When your doctor hands you a prescription for a generic drug, do you feel relieved-or worried? You’re not alone. Millions of people in the U.S. take generic medications every day, saving hundreds or even thousands of dollars a year. But somewhere in the back of their minds, a question lingers: Are generics really the same?
The answer is yes. But knowing that and believing it are two different things. And that gap between facts and feelings is what stops people from fully trusting generic drugs-even when the science is clear.
Why People Doubt Generic Medications
It’s not about being irrational. It’s about perception. Many patients associate the look of a pill with its effectiveness. If your brand-name pill is a blue oval with a logo, and the generic is a white circle with no markings, it’s easy to wonder: Is this really doing the same thing?
That’s not just a gut feeling-it’s backed by data. In Greece, nearly one-third of patients refused a generic because they believed the brand-name version was of higher quality. In the U.S., 24% of patients still doubt generics work as well. Even though the FDA requires generics to be bioequivalent-meaning they deliver the same amount of active ingredient into your bloodstream within the same timeframe as the brand-many don’t know what that actually means.
And then there’s the fear of side effects. One Reddit user shared that their generic Lyrica made them nauseous, while the brand never did. Another said switching from brand Synthroid to generic levothyroxine kept their thyroid levels stable for two years-and saved $300 annually. Both stories are real. Both happen. But the negative experience sticks harder because it feels personal. It’s not a statistic; it’s your body reacting.
What ‘Bioequivalent’ Actually Means
The FDA doesn’t just approve generics because they look similar. They require them to meet strict standards. For a generic to be approved, it must contain the same active ingredient, in the same strength, and work the same way in your body as the brand-name drug. The difference? The inactive ingredients-like fillers, dyes, or coatings-that make the pill look different or easier to swallow.
Here’s the key: bioequivalence means the drug performs the same way in your body. The FDA tests this using blood samples from healthy volunteers. The amount of drug absorbed must fall between 80% and 125% of the brand-name version. That’s not a wide range-it’s tight. It’s like comparing two identical engines: one might have a slightly different paint job, but the horsepower and fuel efficiency are the same.
And here’s something most people don’t realize: the brand-name drug itself was tested against a placebo in clinical trials. The generic doesn’t need to re-prove that. It only needs to prove it matches the brand. That’s why generics are approved faster and cost far less-because the safety and effectiveness of the active ingredient are already proven.
Who Trusts Generics-and Who Doesn’t
Trust in generics isn’t random. It follows patterns. People over 60 are more likely to trust them. Why? They’ve seen more of the system. They’ve been on multiple medications, switched prescriptions, and learned that not every expensive pill is better. In fact, 71% of seniors believe generics are safe.
Employed people also show higher trust-82% say generics are safe. That makes sense. They’re more likely to have insurance with formularies that push generics, and they’ve probably experienced the cost difference firsthand.
But here’s the twist: the more educated someone is, the less they trust generics. That’s not because they know more-it’s because they know more about how complicated the system is. They’ve read about recalls, heard stories about inconsistent manufacturing, or know that some generics come from overseas. That awareness breeds caution.
And then there’s the doctor factor. Patients trust their doctors. If your doctor says, “This generic is just as good,” you’re far more likely to accept it. A study in Greece found that when doctors recommended generics, patients accepted them 87.6% of the time. That’s not because patients are easily convinced-it’s because they trust the person telling them.
How Doctors and Pharmacists Can Build Trust
It’s not enough to say, “It’s the same.” You have to explain why.
Kaiser Permanente created a simple tool: a visual chart showing two pills side by side-one brand, one generic-with arrows pointing to the active ingredient. The chart says: “Same medicine. Different color. Same effect.” They cut refusal rates by 37% in just a few months.
Mayo Clinic takes it further. They assign pharmacists to do 15-minute consultations with patients switching to generics. These aren’t sales pitches. They’re Q&As: “What are you worried about?” “Have you noticed any changes?” “Let’s check your bloodwork in 6 weeks.” That personal touch raised patient satisfaction to 92%.
And pharmacists? They’re the last line of defense. When you pick up your prescription, and the pill looks different, the pharmacist should say something. Not just, “It’s generic.” But: “This is the same medicine your doctor prescribed, just made by a different company. The color changed because they used a different dye, but it works exactly the same. I’ve seen thousands of patients switch with no issues.”
What You Can Do to Feel More Confident
If you’re unsure about a generic, here’s how to take control:
- Ask your doctor: “Is this generic equivalent to the brand? Can you show me the data?” Most doctors have access to FDA bioequivalence reports or can point you to the FDA’s website.
- Check the pill: Use the FDA’s Drug Lookup tool (or ask your pharmacist) to compare the generic and brand pill. Note the active ingredient-they’re identical.
