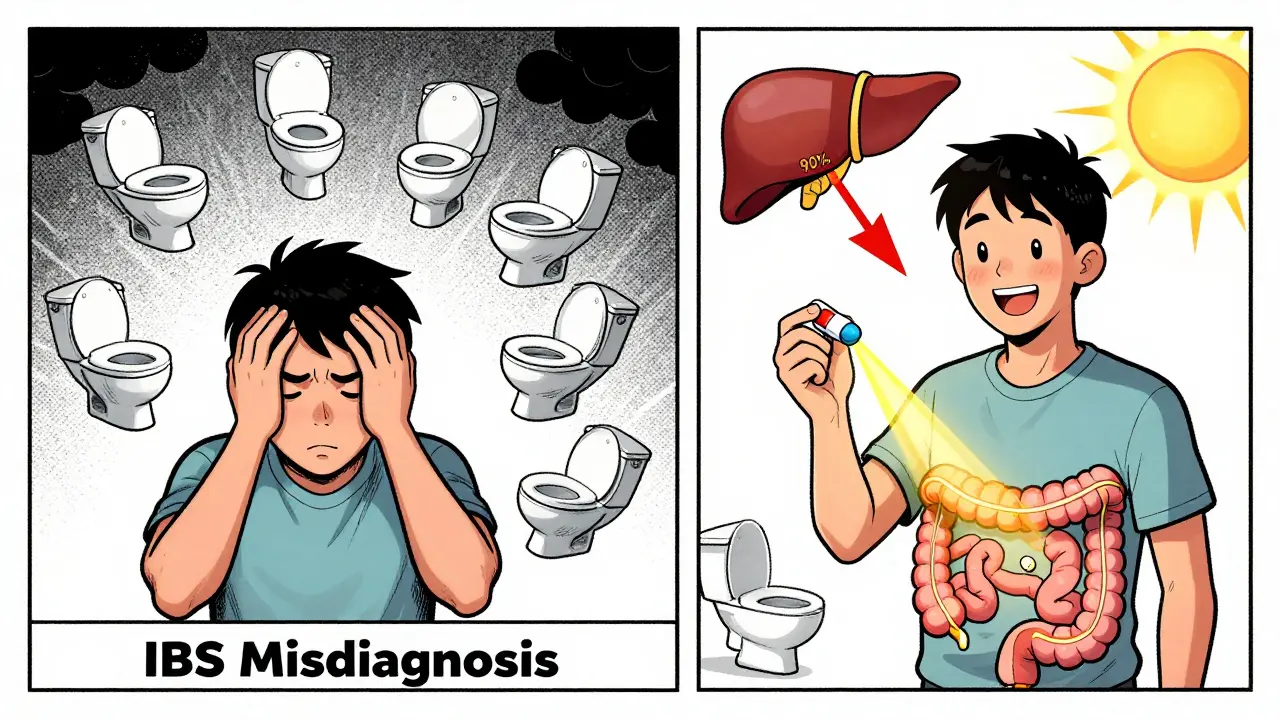
What Is Microscopic Colitis?
