Every year, more than 100,000 people in the U.S. die from opioid overdoses. Many of these deaths happen because no one nearby knows how to respond - or worse, they’re afraid to act. The truth is, naloxone can bring someone back from the brink in under five minutes. It’s not magic. It’s medicine. And it’s now available without a prescription in every state.
How Naloxone Works - And Why It’s a Lifesaver
Naloxone is an opioid blocker. It doesn’t cure addiction. It doesn’t treat pain. It simply kicks opioids off the brain’s receptors so breathing can restart. When someone overdoses, their breathing slows or stops. Their brain isn’t getting oxygen. Naloxone steps in fast - usually within 3 to 5 minutes - and reverses that effect. It’s like hitting a reset button on the body’s breathing system.
It works on all opioids: heroin, oxycodone, fentanyl, morphine, even prescription pain pills. But here’s the key: it only works if opioids are in the system. If you give naloxone to someone who hasn’t taken opioids, nothing happens. No side effects. No danger. That’s why it’s safe for anyone to use - family members, friends, even strangers.
Studies show naloxone reverses overdoses successfully in 85% to 95% of cases when given quickly. In communities where it’s widely available, overdose deaths drop by up to 14%. That’s not a small number. That’s thousands of lives saved every year.
Recognizing an Opioid Overdose - Don’t Wait
Most people think an overdose looks like someone passed out on the floor. But it’s often quieter than that. Look for these signs:
- Unresponsive to loud noises or shaking
- Slow, shallow, or stopped breathing
- Lips or fingernails turning blue or gray
- Pinpoint pupils (very small dark circles in the center of the eyes)
- Gurgling or snoring sounds - like they’re drowning but still breathing
Don’t wait for all these signs. If someone is unresponsive and you suspect opioids were involved, act. Time matters. A 2022 study found survival rates drop from 95% if naloxone is given within 2 minutes, to just 65% if delayed beyond 5 minutes.
Many people mistake overdoses for drunkenness or seizures. But alcohol and stimulants don’t respond to naloxone. If you’re unsure, give it anyway. It won’t hurt. And if they’re overdosing, it could save their life.
Naloxone Forms: Spray vs. Injection
There are two main ways to give naloxone: nasal spray and injection.
Nasal spray (like Narcan) is the most common today. It’s easy. No needles. Just spray one dose into one nostril. The FDA-approved version delivers more naloxone into the bloodstream than homemade versions. Since 2023, it’s been available over the counter at pharmacies, grocery stores, and even some gas stations.
Intramuscular injection (using a syringe) is still used by EMS and hospitals. It works just as well but requires more training. For most people, the nasal spray is the better choice.
But here’s the catch: fentanyl is so strong that one dose of naloxone often isn’t enough. The CDC reports that 40% of fentanyl overdoses require two or more doses. That’s why it’s smart to carry two naloxone kits. Always call 911 after giving naloxone - even if the person wakes up. The effects of naloxone wear off in 30 to 90 minutes, but opioids like fentanyl can stay in the body for hours. They can slip back into unconsciousness.
What Happens After Naloxone?
People who’ve been using opioids regularly will go into sudden withdrawal after naloxone. That’s not an allergic reaction - it’s the body reacting to the sudden absence of opioids. Symptoms include:
- Agitation or anger
- Nausea and vomiting
- Sweating
- Shaking
- Fast heartbeat
This can be scary - for the person and for the person giving naloxone. But it’s not life-threatening. The risk of death from the overdose is far greater than the risk from withdrawal. Keep them calm. Keep them breathing. Put them in the recovery position (on their side) to prevent choking if they vomit.
Some people panic and run away after naloxone because withdrawal feels so bad. That’s why staying with them until help arrives is critical. Don’t let them leave. Call 911. Stay. Even if they’re mad at you.

