FDA MedWatch: Understanding Drug Safety Reports and How to File Them
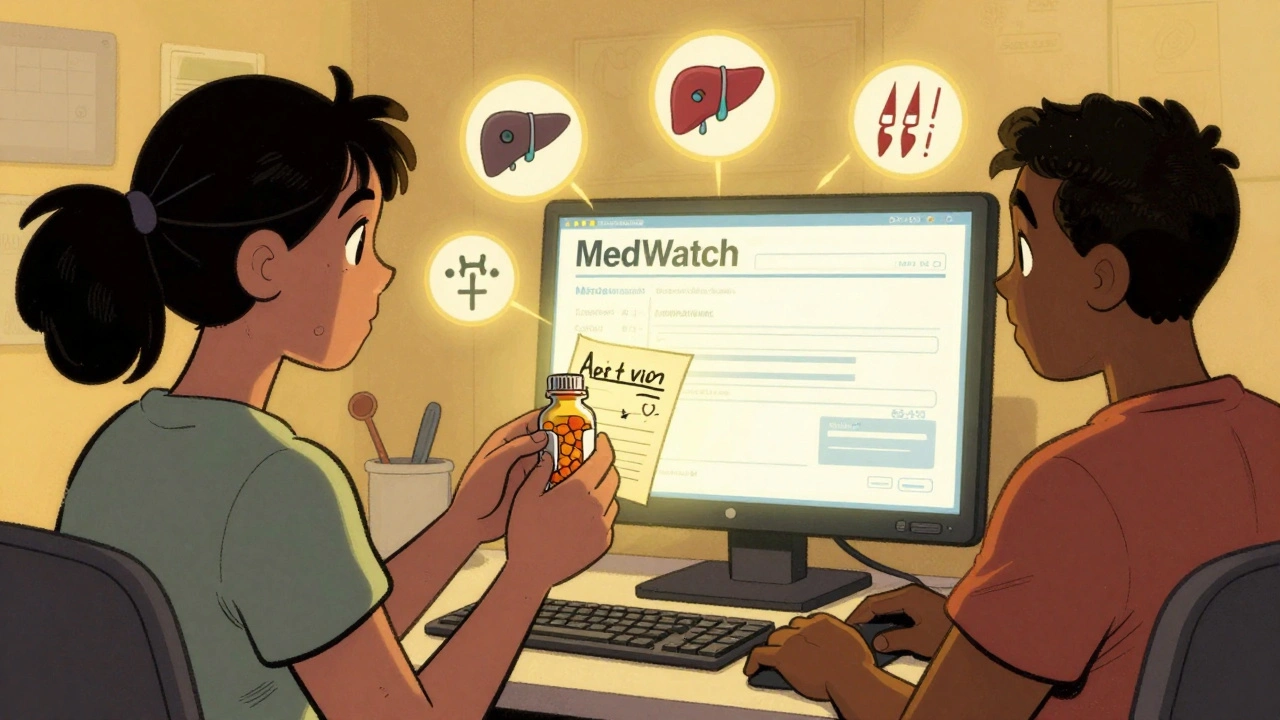
When a drug gets approved, the work isn’t done. The FDA MedWatch, the U.S. Food and Drug Administration’s program for collecting reports of adverse drug reactions and product problems. Also known as MedWatch, it’s the frontline system that catches hidden dangers after a medication is already in use by millions. Brand-name drugs go through clinical trials with a few thousand people. But real-world use? That’s thousands of different bodies, habits, and health conditions. That’s where MedWatch comes in — it’s how patients, doctors, and pharmacists tell the FDA when something goes wrong.
MedWatch isn’t just for pills. It covers vaccines, medical devices, dietary supplements, and even cosmetics. A bad reaction to a generic blood thinner, a faulty insulin pump, or a supplement that causes liver damage — all of these can be reported. The system doesn’t just collect complaints. It turns them into action. When enough people report the same issue, the FDA can update warning labels, require new safety studies, or even pull a drug off the market. In 2020, over 1.2 million reports came in through MedWatch. Many of them came from regular people like you who noticed something off and decided to speak up.
Related entities like adverse drug events, unexpected or harmful reactions to medications that aren’t listed on the label and post-market surveillance, the ongoing monitoring of drugs after they’re approved for public use are the backbone of MedWatch. These aren’t abstract terms — they’re the reason your doctor might warn you about a new side effect, or why a medication guide suddenly adds a black box warning. The FDA doesn’t magically know these things. It learns from reports. And those reports often come from people who noticed dizziness after taking a new generic, or a rash that showed up weeks after starting a new antidepressant.
What you’ll find in the posts below is a collection of real-world cases where safety reports, monitoring gaps, and hidden risks turned into urgent conversations. From how generic drugs behave differently across batches to why black box warnings on antidepressants may have had unintended consequences, these stories show how MedWatch isn’t just paperwork — it’s a living system shaped by patient experience. You’ll read about how drug shortages during COVID-19 led to dangerous substitutions, how biosimilars are tracked for safety, and how even herbal remedies like Rumalaya can trigger unexpected reactions. These aren’t theoretical concerns. They’re the kind of issues that show up in MedWatch reports every day.
If you’ve ever wondered whether your side effect was "normal" — or if you’ve been told to just "wait it out" — know this: your report matters. You don’t need to be a doctor. You don’t need to prove anything. Just describe what happened, when, and what you were taking. That’s all it takes to help someone else avoid the same problem. The system only works if people use it. And below, you’ll find the tools and knowledge to understand what’s being reported — and how to add your voice to it.