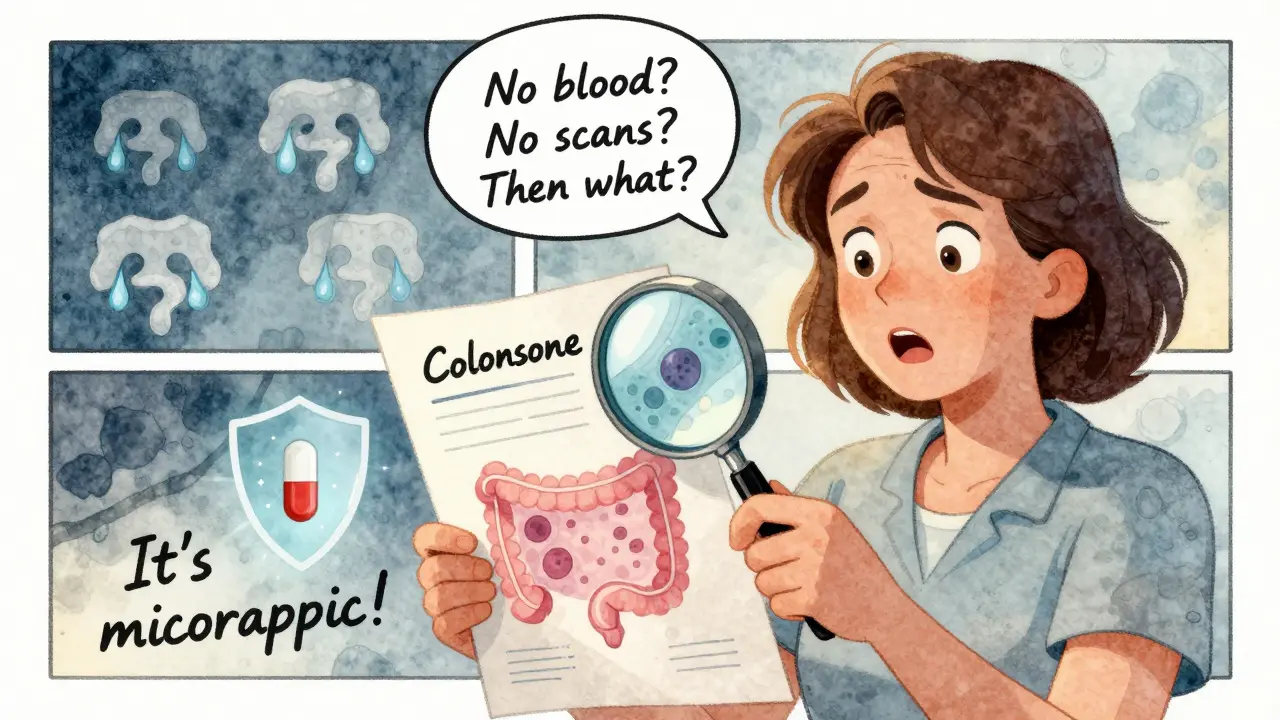
Microscopic colitis is a hidden cause of long-lasting, watery diarrhea-no blood, no obvious signs on colonoscopy, but serious enough to wreck your daily life. You might feel fine one day and then spend hours in the bathroom the next. It’s not Crohn’s or ulcerative colitis. It doesn’t show up on scans. The inflammation? Only visible under a microscope. That’s why it’s called microscopic colitis.
There are two types: collagenous colitis and lymphocytic colitis. Both cause the same symptoms, but the damage looks different under the lens. In collagenous colitis, a thick band of collagen forms under the colon lining-like a plastic sheet blocking water absorption. In lymphocytic colitis, too many white blood cells pile up inside the lining. Either way, your colon can’t hold onto water. Result? Five to ten watery bowel movements a day, often at night. Some people lose weight. Others deal with incontinence or cramps.
It mostly hits people over 50, and women are twice as likely to get it as men. Many wait over a year before getting diagnosed because doctors often mistake it for irritable bowel syndrome. The only way to know for sure? A colon biopsy. If your colon looks normal during a scope but you’re still having chronic diarrhea, ask for biopsies. Don’t assume it’s IBS.
Why Budesonide Is the First-Line Treatment
When you’re stuck in a cycle of daily diarrhea, you need something that works fast-and safely. That’s where budesonide comes in. It’s not your grandpa’s steroid. Unlike prednisone, which floods your whole body with hormones and causes weight gain, mood swings, or bone loss, budesonide is designed to work locally. About 90% of it gets broken down by your liver before it ever reaches your bloodstream. That means you get the anti-inflammatory punch in your colon-with far fewer side effects.
