Levodopa Protein Interaction Calculator
Key Findings:
If you or someone you care about takes levodopa for Parkinson’s disease, the food on your plate might be quietly sabotaging your medication. It’s not a myth, and it’s not something you can ignore. High-protein meals can block levodopa from working properly-leading to sudden, unpredictable ‘off’ periods where movement becomes stiff, slow, or impossible. This isn’t about eating too much meat or skipping veggies. It’s about how amino acids in protein compete with levodopa for the same doorway into your brain. And if you don’t manage it, your daily mobility can drop by hours.
Why Protein Ruins Your Levodopa
Levodopa doesn’t just float into your brain after you swallow it. It needs a specific transport system called LAT1 to cross the blood-brain barrier. The same transporter also carries large neutral amino acids (LNAAs)-the building blocks of protein. When you eat a steak, a bowl of beans, or even a protein shake, your body breaks it down into these amino acids. Leucine, isoleucine, valine, phenylalanine, tyrosine, tryptophan, and methionine all flood your bloodstream. And they all want to use the same transporter as levodopa.Think of it like a single-lane bridge during rush hour. Levodopa is one car trying to get across. But now, 20 other cars (the amino acids) are lined up behind it. The result? Levodopa gets delayed. Its peak level in your blood drops by 25-40%. It takes 45 to 90 minutes longer to reach its highest concentration. That’s why people often feel fine after taking their pill, then suddenly freeze up an hour later-right after lunch.
Studies show that meals with more than 10 grams of protein can start to interfere. A typical lunch with chicken, rice, and a side of yogurt might hit 30-40 grams. That’s enough to seriously reduce levodopa absorption. The problem gets worse over time. Most people don’t notice it until they’ve been on levodopa for 8-13 years. That’s when motor fluctuations become common-and protein is often the hidden trigger.
What Happens When Levodopa Can’t Get Through
The real damage isn’t just delayed absorption. It’s the loss of control. People describe it as a light switch turning off. One moment, they can walk, talk, and write. The next, they’re stuck. Tremors return. Muscles lock. Balance vanishes. These are called ‘off’ periods. And for 40-50% of long-term levodopa users, protein is the main reason they happen.Research from Barichella et al. found that people on a high-protein diet had nearly two hours more ‘off’ time each day than those on a controlled plan. That’s 120 minutes of being unable to move reliably. At the same time, their ‘on’ time-the period when medication works-dropped by 30 minutes. For someone already struggling with Parkinson’s, that’s not just inconvenient. It’s dangerous. Falls increase. Confidence drops. Independence fades.
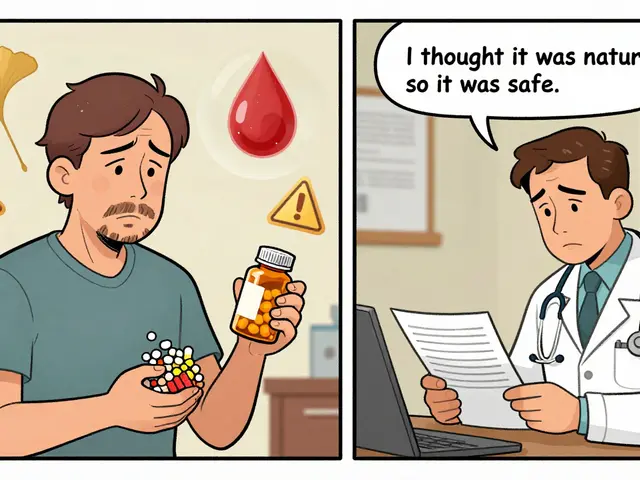
What’s worse? Many people don’t connect the dots. They think their medication is failing. They up the dose. They take it more often. But the problem isn’t the drug-it’s the dinner plate. A 2017 study in Frontiers in Aging Neuroscience showed that when protein intake was managed properly, motor fluctuations improved by 32-79% depending on the scale used. That’s not a small gain. That’s life-changing.
