? Creams? Injectables? Much harder. For complex products like asthma inhalers, topical creams, or biologics (like insulin or rheumatoid arthritis drugs), proving equivalence isn’t just about blood levels. It’s about particle size, viscosity, spray pattern, or how the drug binds to cells.
The FDA reports that ANDAs for these complex generics have a 25% higher rejection rate than standard pills. In 2022, 40% of complex generic applications were initially refused because the data didn’t meet standards. That’s not a flaw in the system-it’s proof the system works. The FDA doesn’t approve them just because they’re cheaper. They approve them only when they can prove they work the same way.
Some companies have pushed back. Teva, for example, petitioned the FDA in 2013 to require immunogenicity testing for generic versions of Copaxone (glatiramer acetate), arguing that standard bioequivalence tests couldn’t detect immune reactions. The FDA didn’t immediately require it-but it did create new guidance for complex biologics. That’s how the system evolves: through evidence, not pressure.
Real-World Evidence: Do Generics Actually Work?
Numbers don’t lie. In 2022, generics made up 90% of all prescriptions filled in the U.S.-over 8.4 billion prescriptions. Yet they accounted for only 23% of total drug spending. That’s $610 billion saved in one year.
But do they work? A 2022 JAMA Internal Medicine study of 38,000 Medicare patients found no difference in outcomes between brand and generic statins. Another analysis of 12,500 patient reviews on Drugs.com showed 87% reported no difference in effectiveness for cardiovascular drugs. Neurologists surveyed in 2021 were 68% confident in generic epilepsy drugs. Those are strong numbers.
But there are exceptions. A Reddit thread in early 2023 with over 1,200 comments showed that 32% of users taking generic levothyroxine reported changes in energy, weight, or mood. The FDA’s bioequivalence range for levothyroxine is 90-111%-tighter than normal. But even then, some patients report differences. Why? Possibly due to slight variations in inactive ingredients affecting absorption, or psychological expectations. The FDA still considers them equivalent. But many endocrinologists now recommend sticking with one brand or generic-no switching back and forth.

What You Should Know Before Switching
If you’re taking a generic drug and feel fine? Keep taking it. The system works for the vast majority. But if you’re on a narrow therapeutic index drug-like thyroid meds, blood thinners, or seizure medications-talk to your doctor before switching between generics or between generic and brand. Even small changes can matter.
Also, don’t assume all generics are the same. There can be multiple generic versions of the same drug, made by different companies. If you notice a change in how you feel after switching from one generic to another, tell your pharmacist and doctor. It’s rare-but it happens.
The FDA’s system isn’t perfect. It’s constantly adapting. New tools like AI are being tested to predict impurities faster. More funding is being directed toward complex generics. But the core principle hasn’t changed: if a generic drug is approved, it’s because the FDA has verified it performs the same as the brand-name version.
Why This Matters
Generic drugs aren’t just about saving money. They’re about access. Without them, millions of people couldn’t afford their medications. A heart medication that costs $300 a month as a brand name might cost $12 as a generic. That’s the difference between taking it every day or skipping doses. And skipping doses? That leads to hospitalizations, strokes, and deaths.
The FDA’s job isn’t to make drugs cheap. It’s to make sure cheap drugs are still safe. And so far, the system has delivered.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards for safety, strength, quality, and performance as brand-name drugs. They must contain the same active ingredient, work the same way in the body, and be manufactured under the same quality controls. The only differences are in color, shape, flavor, or inactive ingredients-none of which affect safety or effectiveness.
How does the FDA prove a generic drug works the same as the brand?
Through bioequivalence studies. These tests measure how much of the drug enters the bloodstream and how quickly. The FDA requires the generic’s absorption rate and peak concentration to fall within 80-125% of the brand-name drug’s values. For high-risk drugs like thyroid or blood thinners, the range is tighter-at 90-111%. These tests are done in healthy volunteers and must meet exact scientific standards.
Why do some people say generic drugs don’t work as well?
A small number of patients report differences, especially with narrow therapeutic index drugs like levothyroxine. This could be due to variations in inactive ingredients affecting absorption, or psychological factors. The FDA considers these drugs bioequivalent, but doctors often recommend sticking with one version-brand or generic-to avoid any potential fluctuations. If you notice a change in how you feel after switching, talk to your provider.
Are all generic drugs the same?
No. Multiple companies can make a generic version of the same drug, and each may use different inactive ingredients or manufacturing processes. While all must meet FDA standards, some patients may respond better to one version over another. If you switch generics and feel different, don’t assume it’s your condition changing-ask your pharmacist to check if the manufacturer changed.
Can I trust generic drugs made overseas?
Yes. The FDA inspects all manufacturing facilities-whether in the U.S., India, China, or elsewhere-before approving a drug. In 2022, nearly half of FDA inspections were overseas. The agency uses a risk-based system to prioritize inspections and has increased oversight of foreign plants by 22% since 2020. If a facility fails inspection, the drug is blocked from entering the U.S.
What’s Next for Generic Drugs?
The FDA is investing in new science to keep up with complex drugs. In 2023, $15 million was allocated to develop AI-driven models that predict impurities and improve bioequivalence testing for inhalers, creams, and biologics. The agency is also working with MIT on machine learning tools to spot dangerous compounds faster. And with GDUFA III funding, approval times have dropped by 35% since 2012.
Generics aren’t going away. They’re growing. In 2022 alone, the FDA approved 1,025 new generic drugs. As more brand-name patents expire, the demand for safe, affordable alternatives will only rise. The system isn’t perfect-but it’s one of the most rigorously tested and transparent drug approval processes in the world. And for millions of people, it’s the only reason they can afford to stay healthy.