- Monitor your response: If you’re switching for a chronic condition like high blood pressure or thyroid disease, ask for a follow-up blood test in 4-6 weeks. Stable results mean it’s working.
- Know your insurance: Some plans force generic substitution. Others let you opt out. Know your rights. You can always ask for the brand if you’re uncomfortable.
- Track your experience: Keep a simple journal: “Day 1: Took generic. No side effects. Day 7: Still feeling the same.” That data is more powerful than fear.
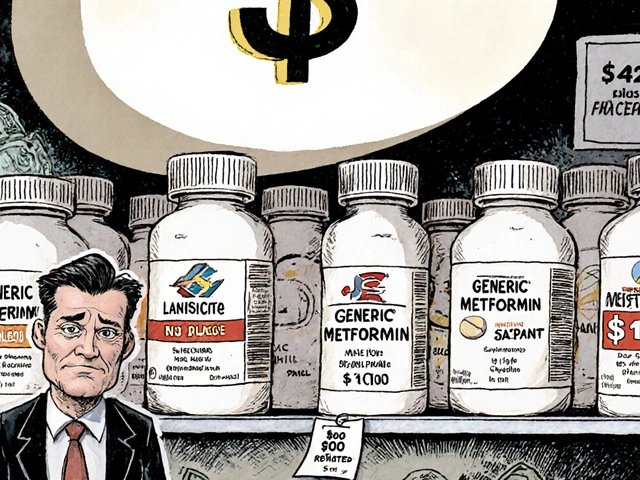
The Real Cost of Not Trusting Generics
Let’s be clear: this isn’t just about saving money. It’s about access.
Generics make life-saving drugs possible for people who otherwise couldn’t afford them. Take apixaban (Eliquis). The brand costs over $500 a month. The generic? Around $15. A Medicare patient in Kansas saved $1,200 a year switching to the generic-and kept her blood clot risk exactly the same.
Now imagine that multiplied across millions of people. In 2023, Americans filled 6.8 billion generic prescriptions. That’s 90% of all prescriptions. But those generics only accounted for 23% of total drug spending. That’s $1.7 trillion in potential savings over the next decade-if people trusted them fully.
But trust doesn’t come from brochures. It comes from consistent, clear, human conversations. From a pharmacist who takes five extra minutes. From a doctor who says, “I’ve prescribed this to my own mother.” From a system that doesn’t hide the fact that pills look different-but explains why that doesn’t matter.
The Future of Generic Trust
The FDA launched a $15 million campaign in early 2024 called “Know Your Options,” targeting myths like “Generics have less active ingredient.” That’s a myth. The law requires generics to contain 90-110% of the active ingredient-same as the brand. The FDA’s own data shows no meaningful difference in effectiveness or safety.
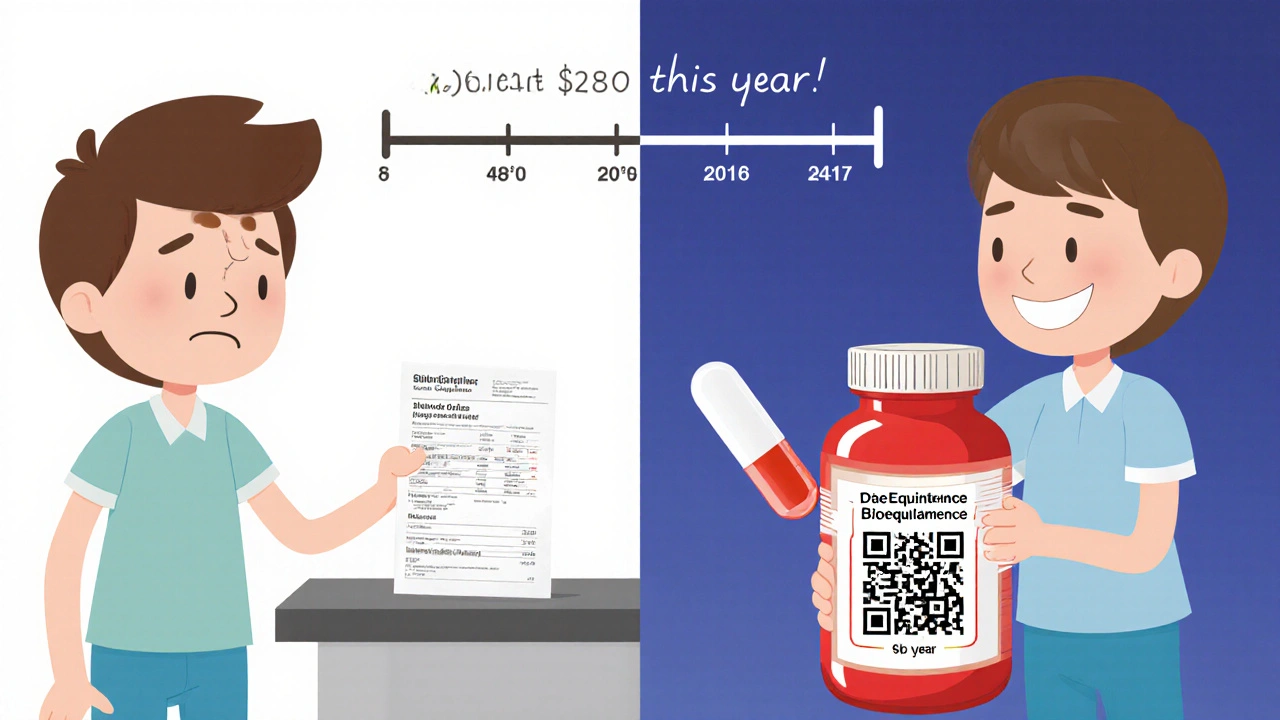
Pharmacies are starting to use QR codes on generic packaging. Scan it, and you see the FDA approval number, the manufacturer, and a short video explaining bioequivalence. CVS Health is testing AI tools that analyze your medication history and send personalized messages: “You’ve taken this generic for 6 months. Your blood pressure is stable. You’ve saved $280 this year.”