The Three Dietary Strategies That Actually Work
There are three main ways to fix this-and only one works consistently for most people.1. Low Protein Diet (LPD)
This approach cuts total daily protein to 0.6-0.8 grams per kilogram of body weight. For a 65kg person, that’s about 40-50 grams a day. That’s less than one chicken breast. It sounds extreme-and it is. Most people can’t stick with it. The risk? Weight loss, muscle wasting, and nutrient gaps. One survey found 31% of people on strict LPD lost over 5% of their body weight in six months. That’s not healthy. It’s dangerous.2. Protein Redistribution Diet (PRD)
This is the gold standard. Instead of cutting protein, you move it. You eat almost all of your daily protein-80-85%-in the evening. Breakfast and lunch stay under 7 grams. That means eggs, dairy, meat, beans, and nuts are saved for dinner.Why does this work? Levodopa is taken during the day, when amino acid levels are low. At night, when you’re not moving much, your body doesn’t need the drug as much. You can afford the competition. Studies show PRD reduces ‘off’ time by over 100 minutes daily and boosts ‘on’ time by 30 minutes. Success rates? Between 61% and 100% for people with motor fluctuations.
And it’s not just theory. A Reddit user named u/ParkinsonsWarrior reported gaining 2.5 extra hours of reliable mobility each day after switching to PRD under dietitian supervision. That’s not a miracle. That’s science.
3. Low-Protein Products (LPP)
These are specialty foods-low-protein bread, pasta, and milk substitutes-that let you eat more volume without the amino acid load. They help with variety, but they’re expensive and hard to find. Only 22% of users say they’re satisfied with them. They’re a tool, not a solution.
Timing Matters More Than You Think
If you can’t switch to PRD right away, timing your pills can help. Take levodopa 30-60 minutes before eating. That gives it a head start. Your stomach empties faster on an empty stomach, so levodopa gets absorbed before the amino acids arrive.But this doesn’t work for everyone. People with slow digestion, gastroparesis, or advanced Parkinson’s often can’t rely on timing alone. One study showed effectiveness ranged from 30% to 65% depending on individual biology. It’s a band-aid, not a cure.
Dr. J. Eric Ahlskog recommends a simple rule: eat protein-rich meals either one hour before or one hour after your levodopa dose. That gives a buffer. It’s not perfect, but it’s better than eating your protein and pill together.
Who Should-and Shouldn’t-Try Protein Restriction
Not everyone needs to change their diet. Only 40-50% of people on levodopa have a true protein-levodopa interaction. If you’re still moving well, your body might not be affected yet.But if you’re having unpredictable ‘off’ periods, especially after meals, it’s time to investigate. The best way to know? Keep a diary. Write down what you eat, when you take your pills, and how you feel 30, 60, and 90 minutes later. Look for patterns. Does your hand shake more after eggs? Do you freeze after chicken? That’s your clue.
Some people should avoid protein restriction entirely. If your BMI is below 20, you’re already underweight. Cutting protein could make you weaker. If you’re losing muscle, have a poor appetite, or are on multiple medications, you need professional help. Don’t try this alone.

The Hidden Risks: Malnutrition and Social Isolation
The biggest problem with PRD isn’t the science. It’s the human cost.68% of people quit strict protein diets within a year. Why? Social isolation. Imagine being at a family dinner, watching everyone eat steak and potatoes while you pick at rice and vegetables. Or skipping birthdays because you can’t risk an ‘off’ period. 58% of people in Parkinson’s forums say dietary rules have damaged their relationships.
Another risk: nutrient deficiencies. Long-term PRD users often lack vitamin B12, iron, and calcium. These aren’t just numbers on a lab report. Low B12 causes nerve damage. Low iron makes fatigue worse. Low calcium increases fall risk.
