When someone you love is struggling with substance use, the fear of an overdose isn’t just a possibility-it’s a real, daily risk. Overdoses don’t always happen in public places or emergency rooms. Most happen at home, where family members are the first-and sometimes only-line of defense. Teaching your family how to recognize the signs of an overdose isn’t about assuming the worst. It’s about being ready to act when every second counts.
What an Overdose Actually Looks Like
Many people think an overdose means someone is passed out or shaking violently. That’s not always true. In fact, the most dangerous overdoses are the quiet ones. Someone might be breathing too slowly, their skin might look gray or blue, and they won’t respond when you shake them or shout their name. These aren’t signs of being "high." They’re signs of their body shutting down. For opioid overdoses-which include heroin, fentanyl, oxycodone, and prescription painkillers-the three key signs are called the "Opioid Triad":- Unresponsive: They don’t wake up when you shake their shoulder or rub your knuckles hard on their sternum (the bone in the center of their chest).
- Slow or stopped breathing: Fewer than one breath every five seconds, or no breathing at all.
- Blue or purple lips and fingernails: This is cyanosis, caused by lack of oxygen. On darker skin tones, this looks more like grayish or ashen skin, especially around the lips and nail beds.
- Body temperature over 104°F (40°C)
- Seizures or uncontrollable shaking
- Chest pain, rapid heartbeat, or confusion
- Extreme agitation or paranoia
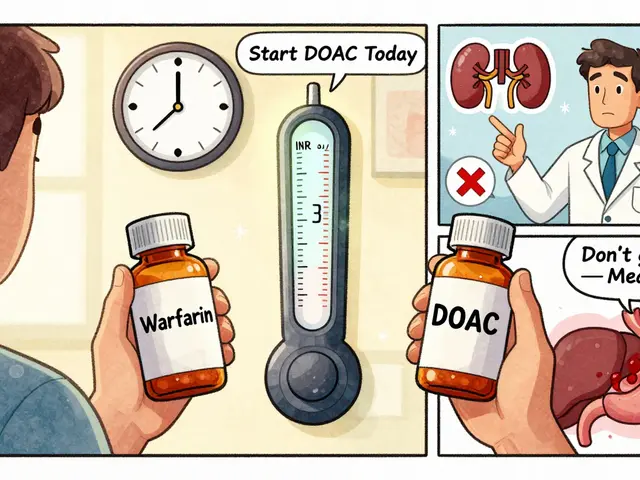
Why Naloxone Is Non-Negotiable
Naloxone (brand name Narcan) is the only medication that can reverse an opioid overdose. It’s safe, easy to use, and works within minutes. But it only works if you have it and know how to use it. In 2023, 31 states allow anyone to get naloxone without a prescription. You can pick it up at most pharmacies for under $40. Some community health centers give it out for free. Don’t wait for a crisis to get it. Keep it in your glovebox, your purse, your coat pocket. If you’re teaching your family, make sure everyone knows where it is. There are two main types: nasal spray and injectable. The nasal spray is the most common for families. It’s simple: peel the package, insert the nozzle into one nostril, and press the plunger. No needles, no training needed. The key is speed. If someone stops breathing, give naloxone within four minutes. After that, brain damage starts. Studies show that if naloxone is given within four minutes, 98% of opioid overdoses can be reversed.How to Teach It-Without Scaring Everyone
You can’t just hand someone a pamphlet and expect them to remember. The CDC found that programs using only lectures had only a 42% skill retention rate after three months. But programs that used hands-on practice? 89% retention. Here’s how to make it stick:- Start with a calm conversation. Say: "I love you, and I’m scared something bad could happen. I want us to be ready, not scared."
- Use a training kit. Buy a naloxone training device (they’re non-functional and cost about $35). Practice on a mannequin or even a pillow. Go through the steps: check responsiveness, call 911, give naloxone, start rescue breathing.
- Practice the "Recognize-Respond-Revive" method. This is the model used by Rady Children’s Hospital and adopted by most health departments:
- Recognize: Look for the triad-unresponsive, slow breathing, blue skin.