And the trend is clear: more brand-name drugs are losing patents. Over 227 will go generic between 2024 and 2028. That means more people will face this decision. More people will need to understand it.
The question isn’t whether generics work. They do. The question is: Will we let fear stop us from using them?







9 Comments
Look, I don’t care what the FDA says. My cousin took a generic version of her antidepressant and started crying in the grocery store for no reason. That’s not bioequivalence, that’s a betrayal. The pill looked different. The packaging felt cheap. My body knows. And so does yours.
Let’s be real-generics are the unsung heroes of healthcare. You think Big Pharma cares about your thyroid? Nah. They care about your wallet. Switching to generic levothyroxine saved me $400/year. My TSH? Perfect. My bank account? Also perfect. Stop letting color and shape dictate your health outcomes. This isn’t a fashion show, it’s medicine.
I’m a nurse practitioner, and I’ve prescribed generics to hundreds of patients over the last 15 years. Not one has had a clinically significant difference in outcomes compared to brand. The science is solid. The FDA’s 80–125% bioequivalence range isn’t a loophole-it’s a precision instrument. When patients ask me, I show them the data. Then I ask them: ‘Would you trust your mechanic if they said your car needed a $2,000 part when a $200 part does the same job?’
Okay, so the FDA says generics are ‘equivalent.’ But who approves the FDA? Who funds the studies? Who owns the labs that test these pills? Let me tell you something-the same conglomerates that make the brand-name drugs also make the generics. Same factories. Same supply chains. Same executives. The only difference? The label. You’re not saving money-you’re being manipulated by a system that wants you to think you’re getting a deal. Wake up.
My dad’s been on generic metformin for 8 years. His sugar’s stable, he’s not in the hospital, and he’s saved enough to take a trip to India last year. I used to be skeptical too-until I saw the numbers. The active ingredient? Identical. The cost? 1/30th. The fear? Totally understandable. But the data? Doesn’t lie. Maybe we need more stories like his, not more fear.
Ever heard of the ‘generic pill cartel’? It’s real. The FDA doesn’t inspect every batch. Most generics come from India and China-countries where they’ve been caught dumping industrial waste into rivers and still shipping pills to the U.S. You think your ‘bioequivalent’ pill is safe? Check the manufacturer code. Then Google it. You’ll see. I did. And I stopped taking generics. My life’s worth more than a $15 co-pay.
I switched to generic Synthroid last year… and… I… didn’t… notice… any… difference… at… all… Seriously… my TSH… has… been… perfect… for… 14… months… I… saved… $320… this… year… and… I… didn’t… feel… weird… or… tired… or… anything… I… just… felt… like… myself…
The efficacy of generic pharmaceuticals is a matter of regulatory fidelity, not perception. The FDA's bioequivalence standards are among the most rigorous in the world. The psychological aversion to altered pill morphology is a well-documented cognitive bias. Education, not coercion, is the solution. Trust is earned through transparency, not slogans.
USA is the only country where you get ripped off by your own government. Generic? Yeah right. That’s just the Chinese government’s way of poisoning our kids with cheap plastic pills. Meanwhile, our doctors are in on it-paid by Big Pharma to push ‘equivalent’ poison. I’d rather pay $500 for Eliquis than let some factory in Bangalore make my heart explode. America First. Pills Last.