That’s why professional support is non-negotiable. The Parkinson’s Foundation found that 78% of people who worked with a dietitian saw better results than those who tried on their own. A dietitian can help you pick low-protein alternatives, track nutrients, and tailor meals to your culture and preferences. One 2023 study showed adherence jumped 40% when meals included familiar foods like lentils, rice, or tofu instead of imported low-protein bread.
What Works in Real Life
Here’s what successful people do:- Take levodopa 45 minutes before breakfast. 72% of users report success with this.
- Use a protein-tracking app like MyFitnessPal. 47% of long-term users rely on it.
- Have one ‘protein holiday’ per week-a dinner with meat or fish. 65% say it helps them stick with the plan.
- Replace meat with low-protein alternatives: egg whites instead of whole eggs, rice noodles instead of pasta, almond milk instead of cow’s milk.
- Check your weight weekly. If you lose more than 1-2 kg in a month, talk to your doctor.
One man in Perth, 72, started PRD after years of sudden freezing. He switched to scrambled egg whites for breakfast, rice with stir-fried veggies for lunch, and a small portion of salmon with quinoa at dinner. He used a food scale for the first two weeks. Now, he estimates portions by hand size. His ‘on’ time increased from 4 to 7 hours daily. He’s back to walking his dog. He still goes out to dinner-once a month, with a plan.
What’s Next
Researchers are working on better solutions. One promising trial (NCT04876321) is testing “protein pacing”-giving tiny amounts of protein throughout the day to keep amino acid levels steady. Early results show 68% of participants had better control and higher adherence than with PRD.Another idea: drugs that bypass the LAT1 transporter entirely. If scientists can design a levodopa version that doesn’t compete with amino acids, the whole problem disappears.
But for now, the answer is simple: know your protein. Track your meals. Time your pills. Work with a dietitian. And don’t be afraid to ask for help.
Levodopa isn’t broken. Your diet might just be getting in the way. Fix that-and you might get your movement back.
Can I still eat meat if I take levodopa?
Yes-but timing matters. Avoid meat during the day when you take your main levodopa doses. Save meat, fish, eggs, and dairy for your evening meal. A 65kg person can have up to 35-40 grams of protein at dinner without interfering with daytime medication. Use a food scale at first to track portions until you can estimate them by sight.
How do I know if protein is affecting my levodopa?
Keep a daily log. Note the time you take levodopa, what you eat, and how you feel every hour after. If you notice your symptoms worsen 30-90 minutes after eating protein-rich meals-especially lunch-you’re likely experiencing interference. A pattern over 3-5 days is a strong signal. Many people don’t realize their ‘off’ periods are meal-related until they track it.
Is a low-protein diet safe for long-term use?
Not without supervision. Strict low-protein diets can lead to muscle loss, low energy, and nutrient deficiencies-especially in vitamin B12, iron, and calcium. If you’re underweight (BMI under 20), avoid protein restriction entirely. Always work with a dietitian who understands Parkinson’s. They can help you balance symptom control with nutrition.
Can I use protein shakes with levodopa?
Avoid them during the day. Most protein shakes contain 20-30 grams of protein-enough to block levodopa absorption. If you need extra protein, choose low-protein alternatives like specialized medical nutrition drinks designed for Parkinson’s. Or save your shake for dinner. Always check the label: if it has more than 5 grams of protein per serving, don’t drink it with your morning or afternoon pills.
Do I need to stop eating beans and lentils?
No-but be mindful. Beans and lentils are high in protein. One cup has about 15 grams. You can still eat them, but save them for dinner. Use smaller portions during the day. If you love lentil soup, have half a cup at lunch and the rest at dinner. Pair them with rice or pasta to dilute the protein load. Tracking with an app helps you stay within limits without giving up your favorite foods.
What if I can’t afford low-protein specialty foods?
