Switching from a brand-name respiratory inhaler to a generic version might seem like a simple cost-saving move - until you realize the device itself is part of the medicine. Unlike pills, where swapping one generic for another usually works without issue, respiratory combination inhalers are far more complex. The drug isn’t the only thing that matters - the inhaler’s design, how it delivers the medication, and how you use it can make or break your treatment.
Why Inhalers Aren’t Like Pills
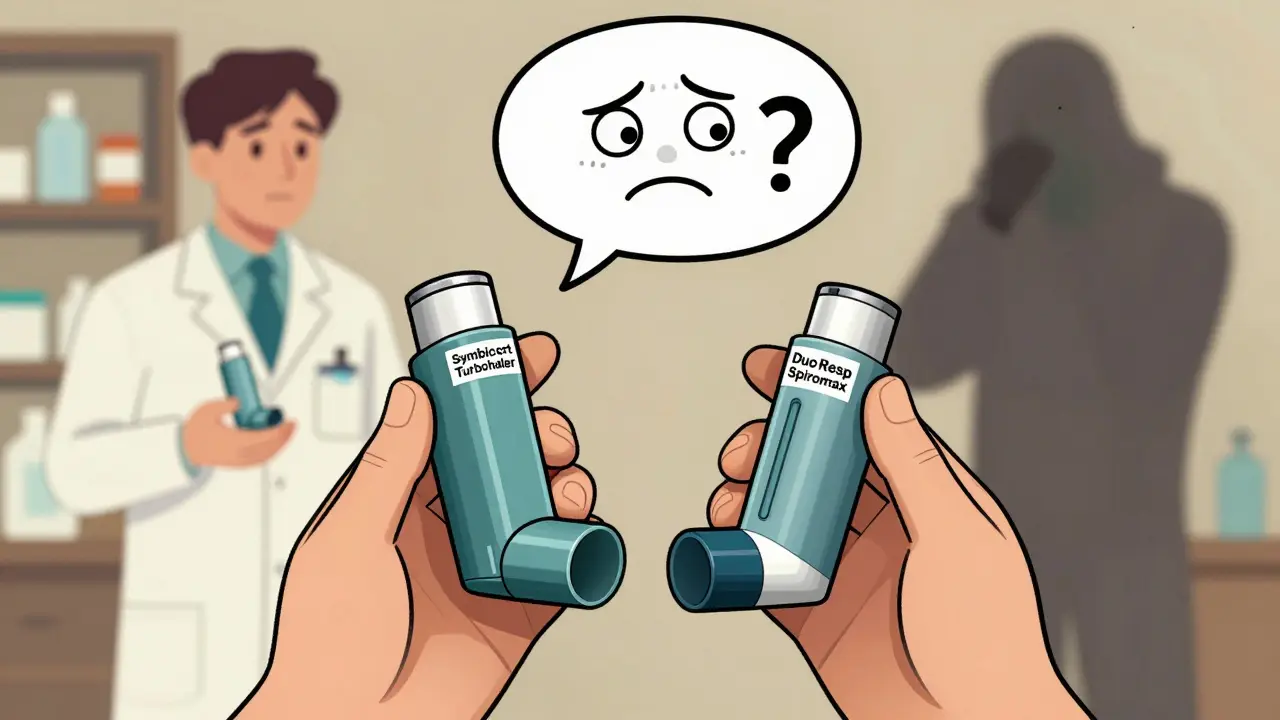
Think of a respiratory combination inhaler as a system: two drugs (usually a corticosteroid and a long-acting beta agonist) delivered through a specific device. Brands like Symbicort Turbohaler and Advair Diskus have been the gold standard for years. But as patents expire, generics are flooding the market. The problem? Many of these generics aren’t just cheaper versions of the same device - they’re different devices entirely.
Take DuoResp Spiromax. It contains the same drugs as Symbicort Turbohaler: budesonide and formoterol. But the device? Totally different. Turbohaler requires you to twist the base to load a dose. Spiromax uses a side slider. One needs a slow, deep breath. The other needs a sharp, forceful inhale. If you’ve been using Turbohaler for years and suddenly get switched to Spiromax without instruction, you’re not just getting a different inhaler - you’re getting a different treatment.
A 2020 study found that 76% of patients switched without training used the new device incorrectly. That’s not a small number. That’s three out of every four people. And those mistakes? They lead to more asthma attacks, more hospital visits, and more emergency care.