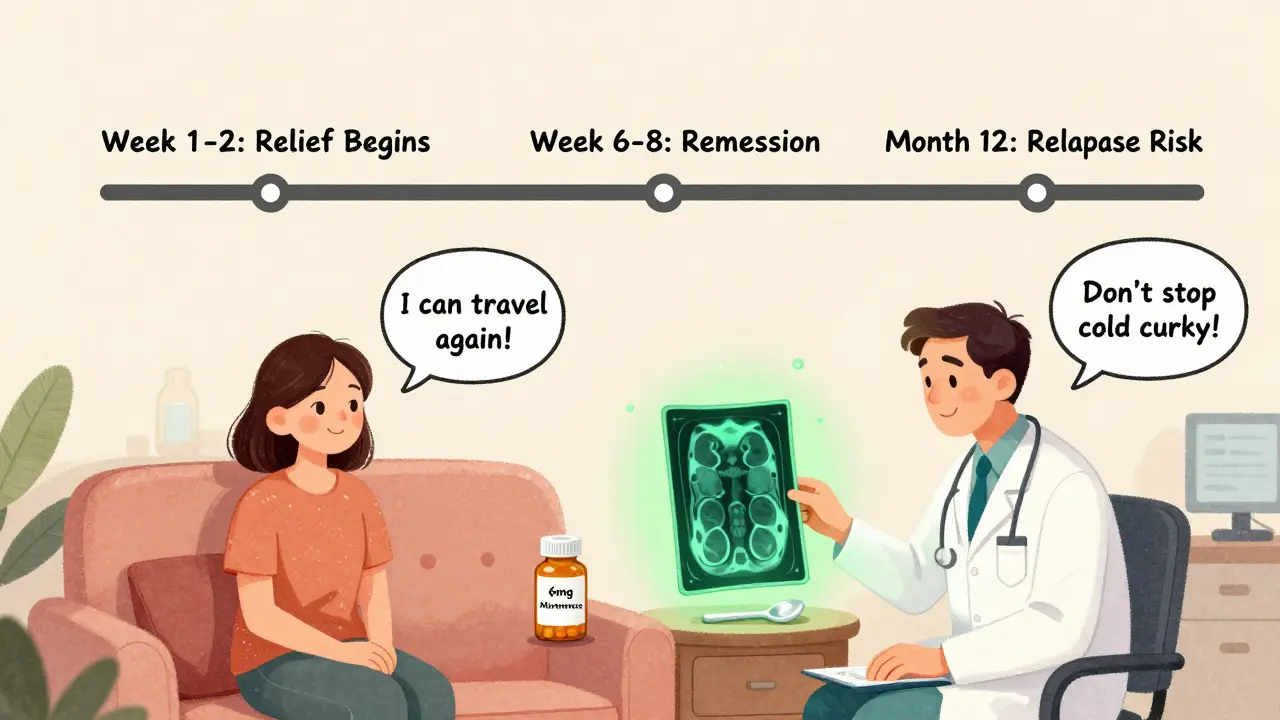
Studies show that 75 to 85% of people with microscopic colitis go into remission after taking 9 mg of budesonide daily for 6 to 8 weeks. In one major trial, 84% of collagenous colitis patients saw their diarrhea vanish within two months, compared to just 38% on placebo. Most people notice improvement within 10 days. One Reddit user wrote: “Went from 10 bathroom trips a day to 2 in under two weeks.” That’s not an outlier. That’s the norm.
Guidelines from Europe and North America agree: budesonide is the go-to first treatment. It’s recommended by the European Microscopic Colitis Group and the Crohn’s & Colitis Foundation. Gastroenterologists in Scandinavia, where the disease is most common, prescribe it in over 90% of cases. The FDA approved generic versions in 2018, cutting the cost by more than half. You don’t need to pay $1,200 for the brand name Entocort EC anymore.
How Budesonide Compares to Other Options
What if budesonide doesn’t work-or you can’t afford it? Other options exist, but none match its success rate.
- Bismuth subsalicylate (Pepto-Bismol): Works for about 26% of people. Cheap, but you’ll need to take it daily for months. Tastes awful. Can turn your stool black.
- Mesalamine: Used for ulcerative colitis, but only helps 40-50% of microscopic colitis patients. Often used when budesonide isn’t available.
- Cholestyramine: Good if bile acid malabsorption is part of the problem. Works for 60-70% in those cases. Often combined with budesonide for better results.
- Prednisone: Works just as well as budesonide-but 45% of users get serious side effects like high blood sugar, insomnia, or muscle loss. Not worth the risk.