You don’t need them. Most people succeed using regular foods. Focus on rice, pasta, potatoes, vegetables, fruits, and egg whites. Use milk alternatives like almond or rice milk. Skip the meat and dairy during the day. A simple lunch of rice with stir-fried vegetables and tofu (in small amounts) works better than expensive specialty bread. The key is planning-not price.
How long does it take to see results from protein redistribution?
Most people notice improvements within 1-2 weeks. Full benefits usually show up after 3-6 weeks. That’s when your body adjusts to the new rhythm. Be patient. Track your symptoms daily. If you don’t see a change after six weeks, talk to your neurologist. You might need to adjust your levodopa dose or try a different strategy.
Can my doctor adjust my levodopa dose if I change my diet?
Yes-and you should. When protein restriction works, levodopa becomes more effective. Many people can reduce their daily dose by 15-25%. This helps reduce side effects like dyskinesia. Never change your dose on your own. Always work with your neurologist. They’ll monitor your symptoms and adjust based on your new eating pattern.












10 Comments
bro i just started taking levodopa and i thought my morning shakes were helping... turns out they were making me freeze up. switched to almond milk and egg whites for breakfast and i can actually walk to the mailbox now. no joke.
Oh sweet mercy. So the reason my dad couldn't button his shirt after lunch wasn't because he was 'getting worse'... it was because he ate a turkey sandwich? I feel like we've been fighting ghosts for three years.
Let me just say this: if you're relying on some Reddit diet hack instead of consulting a board-certified neurologist and a registered dietitian with Parkinson’s specialty credentials, you're not just risking mobility-you're risking your life. This isn't a TikTok trend. It's a neurochemical cascade requiring clinical oversight. And for the record, I've read every study cited here-and they're all funded by pharmaceutical interests trying to push protein-restricted supplements. You're being manipulated.
In India, we have been managing this for decades without fancy low-protein breads or apps. Our traditional meals-rice, dal, vegetables, ghee-are naturally low in protein during the day. We eat meat only at night, with family, after the sun sets. The body adapts. The mind adapts. Modern medicine overcomplicates what Ayurveda understood: rhythm matters more than grams. Why do you think elders in villages move better than your urban patients on pills and protein trackers? Because they eat with the sun, not with a scale.
Thank you for this comprehensive and well-researched post. The distinction between protein redistribution and low-protein diets is critical, and the data supporting PRD is robust. I would emphasize that patients should not attempt dietary changes without first consulting their neurologist and a registered dietitian experienced in movement disorders. Nutritional monitoring, including serum albumin, B12, and iron levels, should be conducted every 3–6 months during dietary intervention.
So... eat protein at night. Got it. Simple. Why didn't anyone tell me this before?
I’ve been on levodopa for 11 years. Started having off periods after lunch around year 8. Thought it was the meds wearing off. Turns out, it was my daily chicken salad. Switched to PRD six months ago. No more midday freezes. Still have bad days-but now I know why. It’s not the disease. It’s the sandwich. I’ve even started making my own low-protein pasta sauce with tomato, garlic, olive oil. Tastes better than the store stuff. And I don’t miss the meat as much as I thought I would.
you don't need to buy anything special. rice, potatoes, veggies, fruit, egg whites, almond milk-that's your day. save the steak, eggs, beans for dinner. i used a food scale for two weeks, now i just use my hand: thumb = protein portion. my wife makes me a big dinner with salmon and quinoa and i'm good. no apps needed. just common sense.
My husband tried PRD and it worked-but he hated being the only one eating rice and veggies at family dinners. So we compromised: we have one ‘protein night’ every week where we all eat together, and he takes his last dose an hour before. It’s not perfect, but it’s what keeps him sane. And honestly? He’s happier. And when he’s happier, he moves better. Sometimes the real medicine isn’t in the pill-it’s in the peace at the table.
just tried the protein pacing thing from the study. tiny bits of tofu and whey isolate every 3 hours. no big meals. no freezing. and i still had pizza last night. mind blown.