How Different Devices Change Everything
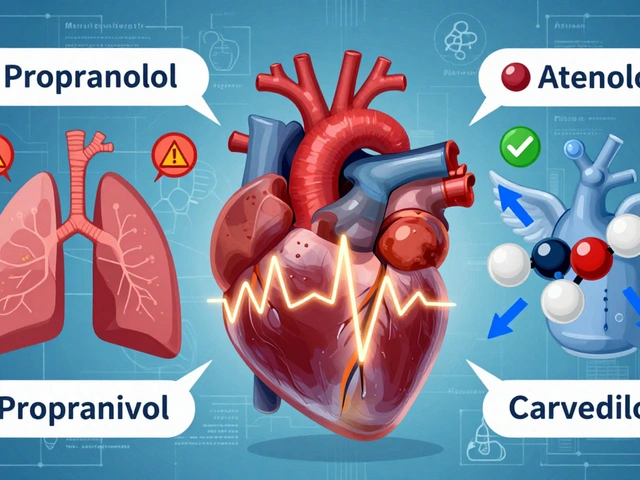
There are three main types of inhalers: pressurized metered-dose inhalers (pMDIs), dry powder inhalers (DPIs), and nebulizers. Each works differently.
- pMDIs (like older versions of Ventolin) need perfect timing - press the canister and breathe in at the same time. Most people get this wrong.
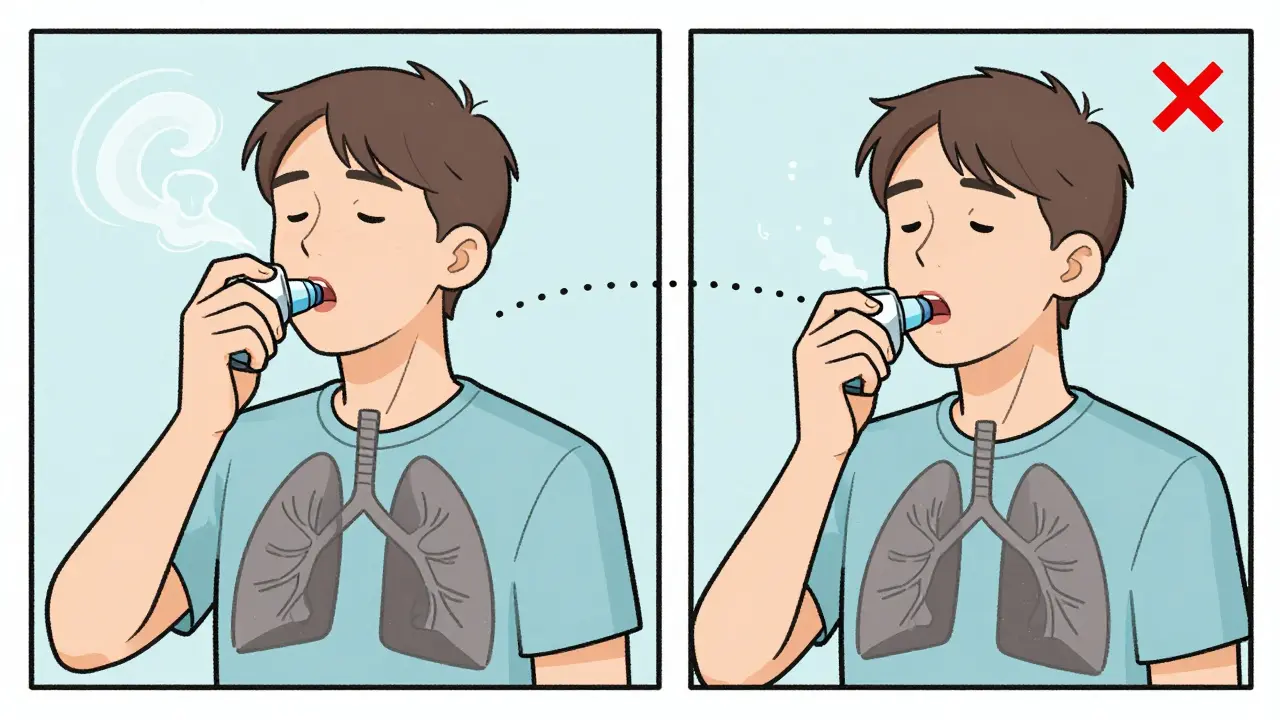
- DPIs (like Turbohaler or Spiromax) don’t need coordination. But they demand strong, fast inhalation to pull the powder into the lungs. If you breathe too slowly, the medicine stays in your mouth.
The difference in technique isn’t subtle. It’s the difference between getting the full dose and getting almost nothing. Studies show lung deposition can vary by 25-40% between devices with the same drugs. That’s like taking a 10mg pill one day and a 6mg pill the next - and not knowing why your symptoms got worse.