- Anti-TNF drugs (like infliximab): Used for severe Crohn’s. They help only 20-30% of microscopic colitis patients and cost $2,500-$3,000 per infusion. Reserved for cases that don’t respond to anything else.
Budesonide isn’t perfect, but it’s the best balance of effectiveness, speed, and safety we have right now.
What Happens After the 8 Weeks?
Here’s the catch: budesonide doesn’t cure microscopic colitis. It controls it. About half of people relapse within a year after stopping the drug. That’s why many need maintenance therapy.
Doctors often taper the dose slowly-reduce by 3 mg every 2 to 4 weeks. Some patients stay on 6 mg daily for months or even years. One patient on PatientsLikeMe said: “It worked great for 6 weeks. Then symptoms came back. Now I’m on maintenance for two years.”
Long-term use is generally safe because of the low systemic absorption. But it’s not risk-free. In older adults, even small amounts of steroids can affect bone density or blood sugar. That’s why your doctor should check your HbA1c, blood pressure, and bone density before starting-and every year after.
If you’re on maintenance, consider adding a bile acid binder like cholestyramine. Many patients find that combining treatments reduces the dose they need and lowers relapse risk. “Budesonide plus cholestyramine fixed me after 3 years of suffering,” wrote one Reddit user.
Real People, Real Experiences
Online forums are full of stories. Of the 247 patients tracked on PatientsLikeMe, 68% said budesonide gave them their life back. But 32% had problems.
- Positive: “I stopped hiding from social events. I could travel again.”
- Negative: “I got acne, couldn’t sleep, and felt anxious. I thought it was the diarrhea-I didn’t know it was the drug.”
- Cost shock: “I had insurance. Without it, I couldn’t afford this.”
- Relapse frustration: “I tapered too fast. Within a week, I was back to square one.”
Many don’t realize how common relapse is. They stop the medication when they feel better-not realizing they need to finish the full course and possibly continue at a lower dose. Your doctor should talk to you about this before you even start.
What You Should Ask Your Doctor
If you’ve been diagnosed with microscopic colitis, here’s what to ask:
- “Is this collagenous or lymphocytic colitis? Does it matter for treatment?”
- “Do I need a baseline bone density scan or blood sugar test before starting budesonide?”
- “What’s the plan if I relapse after stopping?”
- “Can I combine budesonide with cholestyramine or another agent to reduce long-term use?”
- “Are there cheaper generic versions available?”
Don’t let the word “steroid” scare you. Budesonide isn’t the same as the steroids bodybuilders use. It’s targeted. It’s studied. It’s the standard for a reason.
What’s Next for Treatment?
The future is looking promising. In 2023, the FDA gave fast-track status to vedolizumab-a biologic drug that targets gut-specific inflammation. Early trials show 65% remission in patients who didn’t respond to budesonide. It’s not approved yet, but it could be a game-changer for those stuck on long-term steroids.
Researchers are also looking at genetics. Early data from the COLMICS trial suggests people with HLA-DQ2 or HLA-DQ8 genes respond better to budesonide. In the next five years, we may see blood tests that predict who will benefit most from which drug.
For now, budesonide remains the gold standard. It’s effective, safe, and backed by decades of research. If you’re struggling with unexplained chronic diarrhea, don’t give up. Get the biopsy. Ask for budesonide. You might get your life back faster than you think.
Common Questions About Microscopic Colitis and Budesonide
Is microscopic colitis the same as IBS?
No. IBS is a functional disorder-your gut looks normal and there’s no inflammation. Microscopic colitis is an inflammatory disease. The symptoms overlap-watery diarrhea, cramping-but only a colon biopsy can confirm microscopic colitis. Many people are misdiagnosed with IBS for years before getting the right test.
Can I take budesonide if I have liver disease?
Not if you have severe liver disease (Child-Pugh Class C). Budesonide is broken down by the liver. If your liver can’t process it, the drug builds up in your blood, increasing the risk of steroid side effects. Mild or moderate liver disease may be okay with close monitoring, but your doctor will need to adjust the dose or choose another option.
How long does it take for budesonide to work?
