Sarcoptes Scabiei: What the Scabies Mite Does to Your Skin
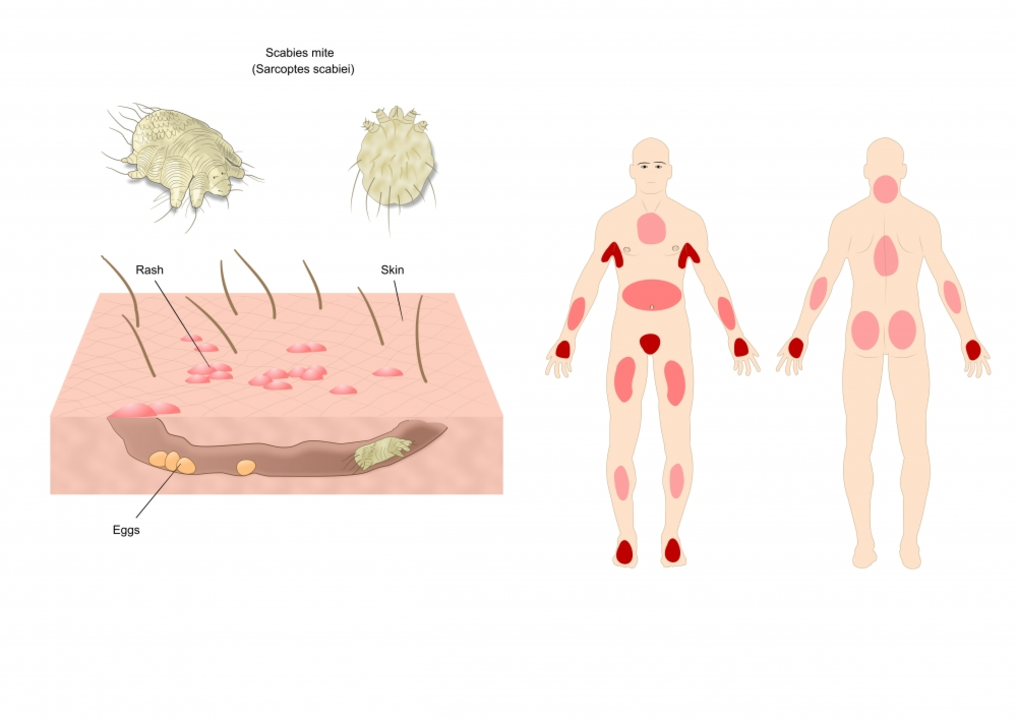
If you’ve ever heard the word "scabies" you probably picture an itchy rash that won’t quit. That rash is caused by a tiny creature called sarcoptes scabiei. It’s a microscopic mite that burrows under your skin and lays eggs, leading to intense itching and red bumps.
Most people catch it through close skin‑to‑skin contact – think sharing a bed, hugging, or even playing sports. You can also pick it up from clothing, towels, or bedding that an infected person has used. The mite doesn’t jump, so you need direct contact for it to spread.
Spotting the Signs Early
The first clue is a rash that gets worse at night. Look for tiny, thread‑like lines (called burrows) on wrists, between fingers, elbows, waistline, and even on the genitals. These burrows feel like sandpaper under your skin.
If you scratch a lot, you might see secondary infections – yellow crusts or pus. In kids, the rash can spread to the face and scalp, which is less common in adults.
How to Get Rid of It
The fastest way to clear scabies is with prescription creams like permethrin 5% or oral medication such as ivermectin. Apply the cream from neck down (or all over for babies) and leave it on for the recommended time, usually eight hours.
After treatment, wash all clothing, towels, and bedding in hot water (at least 50°C/122°F) and dry on high heat. Items that can’t be washed should be sealed in a plastic bag for at least three days – the mites won’t survive without a host.
Even if symptoms improve quickly, finish the full course of medication. Stopping early can let any surviving mites cause another round of infection.
Preventing Re‑Infection
Talk to everyone you’ve been in close contact with – family, friends, roommates – and have them treat at the same time. This stops a cycle where one person gets cured only for the mite to come back from someone else.
Avoid sharing personal items like towels or clothing until everyone finishes treatment. Keep your nails trimmed so scratching doesn’t break the skin and invite bacterial infections.
If you work in close‑contact jobs (healthcare, childcare, hospitality), follow workplace guidelines for scabies outbreaks – they often recommend treating all staff members even if only a few show symptoms.
When to See a Doctor
If the rash lasts more than two weeks after treatment, or if you notice spreading redness, fever, or pus, get medical help. Those could be signs of a secondary infection that needs antibiotics.
A doctor can confirm scabies with a skin scraping under a microscope, but most of the time they’ll diagnose based on your description and look at the rash.
Remember, scabies is common worldwide – you’re not alone. Quick treatment, good hygiene, and treating close contacts will get you back to normal fast.