Bioequivalence: What It Really Means for Generic Drugs
When you pick up a generic pill, you expect it to do the same job as the brand-name version. That’s where bioequivalence, the scientific standard that proves two drug formulations release the same amount of active ingredient at the same rate in the body. Also known as pharmacokinetic equivalence, it’s the invisible rule that keeps your blood pressure, diabetes, or depression meds working the way they should. But bioequivalence isn’t a magic guarantee—it’s a measured range, and that range matters more than you think.
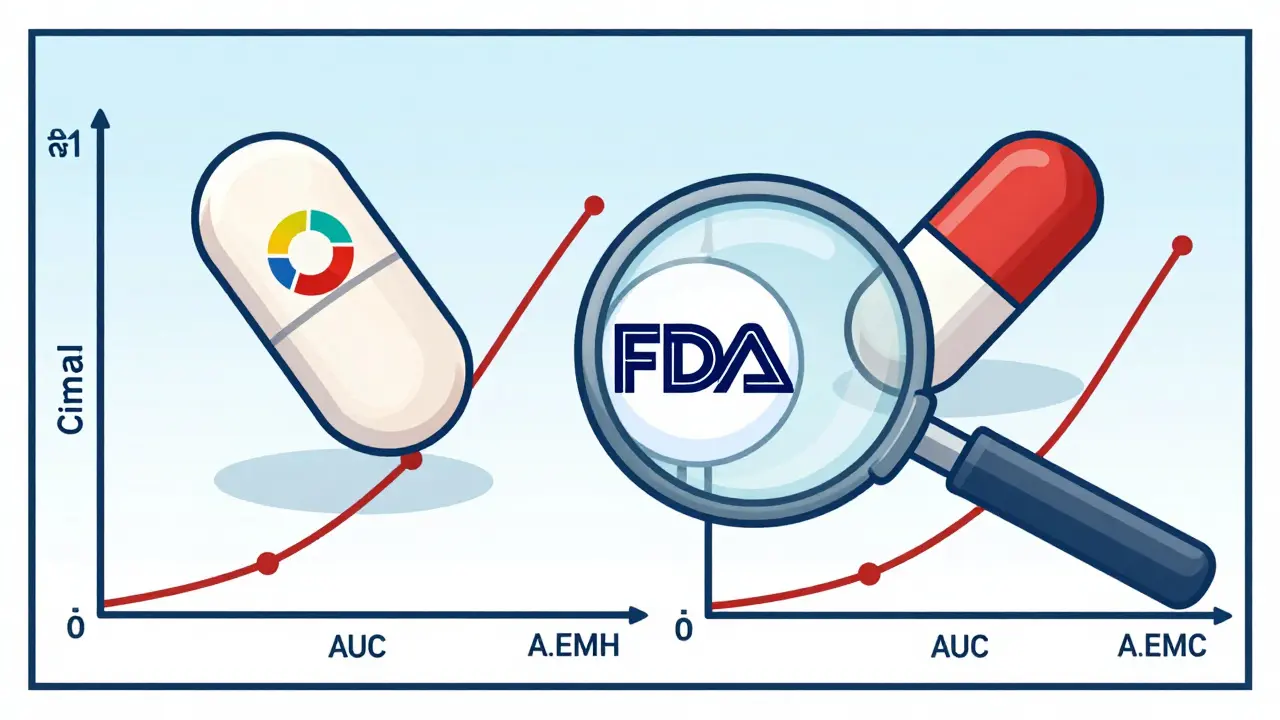
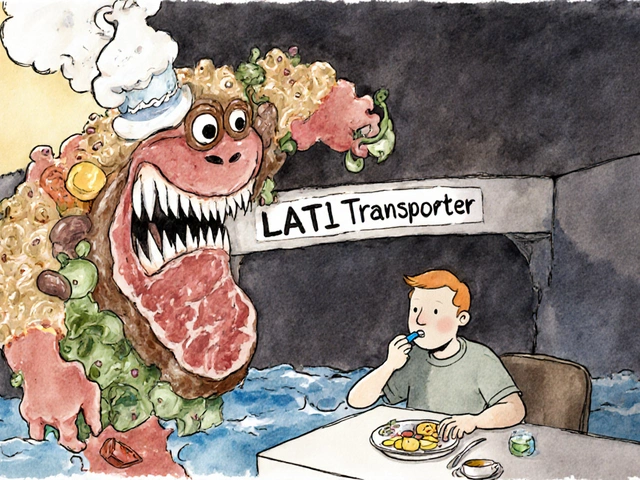
Behind every generic drug is a batch variability, the natural differences in how each production run performs, even when made to the same formula. One batch might absorb 95% of the active ingredient, another 88%. Regulatory agencies like the FDA and EMA allow this, as long as it stays within 80% to 125% of the brand-name drug’s performance. That’s the official bioequivalence standards, the legal thresholds that define acceptable performance differences between generics and brand-name drugs. But here’s the catch: if you switch between multiple generic brands over time, your body might be getting slightly different doses each time. For some people—especially those on narrow-therapeutic-index drugs like warfarin or levothyroxine—that small shift can mean the difference between control and crisis.
That’s why pharmacokinetic variability, how your body absorbs, processes, and eliminates a drug over time isn’t just a lab term. It’s your real-world experience. Maybe you noticed your blood pressure creeping up after switching generics. Or your seizures returned after a refill from a different manufacturer. These aren’t coincidences—they’re signals that bioequivalence limits, while technically met, don’t always feel equal to your body. The latest research shows that even within approved ranges, some generic batches cause more side effects or reduced effectiveness, especially in older adults or people with liver or kidney issues.
What you’ll find in the posts below isn’t theory—it’s real patient stories, lab data, and regulatory updates that show how bioequivalence works (and sometimes fails) in everyday life. You’ll see how batch differences affect blood pressure meds, why some generics cause unexpected reactions, and how to tell if your medication isn’t performing as it should. No fluff. No marketing. Just what you need to know to spot the gaps between the label and your actual health.