Blood Thinners: What They Are, How They Work, and What to Watch For
When your blood starts clotting too easily, blood thinners, medications that reduce your blood’s ability to form dangerous clots. Also known as anticoagulants or antiplatelets, they keep clots from blocking arteries or veins — which could cause a stroke, heart attack, or pulmonary embolism. These aren’t just for older adults. People with atrial fibrillation, artificial heart valves, deep vein thrombosis, or even some genetic conditions rely on them daily. But they’re not harmless. Even small mistakes — skipping a dose, mixing with certain foods, or taking another drug — can turn them from lifesavers into dangers.
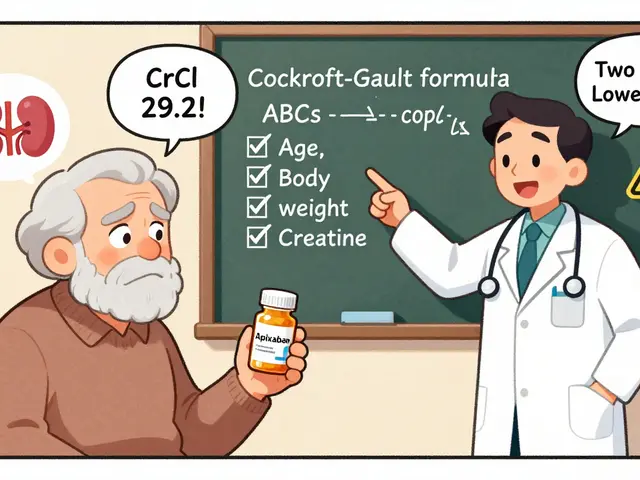
There are two main types: anticoagulants, like warfarin or apixaban, that slow down the chemical process behind clotting, and antiplatelets, like aspirin or clopidogrel, that stop blood cells called platelets from sticking together. You might think all blood thinners work the same, but they don’t. Warfarin needs regular blood tests to check your INR levels. Newer ones like rivaroxaban or dabigatran don’t, but they’re pricier and harder to reverse if you bleed. And yes — they interact with cinnarizine, a vertigo drug that can increase bleeding risk when mixed with anticoagulants, just like alcohol, NSAIDs, or even some herbal supplements. That’s why reading your medication guides, the plain-language warnings the FDA requires for high-risk drugs isn’t optional. It’s how you spot red flags before they turn into emergencies.
People on blood thinners often worry about bleeding, but the bigger issue is consistency. Missing a dose raises your clot risk. Taking too much raises your bleeding risk. Even something as simple as switching from one generic brand to another can throw off your levels — not because the active drug changed, but because of differences in fillers or how fast it’s absorbed. That’s why batch variability, small differences between production lots of the same generic drug, matters more than you think. And if you’re also managing high blood pressure, diabetes, or heart failure, your blood thinner doesn’t exist in a vacuum. It’s part of a system. That’s why team-based care — where your doctor, pharmacist, and nurse all talk to each other — works better than trying to manage this alone.
Below, you’ll find real, practical advice on how to read your medication labels, avoid dangerous interactions, understand what to do if you bleed, and even how timing your dose can reduce side effects like dizziness or frequent urination. You’ll see how other drugs like eplerenone or cinnarizine can change the game. And you’ll learn why some people need blood tests while others don’t — and what to do if you’re unsure. This isn’t theory. It’s what people on blood thinners actually need to know to stay safe, every single day.