Global Rules, Different Results
Not every country handles this the same way. In the U.S., the FDA allows automatic substitution. Their stance? If the generic meets bioequivalence standards, it’s fine to switch without warning. But clinical evidence says otherwise.
In Europe, the EMA takes a harder line. They require proof that the generic performs the same in real-world use - not just in labs. They demand comparative studies on lung delivery, patient outcomes, and even how easy it is to use correctly. The UK’s NICE guidelines go even further: they explicitly warn against automatic substitution, saying it can lead to worse asthma control.
The numbers back this up. A 2021 study showed patients switched from Symbicort Turbohaler to Spiromax without training had a 22% increase in asthma exacerbations within six months. That’s not a fluke. That’s a pattern.
What Patients Are Saying
Real people are feeling the impact. On Reddit’s r/asthma community, 83% of users who were switched to a generic inhaler without warning reported worsening symptoms. One woman wrote: “I didn’t know I had to breathe harder. My asthma got so bad I ended up in the ER.”
A 2022 survey by Asthma UK found 57% of patients were confused after a switch. One in three had at least one emergency visit in the three months after being switched. On Drugs.com, Symbicort Turbohaler has a 6.2/10 rating. DuoResp Spiromax? 4.8/10. Common complaints: “harder to use,” “feels less effective,” “I don’t trust it anymore.”
But here’s the flip side: when patients get proper training, success rates jump. One 2022 study found 89% of people using generic inhalers correctly had been shown how to use them - by a nurse, pharmacist, or doctor - and then asked to demonstrate it back.
The Training Gap
Healthcare providers are caught in the middle. A study from the NIH found general practitioners needed an average of 12.7 minutes of training just to confidently demonstrate both Turbohaler and Spiromax techniques. And 43% couldn’t do it right at first.
Pharmacies? Even worse. A 2022 survey by the American Pharmacists Association found only 28% of community pharmacies consistently offer device-specific training when substituting inhalers. Why? Time. Most pharmacies are rushed. Counseling takes minutes - and those minutes aren’t paid for.
Germany requires pharmacists to spend 15 minutes in person with every first-time inhaler user. The U.S.? No federal mandate. That’s why so many patients get left in the dark.

What Should You Do?
If you’re on a combination inhaler - whether it’s for asthma or COPD - here’s what you need to know:
- Never assume your inhaler hasn’t changed. If your refill looks different, ask. Don’t just use it.
- Ask your doctor or pharmacist: “Is this the same device as before? If not, can you show me how to use it?”
- Use the teach-back method. After they show you, do it yourself. If you can’t, they need to try again.
- Watch for warning signs. More coughing? More shortness of breath? More rescue inhaler use? That’s not normal. That’s a red flag.
- Request brand-name if needed. In many places, you have the right to refuse substitution. Say so.
It’s not about being anti-generic. It’s about being pro-safety. A cheaper inhaler that doesn’t work right isn’t saving money - it’s costing you your health.
The Bigger Picture
The global market for respiratory inhalers hit $38.7 billion in 2022. Generics now make up about 18% of sales. But the hidden cost? $1.2 billion a year in avoidable hospital visits and ER trips, according to IMS Health. That’s money spent because people were switched without training.
Guidelines are shifting. GINA’s 2023 update now says: “Device familiarity and correct technique should be prioritized over generic substitution.” The European Respiratory Society says prescribe by brand name to avoid errors. The FDA is now requiring more clinical endpoint studies for inhaler generics - a direct response to the evidence.
Smart inhalers are starting to help. Devices with sensors that track your technique and send feedback to your phone have cut exacerbations by 33% in studies. But they’re still expensive and not widely available.
The truth? Generic substitution for inhalers isn’t a simple swap. It’s a medical procedure. And like any procedure, it needs informed consent, proper instruction, and follow-up.
Can I switch to a generic inhaler without asking my doctor?
No, you shouldn’t. Even if your pharmacy automatically substitutes, you have the right to ask for the same device you’ve been using. Many generic inhalers use different devices, and using them without proper instruction can lead to poor medication delivery, worsening symptoms, or even hospitalization. Always check with your doctor or pharmacist before switching.
Why do some generic inhalers feel less effective?
They’re not necessarily less effective - but they might be delivered differently. A different inhaler design can change how deeply the medicine reaches your lungs. If you’re used to a slow, deep breath with one device and now have to use a forceful inhale with another, you might not be getting the full dose. That’s why patients often say the generic “feels less effective.” It’s not the drug - it’s the device.