Most people notice improvement within 7 to 14 days. By week 4, 70-80% of patients are in remission. Don’t stop taking it just because you feel better. The full 6-8 week course is needed to fully reduce inflammation and lower the chance of early relapse.
Does budesonide cause weight gain?
Unlike prednisone, budesonide rarely causes significant weight gain. Because it’s mostly metabolized by the liver before entering the bloodstream, it doesn’t trigger the same metabolic changes. Some people report mild bloating or increased appetite, but serious weight gain is uncommon. If you notice rapid weight gain, talk to your doctor-it could be a sign of fluid retention or another issue.
Can I stop budesonide cold turkey?
No. Stopping suddenly can trigger a flare-up or even adrenal suppression, especially if you’ve been on it for more than a few weeks. Always taper under medical supervision. A typical taper is reducing by 3 mg every 2-4 weeks. Your doctor may recommend staying on a low dose (3-6 mg) for months if you’re prone to relapse.
Are there natural remedies that work for microscopic colitis?
No proven natural remedies can replace budesonide for inducing remission. Some people find relief from avoiding NSAIDs, caffeine, or dairy, but these don’t treat the inflammation. Bismuth subsalicylate (Pepto-Bismol) is available over the counter and helps a minority of patients, but it’s not as effective as prescription budesonide. Don’t delay proper treatment in favor of unproven supplements.
What to Do Next
If you’ve had chronic diarrhea for more than 4 weeks and tests haven’t found a cause, ask your doctor for a colon biopsy. Don’t settle for an IBS diagnosis without ruling out microscopic colitis. If you’ve been diagnosed, start budesonide as directed. Track your symptoms. Talk to your doctor about tapering and maintenance. And remember-you’re not alone. Thousands have walked this path and found relief. The key is getting the right diagnosis and sticking with the treatment plan.











15 Comments
I've been dealing with this for years in Delhi, and honestly, budesonide was the only thing that gave me back my life. I used to avoid family gatherings because I didn't know when I'd have to run to the bathroom. Now I travel to Goa with my kids without panic. The cost was brutal at first, but the generic? Game changer. Don't let the word 'steroid' scare you-it's not prednisone. This drug is like a sniper, not a bomb.
If you're still using Pepto-Bismol for microscopic colitis you're wasting your time and money. This isn't a digestive hiccup it's an inflammatory disease. Budesonide is the gold standard because the science backs it. Stop listening to random Reddit users who say 'natural remedies work'-if your colon is inflamed you need targeted anti-inflammatories not herbal tea. End of story.
I was diagnosed last year and I'll be honest I cried when I found out it wasn't IBS. All those years thinking I was just 'anxious' or 'eating wrong'-turns out my colon was literally screaming. Budesonide worked like magic. I started feeling better in 8 days. The only thing I wish someone had told me? Don't stop it just because you feel fine. I did that once and ended up back in the bathroom for weeks. Taper slow. Your body will thank you.
This post made me feel so seen. I spent 18 months being told it was stress or IBS. My doctor didn't even mention biopsies. I finally pushed back and demanded them. When the results came back I felt like I'd been given a map after wandering in the dark. Budesonide didn't fix everything-still get occasional cramps-but I can sleep through the night now. That alone is worth every pill.
The real tragedy here isn't the disease-it's the medical industrial complex's failure to acknowledge that microscopic colitis is a silent pandemic of the aging female body. We're dismissed as 'hysterical' or 'menopausal' while our colons slowly unravel. Budesonide is a bandage on a bullet wound. The real question is why aren't we researching the root causes? Why is it still so underfunded? Why do we treat symptoms instead of asking why collagen bands form? The answer is gendered neglect disguised as science.
They're lying about budesonide. It's not safe. The FDA approved generics because Big Pharma wanted to kill the brand name and make more money. They don't want you to know that steroids cause adrenal shutdown and that's why they tell you to taper slowly. I know someone who got diabetes from it. And why is it only approved for 8 weeks? Because they know it's not a cure. This is all a scam. The real cause? Glyphosate in the water. Look it up.