- Respond: Yell their name, shake them, rub their sternum. If no response, call 911 immediately. Don’t wait. Say: "I think someone is overdosing. They’re not breathing." Then give naloxone.
- Revive: After giving naloxone, start rescue breathing. Tilt the head back, pinch the nose, give one breath every five seconds. Keep going until they wake up or help arrives.

Don’t Forget Skin Tone Matters
Many training materials only show blue lips on white skin. That’s dangerous. On darker skin, cyanosis looks like gray, ashen, or dull skin-especially around the lips, gums, and nail beds. A 2022 study by the California Department of Public Health found that training programs that included skin tone variations reduced misidentification errors by 63%. Make sure your family knows: blue isn’t the only color to watch for.What to Do After Giving Naloxone
Naloxone wears off in 30 to 90 minutes. Opioids can stay in the body longer. That means someone can stop breathing again after you think they’re fine. That’s why you must:- Stay with them until EMS arrives
- Keep giving rescue breaths if they’re not breathing
- Do not leave them alone-even if they wake up
- Do not assume they’re "out of danger" just because they’re conscious

Real Stories, Real Results
In Georgia, 87 family members trained through a county program later used their skills to respond to actual overdoses. 94% of those people survived. One man in Ohio said he reversed his son’s overdose after practicing with a training kit three times. He said, "I didn’t hesitate. I knew what to do because we’d practiced it like a fire drill." A Reddit user from r/opiatesupport wrote: "I thought training would make me feel like I was expecting the worst. But after I did it, I felt powerful. Like I had a tool I could actually use."Getting Started: Your Action Plan
You don’t need to be a medical professional. Here’s what to do this week:- Ask your pharmacist for naloxone. No prescription needed in most states.
- Buy a training kit (search "naloxone training device" online). They come with step-by-step instructions.
- Set aside 45 minutes. Watch a 10-minute video from Overdose Lifeline or SAMHSA on YouTube.
- Practice the steps together: check, call, give, breathe.
- Keep naloxone in a place everyone knows-like the kitchen drawer or car glovebox.
FAQ
Can I give naloxone to someone who isn’t overdosing?
Yes. Naloxone only works on opioids. If someone isn’t overdosing on opioids, it won’t hurt them. It won’t wake them up if they’re just drunk or high on other drugs. But it won’t harm them either. Better to give it and find out than wait and risk death.
What if I’m afraid to call 911? Will they get in trouble?
In every state, there’s a Good Samaritan law that protects people who call 911 during an overdose. Police won’t arrest someone for drug possession if they’re calling for help. EMS is there to save lives, not punish. Calling 911 is the single most important step.
Is it true that fentanyl makes overdoses harder to recognize?
No-it makes them faster and more dangerous. Fentanyl is 50 to 100 times stronger than morphine. Someone can overdose in seconds. That’s why you can’t wait for obvious signs. If someone is unresponsive and breathing slowly, act immediately. Don’t wait for blue lips. Every second counts.
How often should we practice?
Every three months. Skills fade. Even if you think you’ll never forget, your brain will. Practice the steps like you’re rehearsing for a fire drill. Use the training kit. Review the signs. Make it part of your routine, like checking smoke alarms.
What if I don’t have a training kit? Can I still learn?
Yes. Watch a video from SAMHSA or Overdose Lifeline on YouTube. Practice the motions on a pillow or stuffed animal. Learn the steps: check responsiveness, call 911, give naloxone, start rescue breathing. You don’t need a mannequin to learn the sequence. But if you can get one, do it. It makes a huge difference.









14 Comments
Just picked up two Narcan kits today-one for my car, one for my mom’s purse. 🙏 I told her it’s like a fire extinguisher: hope you never need it, but you’re damn glad it’s there. We practiced on a pillow last night and I swear, I felt less scared after. This stuff saves lives, not just in theory. Real talk: I’m keeping one in my wallet now.
