Vasculitis Treatment: What Works and How to Manage It
If you or someone you know has been diagnosed with vasculitis, the first question is usually “what can I take to feel better?” The good news is that doctors have several tools—from steroids to newer biologics—to calm the inflammation and keep blood vessels healthy.
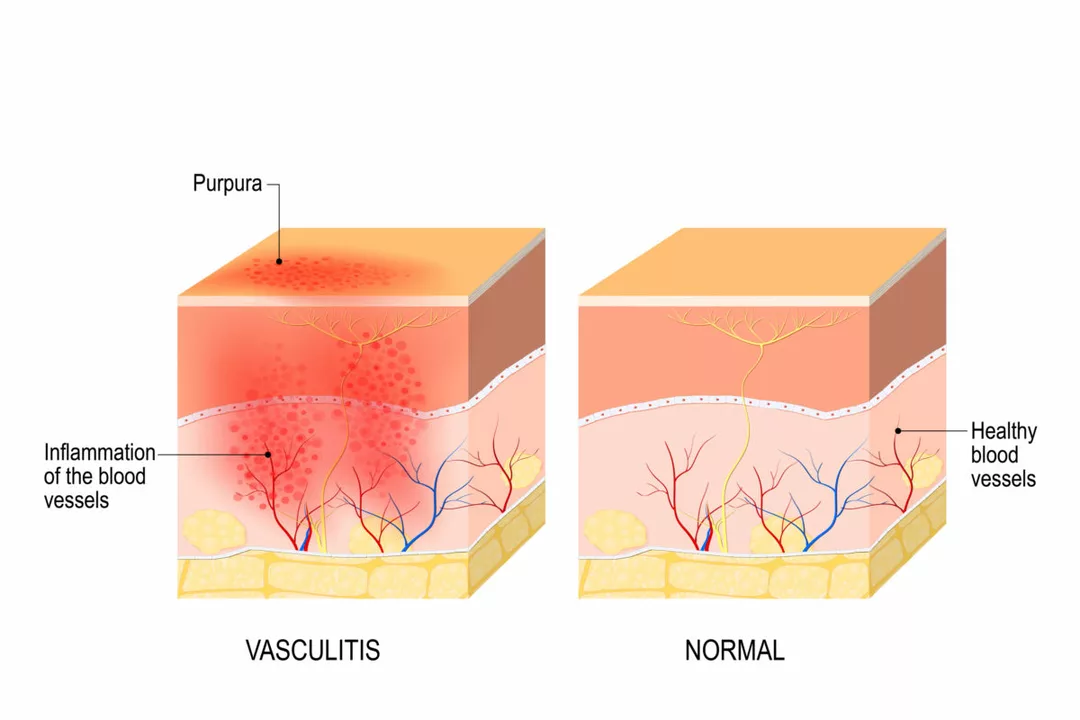
Vasculitis isn’t a single disease; it’s a group of conditions where your immune system attacks vessel walls. Because symptoms range from mild skin rashes to serious organ damage, treatment plans are tailored to what part of the body is involved and how aggressive the inflammation is.
First‑Line Medications
The go‑to prescription for most types of vasculitis is corticosteroids such as prednisone. These drugs work fast, reducing swelling and pain within days. Starting with a higher dose helps bring the flare under control, then doctors taper it slowly to avoid side effects.
Typical steroid side effects include weight gain, mood swings, and higher blood sugar. To keep those in check, many patients add an “steroid‑sparing” drug—often called an immunosuppressant. Common choices are azathioprine, methotrexate or mycophenolate mofetil. These medicines let you lower the steroid dose while still keeping the immune system from attacking your vessels.
If the vasculitis is more severe (for example, affecting kidneys or lungs), doctors may start with cyclophosphamide or rituximab right away. Cyclophosphamide is a powerful chemo‑type drug that shuts down overactive immune cells, but it can hurt the bladder and lower blood counts, so regular lab checks are essential.
When to Try Advanced Therapies
Biologic agents have changed the game for patients who don’t respond to steroids and traditional immunosuppressants. Rituximab, a monoclonal antibody that targets B‑cells, works well for many forms of vasculitis, especially those linked to ANCA antibodies. It’s given as an IV infusion every few months, which means fewer daily pills.
Another option is belimumab or abatacept, though they’re used less often and usually only after other drugs fail. The key with biologics is close monitoring for infections—your immune system will be weaker, so you’ll need to watch for fever, cough, or unusual bruising.
Beyond meds, lifestyle tweaks help keep flare‑ups at bay. Eating a balanced diet rich in omega‑3 fatty acids (think salmon, walnuts) can lower overall inflammation. Regular gentle exercise—like walking or yoga—improves circulation without overtaxing the heart.
Avoid smoking and limit alcohol, because both can worsen blood vessel damage. If you’re on steroids, talk to your doctor about calcium and vitamin D supplements to protect bone health.
Finally, keep a symptom diary. Note any new rashes, joint pain, or changes in urine color, and share that log with your healthcare team. Early detection of a flare can mean a quick medication adjustment and fewer complications.
Managing vasculitis is a partnership between you and your doctor. With the right mix of medications, regular check‑ups, and healthy habits, most people can keep symptoms under control and lead active lives.