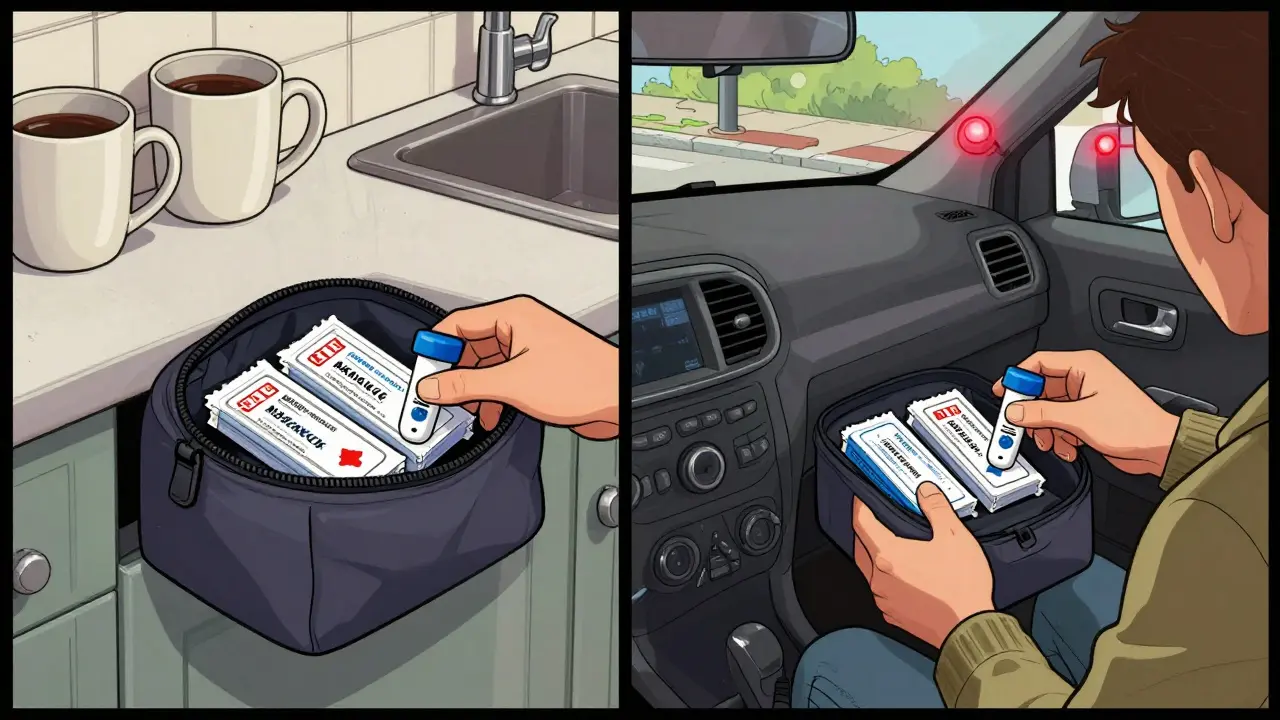
Safe Storage: Keep Naloxone Ready, Not Hidden
Naloxone doesn’t work if it’s locked in a drawer or buried in a first aid kit nobody remembers. Store it where it can be found fast.
- Keep it at room temperature - no need to refrigerate.
- Avoid extreme heat. Don’t leave it in a hot car or near a radiator.
- Check the expiration date every 6 months. Most kits last 2 to 3 years.
- Keep it in a visible spot - on the kitchen counter, next to the medicine cabinet, in your purse or car.
- If you live with someone who uses opioids, make sure they know where it is and how to use it.
Some people worry that having naloxone around encourages drug use. But research shows the opposite. Communities with free naloxone programs see more people seek treatment, not more overdoses. Naloxone isn’t permission to use - it’s a safety net.
Where to Get Naloxone - And How Much It Costs
You can buy naloxone nasal spray at any pharmacy in the U.S. without a prescription. Brands like Narcan and Kloxxado are sold over the counter. Prices vary: $130 to $150 if you pay cash. But many programs give it away for free.