Man, this is the kind of post that makes me glad I’m not alone in this. In India, nobody talks about this-like it’s taboo. But my cousin OD’d last year and we had zero idea what to do. I’m printing this out and showing my family. No more silence. We’re getting trained. Period.
While the intent of this post is commendable, the clinical accuracy is marred by oversimplification. Naloxone’s efficacy is not 98% across all scenarios-it varies by opioid potency, co-ingestants, and time to administration. Furthermore, the assertion that 'blue lips' are the primary indicator ignores the heterogeneity of presentations, particularly in polydrug overdoses. This kind of messaging risks creating false confidence.
Bro, I’ve been thinking-what if this whole overdose thing is just Big Pharma’s way to sell more Narcan? I mean, why do they even make fentanyl so strong? And why is it everywhere now? Smells like a controlled rollout to me. Also, I heard the government’s putting trackers in the nasal spray. Don’t believe the hype. Just sayin’.
I read this quietly over coffee. It’s heavy. My brother’s been clean for three years, but I still keep the kit in the drawer. Not because I expect the worst-but because I refuse to be helpless if the worst comes. I didn’t know about the skin tone thing. That’s critical. Thanks for including it.
You know, I used to think that teaching people about overdose signs was like inviting doom into the house, like saying the words would make it happen-but that’s not how it works at all. It’s like learning CPR or how to use a defibrillator. It’s not morbid, it’s responsible. I sat my whole family down last weekend-we watched the SAMHSA video, practiced on a pillow, and even made a little checklist with sticky notes on the fridge. My 14-year-old daughter said, ‘So if someone’s not breathing, we just do the thing?’ And I said, ‘Yep. And you’ll be the hero.’ It felt like we were finally doing something real. I didn’t cry. I just felt… lighter. Like we weren’t just waiting anymore.
Get the kit. Know the triad. Practice the steps. Call 911. Stay. Breathe. That’s it. No fluff. Just do it.
Let’s be real-this whole ‘teach your family’ thing is just guilt-driven performative activism. People don’t want to save lives, they want to feel like heroes without changing anything. Meanwhile, the real problem is the system that lets drugs flood neighborhoods and then hands out Narcan like bandaids. You’re not fixing anything-you’re just buying time for the same cycle to repeat. And don’t get me started on how they’re pushing this as a substitute for treatment.
My aunt used Narcan on her grandson last month. He’s 19. She didn’t know how to use it until she watched a 5-minute TikTok. Now she carries it everywhere. 🥹 I told her she’s a superhero. She said, ‘Nah, I just didn’t want to lose him.’ We all need to be like her. 💪❤️
Why are we even letting people have this stuff without counseling? You give someone Narcan and they just go right back to using. It’s enabling. You’re not helping them-you’re letting them keep destroying their life. If you love someone, you don’t hand them a lifeline so they can jump again. You make them face the consequences. This post is dangerous.
It is imperative to note that the pharmacokinetic profile of naloxone necessitates continuous monitoring post-administration due to its shorter half-life relative to many synthetic opioids, particularly fentanyl analogues. Furthermore, the reliance on non-clinical personnel for intervention introduces significant variability in response fidelity, thereby undermining the predictive validity of the proposed protocols. Standardization through certified medical oversight remains the gold standard.
I didn’t know about the gray skin thing on darker skin tones. I’ve seen people panic and say ‘they’re fine, they’re just sleeping’-and I used to think that too. I watched a video last night where a woman recognized it on her brother and saved him. I cried. Not because it was sad-but because I realized I could’ve done that. I’m getting a kit this week. And I’m teaching my sister-in-law. She’s scared. I told her: you don’t have to be brave. You just have to be ready.
This is a most commendable and humane contribution to public health discourse. In my country, such knowledge is often inaccessible due to stigma and lack of infrastructure. I shall translate this into Pidgin English and circulate it among community groups. The emphasis on practice over theory is especially vital. May God bless those who share such wisdom.
Just saw your comment about the skin tone thing. I had no idea either. My cousin is Black and I always thought blue lips were the only sign. I’m gonna rewatch the video and show my whole family again. Thanks for pointing that out. 🙏