The notion that budesonide is 'safe' because it's metabolized by the liver is a dangerous oversimplification. Systemic absorption still occurs, particularly in elderly patients with reduced hepatic clearance. The claim that side effects are 'rare' is statistically misleading when population-based studies show increased incidence of osteoporosis and hyperglycemia in long-term users. Furthermore, the FDA's approval of generics does not equate to bioequivalence in all formulations-many patients report variable efficacy between manufacturers.
I'm 54 and was diagnosed last year. I didn't know anything about this. My doctor just said 'take this pill.' I wish I'd known sooner about combining it with cholestyramine. I started on 9mg and felt better fast, but when I tapered, I relapsed hard. My GI doc finally suggested adding the binder and now I'm on 3mg budesonide + cholestyramine daily. It's not perfect but I can go out to dinner without planning my life around the nearest bathroom. Thank you for writing this. I needed to hear I'm not alone.
This whole thing is a liberal hoax. Why is this disease so common in the US and Europe but not in China or India? Because they don't have the same processed food and GMOs. They don't need budesonide. They eat real food. You don't need a steroid to fix your gut if you stop eating chemicals. This is what happens when you let Big Pharma control medicine. Go back to eating rice and lentils. Problem solved.
I would like to extend my sincere appreciation for the comprehensive and meticulously researched exposition presented herein. The delineation of pathophysiological mechanisms underlying microscopic colitis, coupled with the evidence-based analysis of therapeutic modalities, represents a paradigmatic exemplar of clinical communication. The pharmacokinetic profile of budesonide, particularly its first-pass hepatic metabolism, is not only scientifically accurate but also profoundly illuminating for the lay reader. One might posit that the integration of genetic biomarkers such as HLA-DQ2/8 into future diagnostic protocols could represent a quantum leap toward personalized gastroenterological care.
I'm not saying budesonide doesn't work. I'm saying it's overprescribed. I know three people who were put on it and then got fungal infections, anxiety, or worse. One guy got cataracts. You're telling me we can't find a safer alternative? Why are we using a steroid at all when we have mesalamine? Maybe the real issue is that doctors are lazy and want a quick fix. This isn't science-it's protocol. And the cost? Still too high for people without insurance.
Budesonide is just a Band-Aid. The real problem is the microbiome collapse caused by decades of antibiotics, processed foods, and glyphosate exposure. You think your colon is inflamed because of genetics? No. It's because your gut flora is dead. Probiotics, fermented foods, and fasting can reverse this. I did it. I stopped budesonide after 4 weeks and started eating sauerkraut and bone broth. My symptoms vanished in 3 weeks. The medical system doesn't want you to know this because there's no profit in cabbage.
As a retired gastroenterologist who worked in a university hospital for 35 years, I can confirm that budesonide remains the most effective and safest first-line agent for microscopic colitis. The data is robust, the guidelines are clear, and the real-world outcomes are consistently favorable. I have seen patients in their 80s tolerate low-dose maintenance therapy without significant complications. What matters most is not the fear of steroids, but the fear of living with uncontrolled diarrhea. This post is accurate, balanced, and urgently needed.
Budesonide? That's just the latest pharmaceutical fad. Remember when everyone was on PPIs for everything? Now it's budesonide. Next it'll be some new biologic. The truth? Most people with 'microscopic colitis' just need to stop drinking coffee and eat more fiber. I've been in this field 20 years. The diagnosis is overused. The treatment is overhyped. The real issue? Doctors don't know how to listen. They see diarrhea, they order a biopsy, they hand you a script. No one asks about your stress, your sleep, your diet. This isn't medicine. It's transactional.
Just wanted to say thanks for this. I was terrified of steroids too. Thought I’d gain 30 pounds and turn into a zombie. But I followed the plan-9mg for 8 weeks, then dropped to 6mg for 3 months, now I’m at 3mg. I still take it. I don’t care. I can hike again. I can watch my granddaughter’s soccer games without running to the bathroom every 10 minutes. It’s not magic. But it’s the best tool we’ve got. And honestly? I’d rather take a tiny steroid pill than live like that again.