Check with your local health department, needle exchange programs, or community centers. In many places, you can get a free kit with training. The CDC’s website lists free distribution sites by state. Some pharmacies offer discounts if you use a coupon or health savings account.
Don’t let cost stop you. One kit can save a life. And if you’re worried about someone, having two kits on hand is a smart move.
Training Is Simple - And Free
You don’t need to be a nurse to use naloxone. Most training sessions take 15 to 20 minutes. They cover:
- Recognizing an overdose
- How to use the nasal spray
- What to do after giving naloxone
- When to call 911
State health departments, libraries, and nonprofits offer free sessions. The NIDA website has a free online training module that’s been used over a million times. YouTube videos from trusted sources like the CDC or SAMHSA are also reliable.
Practice makes confidence. If you’ve never used it before, practice on an empty kit (many programs give you training versions with no medicine). You’ll be surprised how simple it is.
What Naloxone Can’t Do
Naloxone only works on opioids. It won’t reverse overdoses from:
- Benzodiazepines (like Xanax or Valium)
- Stimulants (like cocaine or meth)
- Alcohol
- Antidepressants or other drugs
If someone overdoses on a mix of drugs - and many do - naloxone can still help if opioids are part of the mix. But it’s not a cure-all. Always call 911. Emergency responders can treat other causes of overdose too.
What’s Next for Naloxone?
Science is improving naloxone. In 2024, the FDA approved a higher-dose nasal spray (8 mg) specifically for fentanyl overdoses. New formulations are in trials that could last longer than current versions - giving people more time before needing a second dose.
The Biden administration is spending $200 million to get naloxone into more homes, schools, and public spaces. The goal? Distribute 2 million kits per year.
But experts agree: naloxone alone isn’t enough. It’s a tool - not a solution. Real change needs better access to addiction treatment, mental health care, and harm reduction services. But until those systems catch up, naloxone is the best tool we have to stop people from dying right now.
Final Thought: Be the Person Who Acts
Most opioid overdoses happen at home, with family or friends nearby. Someone you know - a neighbor, a cousin, a coworker - could be at risk. You don’t need to be a hero. You just need to be ready.
Keep a kit. Know the signs. Practice the steps. Call 911. Stay with them. You don’t have to understand addiction to save a life. You just have to care enough to act.
Can naloxone be used on children or elderly people?
Yes. Naloxone is safe for all ages, including children and older adults. The dose doesn’t change based on age or weight. It only works if opioids are present, so there’s no risk of harm if given to someone who hasn’t taken opioids. Emergency responders routinely use it on infants born to mothers using opioids.
Is naloxone legal to carry in public?
Yes. All 50 states have laws allowing anyone to possess and administer naloxone without a prescription. Many states also offer legal protection for people who give naloxone in good faith during an emergency. You can carry it in your bag, car, or pocket without fear of legal trouble.
How long does naloxone last, and when do you need a second dose?
Naloxone works for 30 to 90 minutes. But many opioids, especially fentanyl, last much longer. If the person stops breathing again after 30 minutes, give a second dose. Most overdoses from synthetic opioids require two or three doses. Always call 911 - even if they wake up - because they can relapse into overdose after naloxone wears off.
Can you overdose on naloxone?
No. Naloxone has no effect on people who haven’t taken opioids. Even giving multiple doses won’t cause an overdose. The only risks are withdrawal symptoms in opioid-dependent individuals - which are uncomfortable but not life-threatening. The benefit of saving a life far outweighs any temporary discomfort.
Does naloxone work on fentanyl?
Yes - but it often takes more than one dose. Fentanyl is 50 to 100 times stronger than morphine. Many people need two or three doses of naloxone to reverse a fentanyl overdose. The newer 8 mg nasal spray (Kloxxado) was designed specifically for this. Always use two kits if you’re in an area where fentanyl is common.
