Pharmaceutical Disruptions: Understanding Drug Safety, Bioequivalence, and Real-World Risks
When we talk about pharmaceutical disruptions, unexpected changes in how medications behave in the body due to formulation, timing, or patient factors. Also known as medication variability, it's not just about brand vs. generic—it’s about how your body reacts to tiny differences that no label ever mentions. These disruptions can mean the difference between feeling better and feeling worse, even when the pill looks identical.
One of the biggest sources of pharmaceutical disruptions is generic drugs, medications that contain the same active ingredient as brand-name versions but may differ in inactive ingredients, coatings, or manufacturing processes. Many assume generics are exact copies, but the truth is more complicated. A pill from one batch might release the drug slightly faster than another, especially if you’re sensitive to fillers like lactose or dyes. That’s why some people report side effects with one generic but not another—even though both are labeled the same. These aren’t myths; they’re documented in studies on bioequivalence, the measure of how similarly two drug formulations perform in the body. The FDA allows a 20% variability range in absorption, and while that’s legal, it’s not always safe for everyone. If you’re on blood pressure meds, epilepsy drugs, or thyroid medication, even small shifts in absorption can throw off your whole routine.
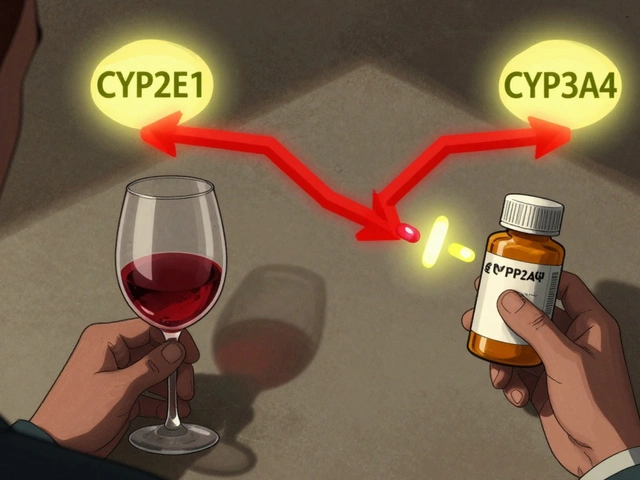
Then there’s drug interactions, when one medication changes how another works, either by competing for absorption, altering metabolism, or affecting organ function. These aren’t always between two pills. High-protein meals can block levodopa from reaching your brain if you have Parkinson’s. Taking blood pressure meds at night instead of morning can reduce dizziness and bathroom trips. Even stress can worsen chapped skin if you’re on steroids. These aren’t side effects you’ll find in a brochure—they’re real, personal, and often overlooked by doctors who assume all patients respond the same.
And let’s not forget medication safety, the practice of using drugs in ways that minimize harm while maximizing benefit. It’s not just about avoiding overdoses. It’s about knowing when to split pills safely, when to question a black box warning, or why your doctor might suggest switching from one antihypertensive to another. It’s about understanding that a drug labeled "safe" doesn’t mean it’s right for you. That’s why so many posts here focus on patient experiences—because the science tells us what’s possible, but real life tells us what actually happens.
What you’ll find below isn’t just a list of articles. It’s a collection of real-world fixes, hidden risks, and quiet breakthroughs—everything from how batch variability affects your heart meds, to why trust in generics matters more than price, to how timing your pill can cut your side effects in half. These aren’t theoretical debates. They’re the things people learn the hard way. And you don’t have to.