Are all generic inhalers the same?
No. Two generics with the same drugs can use completely different devices. For example, one might be a dry powder inhaler (DPI) with a twist mechanism, while another uses a slider. The drug might be identical, but the delivery system isn’t. Always check the device name on the box - not just the drug names.
How can I tell if I’m using my inhaler correctly?
Ask your doctor or pharmacist to watch you use it. Then, repeat the steps yourself - this is called the “teach-back” method. If you’re unsure, record yourself or ask for a demonstration video. Many clinics have these. Also, watch for signs: if you taste the medicine in your mouth, cough after inhaling, or need your rescue inhaler more often, you’re likely not using it right.
What should I do if my inhaler was switched without warning?
Stop using it. Contact your doctor or pharmacist immediately. Ask if the new inhaler is the same device as before. If not, request a return to your original device or schedule a training session. Don’t wait until symptoms worsen. Early action can prevent an emergency.
Final Thoughts
Generic substitution for inhalers isn’t a win-win. It’s a trade-off - lower cost, higher risk. And the risk isn’t theoretical. It’s in hospital records, patient stories, and clinical studies. The medicine is only as good as the way it’s delivered. If you’re not using the device right, you’re not getting the treatment you need.
Don’t let a pharmacy decision override your health. Ask questions. Demand training. Know your device. Your lungs depend on it.






9 Comments
I just got switched to this new generic inhaler last month, and I didn't realize how different it felt until I started coughing nonstop after every use. I thought I was just getting sick, but then I read this post and it clicked - I never got trained on the new device. I'm going to call my pharmacy tomorrow and demand a demo. No more guessing with my lungs.
So let me get this straight - we’re okay with swapping life-saving inhalers like they’re different flavors of gum? The FDA says ‘eh, close enough,’ while people are ending up in ERs because they didn’t know they had to ‘snap’ their breath instead of ‘sigh’ it? I’m not mad, I’m just disappointed in our healthcare system’s idea of innovation.
Y’all, I was skeptical at first - like, why would a device change matter? But after my cousin got switched and ended up in the hospital, I did some digging. Turns out, the difference between a twist and a slide isn’t just ‘kinda different’ - it’s like switching from a manual transmission to a self-driving car without ever learning to drive. Your body doesn’t just adapt. It panics. And if you’re not taught how to use it? You’re basically on your own. Please, if you’re on a combo inhaler - ask. Ask. ASK. It’s not being high-maintenance, it’s being smart.
It is imperative that healthcare providers and pharmacists recognize that device-specific instruction is not ancillary - it is a critical component of therapeutic efficacy. The absence of standardized training protocols constitutes a systemic failure in patient safety. Without mandatory demonstration and competency verification, generic substitution protocols are not merely cost-saving measures - they are potential public health hazards.
So the FDA lets pharmacies swap these things like candy, but the EMA and NICE are like, ‘hold up, let’s not kill people.’ Funny how the country with the most expensive healthcare also has the most laissez-faire attitude toward life-saving devices. I’m not surprised, but I’m still furious.
India has been using generic inhalers for over a decade with zero issues. Why? Because we don’t coddle patients. If you can’t figure out how to use a device, maybe you shouldn’t be breathing. This American obsession with hand-holding is why your healthcare costs are insane. Just teach them once, then let them figure it out. No one needs a 15-minute tutorial. My uncle used three different inhalers in 10 years - never went to the hospital. You’re all overreacting.
There is an epistemological paradox here: if the efficacy of a drug is contingent upon the fidelity of its delivery mechanism, then the ‘generic’ is not a generic at all - it is a qualitatively distinct therapeutic agent. Yet we persist in labeling it as interchangeable. This is not a pharmacological equivalence problem - it is a linguistic and ontological one. The word ‘generic’ implies sameness, but the device renders it heterogenous. We have confused semantics with substance.
Listen, I’ve been on Symbicort for 12 years and when they switched me to Spiromax without warning, I thought I was dying. I went to three different doctors, two ERs, and finally found a nurse who actually knew what she was doing. She showed me how to breathe - not just ‘inhale,’ but like you’re trying to suck a milkshake through a straw that’s two miles long. I’ve been using it right ever since. But guess what? My pharmacist didn’t even ask if I knew how to use it. She handed me the box and said, ‘It’s cheaper.’ That’s not healthcare. That’s retail. And if you’re okay with that, you’re not just naive - you’re dangerous.
I used to think generics were great. Now I think they’re a trap.