Where can I get free naloxone?
Many local health departments, community clinics, needle exchange programs, and pharmacies offer free naloxone kits. Visit the CDC’s website or call the Poison Help hotline at 1-800-222-1222 to find free distribution sites near you. Some pharmacies also give away kits through nonprofit partnerships.
Next Steps: What to Do Today
If you’ve never thought about naloxone before, start here:
- Visit your local pharmacy and ask for Narcan or Kloxxado nasal spray.
- Ask for a free training session - most pharmacists will give you a quick demo.
- Buy two kits. Keep one at home, one in your car or bag.
- Teach one person you care about how to use it.
- Check the expiration date every six months and replace it if needed.
You don’t need to be a medical professional. You don’t need to be brave. You just need to be prepared. Someone’s life might depend on it - and it could be someone you love.








14 Comments
I keep a Narcan kit in my glovebox. Never thought I'd need it until my cousin OD'd last year. We got to him in 90 seconds. He's alive today because of it. Simple as that.
If you're reading this and haven't grabbed a kit yet, stop scrolling. Go to the pharmacy right now. Buy two. Give one to your neighbor. You don't need to be a hero-you just need to be the person who didn't look away. Lives are waiting on that decision.
I had no idea naloxone was available over the counter until last month. Got mine at Walmart next to the cough syrup. The pharmacist showed me how to use it while I waited in line. No judgment. Just help. That’s the kind of system we need more of.
They’re pushing this because Big Pharma wants us to think they care 😒💉 #NaloxoneIsAClimateChangeScam
Funny how we’ll hand out lifesaving tools like candy but won’t fund rehab centers. We’d rather be the people who revive bodies than fix the system that breaks them. We’re not saving lives-we’re just delaying the funeral.
I’ve given naloxone twice. First time, the guy woke up screaming at me like I stole his wallet. Second time, he hugged me and cried. Doesn’t matter what they say afterward. You did the right thing. Keep doing it.
In my town, the library gives out free kits and hosts training every Thursday. No ID needed. Just show up. I took my mom. She’s 72. She’s now the most prepared person in our neighborhood. Best thing I ever did.
Let’s be honest-this is just another performative gesture. We slap naloxone on the shelves like it’s a Band-Aid for a gunshot wound. Meanwhile, the opioid crisis is fueled by corporate greed, broken mental health infrastructure, and a culture that treats addiction like a moral failing. You can’t spray your way out of systemic collapse.
The CDC’s data on fentanyl requiring multiple doses is solid, but I’ve seen too many first responders get burned because laypeople don’t understand pharmacokinetics. The 30–90 minute window isn’t a guarantee-it’s a countdown. If you’re going to carry it, know the half-life. Otherwise, you’re just waving a placebo.
I used to work in ER. Saw the same faces come in over and over. One guy got revived six times. Sixth time, he looked at me and said, 'You know, I’m not gonna die today. But I’m not gonna live either.' That’s the real tragedy. Naloxone doesn’t fix the loneliness. Doesn’t fix the trauma. Doesn’t fix the fact that nobody showed up for him when he needed them most. We’re just buying time with a spray bottle.
I’m not saying naloxone is bad. But let’s not pretend this is progress. We’ve turned a public health emergency into a spectator sport where we cheer for the person who saved someone while ignoring the person who needed help five years ago. We’re good at CPR. We’re terrible at prevention.
In India we dont have this problem because we dont have fentanyl flooding our streets like america does. Why are you importing your problems to the rest of the world
Naloxone? That's a capitalist trick to keep addicts alive so they keep buying drugs. In Nigeria we just let them die and save the money for real problems like electricity and food
I brought my first naloxone kit to my daughter’s school. She’s 16. She said, 'Mom, why are you giving this to them?' I told her, 'Because if you ever have to use it on someone you love, you’ll wish you’d done it sooner.' She now carries one in her backpack. I’m proud of her.