Parlodel (Bromocriptine) vs. Alternative Dopamine Agonists: A Complete Comparison
Compare Parlodel (bromocriptine) with other dopamine agonists, weigh benefits, side‑effects, dosing, and choose the right option for prolactinoma and beyond.
When working with bromocriptine, a dopamine agonist that lowers prolactin and improves motor function. Also known as BC, it plays a key role in managing several endocrine and neurological conditions. As a dopamine agonist, a drug that stimulates dopamine receptors in the brain, bromocriptine influences hormone release, mood regulation, and movement control. This dual action means it can both reduce excess prolactin and help restore normal motor activity, making it valuable for patients dealing with hormonal imbalances and Parkinson’s‑related stiffness. In short, bromocriptine bridges the gap between endocrine therapy and neuro‑pharmacology.
One of the most common reasons doctors prescribe bromocriptine is to treat Parkinson's disease, a progressive neurological disorder characterized by tremor, rigidity, and slowed movement. By activating dopamine receptors, the drug compensates for the dopamine shortage that drives those motor symptoms. At the same time, bromocriptine is effective against prolactinoma, a benign pituitary tumor that overproduces the hormone prolactin. Lowering prolactin levels relieves symptoms like unwanted lactation, menstrual irregularities, and infertility. These two applications illustrate a core semantic triple: bromocriptine treats Parkinson's disease and bromocriptine reduces prolactin in prolactinoma patients. Another important link is between bromocriptine and hyperprolactinemia, a condition marked by elevated prolactin that can cause sexual dysfunction and bone loss. By acting as a dopamine agonist, bromocriptine directly suppresses the hormone’s release, helping restore normal reproductive function and protect bone health. This relationship shows that dopamine agonists influence hormone regulation, a principle that extends beyond bromocriptine to other drugs in the same class. While bromocriptine shines in these areas, it also interacts with medications that affect blood clotting, such as the antiplatelet agent dipyridamole, which appears in our site’s other guides. Unlike dipyridamole, which prevents platelet aggregation, bromocriptine’s primary actions are neurological and endocrine. Understanding that distinction helps patients avoid confusion when reading about drug comparisons. In practice, the safety profile of bromocriptine includes common side effects like nausea, headaches, and dizziness, but serious concerns—such as sudden hypotension or hallucinations—are rare and usually tied to high doses or pre‑existing conditions. For anyone considering bromocriptine, dosage starts low and is gradually increased to minimize discomfort. Typical regimens begin at 1.25 mg daily for prolactin‑related issues and may climb to 5 mg or higher for Parkinson’s disease, always under medical supervision. Regular monitoring of blood pressure, heart rate, and hormone levels ensures the therapy stays on track. If you’re also taking antidepressants, be aware that bromocriptine can amplify serotonin activity, so a doctor’s guidance is essential. Overall, bromocriptine serves as a bridge between hormone control and movement improvement, offering a unique solution for two very different health challenges. Below you’ll find a collection of articles that dig deeper into its mechanisms, compare it with other dopamine agonists, and provide practical tips for safe use.
Compare Parlodel (bromocriptine) with other dopamine agonists, weigh benefits, side‑effects, dosing, and choose the right option for prolactinoma and beyond.
Learn how to safely buy cheap generic tetracycline online, check pharmacy legitimacy, understand dosage, side effects, and avoid scams.
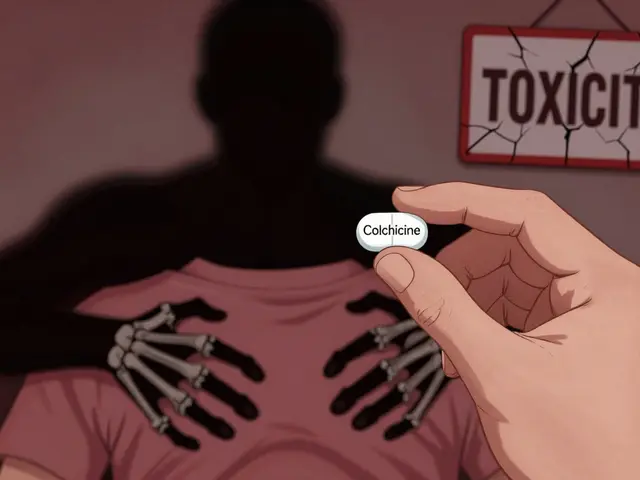
Colchicine and macrolides like clarithromycin can cause life-threatening toxicity due to combined CYP3A4 and P-gp inhibition. Azithromycin is the only safe macrolide option. Know the risks and how to avoid them.
Cardiac MRI and echocardiography both image the heart, but they serve different purposes. Learn when each is used, how accurate they are, and why one might be chosen over the other for your diagnosis.

Hydroxychloroquine is a cornerstone treatment for lupus arthritis, reducing joint inflammation, preventing flares, and protecting against organ damage. Learn how it works, why it's recommended for nearly all SLE patients, and how to use it safely.
Epilepsy surgery can offer freedom from seizures for those with drug-resistant epilepsy. Learn who qualifies, what the risks really are, and what outcomes patients can expect - backed by current medical data.
