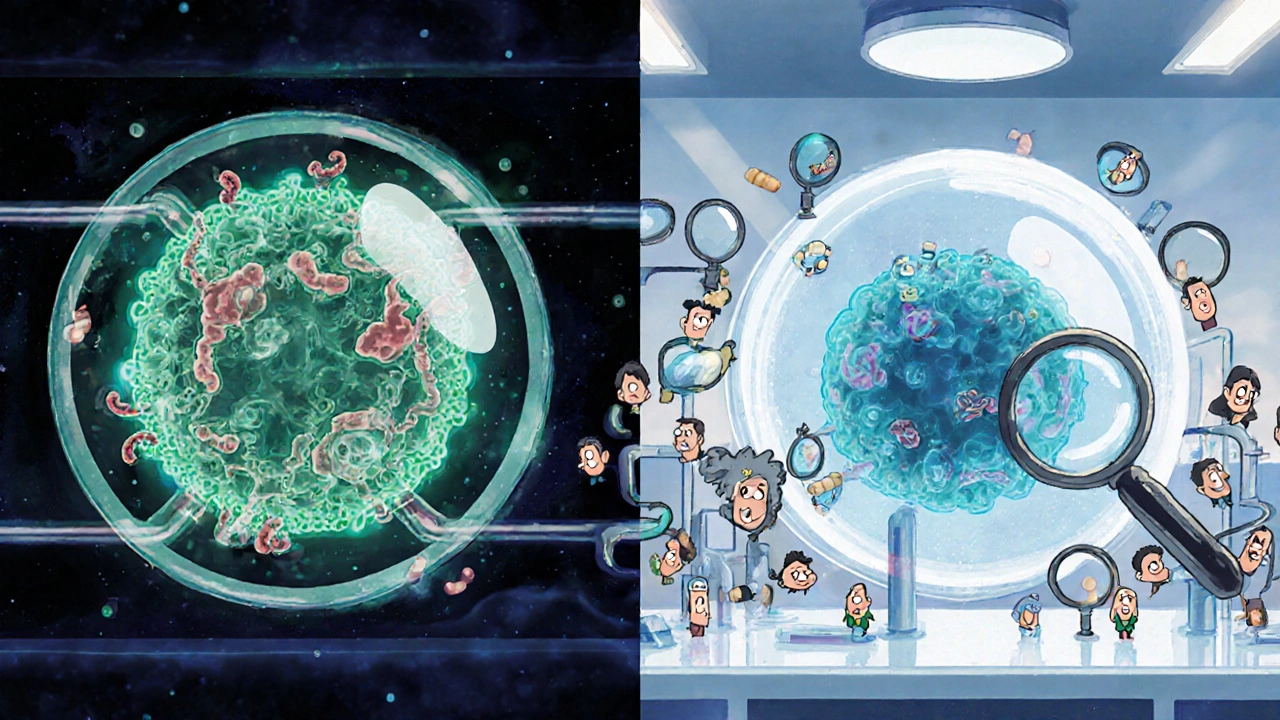
When you hear the word biosimilars, you might think they’re just generic versions of expensive biologic drugs. But they’re not. Generics are simple copies of small-molecule pills-like ibuprofen or metformin. Biosimilars are complex, living drugs made from living cells. They’re designed to be nearly identical to a reference biologic, like Humira, Enbrel, or Avastin. The big question patients and doctors ask: Do they work as well? The answer, backed by years of real-world data and rigorous science, is yes.
They’re not generics. They’re something else entirely.
Generics are chemically identical to their brand-name counterparts. You can make them in a lab with the same molecules, same structure, same everything. Biosimilars? Not even close. They’re made from living organisms-usually cells grown in bioreactors. Even tiny changes in temperature, nutrients, or processing can alter their structure. That’s why regulators don’t call them "copies." They call them "highly similar."
The FDA and EMA require biosimilars to go through more than 200 analytical tests before even touching a human. These tests look at protein shape, sugar attachments, purity, stability, and how the drug behaves in the body. Only after proving they’re nearly identical at the molecular level do they move to clinical trials. And even then, they’re tested in real patients-not just in test tubes.
Do they actually work the same in real patients?
Let’s cut through the noise. Over 500,000 patients worldwide have been tracked in studies comparing biosimilars to their reference biologics. The results? No meaningful difference in how well they work.
In rheumatoid arthritis, a study of 3,450 patients across 12 European hospitals found that the biosimilar ABP501 had the same drug survival rate as the original adalimumab-82.3% versus 81.7%. That’s not a fluke. In inflammatory bowel disease, a Canadian trial of 1,200 patients showed no difference in disease control, flare-ups, or side effects after two years of using the infliximab biosimilar CT-P13 versus the original.
In cancer treatment, the NOR-SWITCH trial gave 480 patients either the original rituximab or its biosimilar. After one year, the response rates were nearly identical: 72.9% versus 69.3%. The difference? Statistically meaningless. The same pattern held true for bevacizumab in lung and colon cancer, and trastuzumab in breast cancer. Across six different cancers, the overall response rates were all within 1% of the original drug.
And it’s not just clinical trials. Real-world data from the UK’s NHS tracked 12,000 patients switched from original rituximab to its biosimilar. No spike in side effects. No drop in effectiveness. On PatientsLikeMe, 87% of users on the adalimumab biosimilar Amjevita said their symptom control was the same as when they were on Humira. Only 2% reported worse symptoms-and even those cases were often linked to other factors, like stress or infections, not the drug itself.
What about safety? Are they riskier?
One of the biggest fears is immunogenicity-will your body react to the biosimilar differently than the original? Will it cause more antibodies, more flares, more side effects?
The science says no. In fact, 84% of biosimilar trials were double-blinded, meaning neither patients nor doctors knew which drug was being given. That’s more rigorous than many original biologic trials, which often weren’t blinded at all. The result? No increased immune response. No higher rate of serious infections, allergic reactions, or autoimmune events.
Some early concerns focused on the manufacturing process. But biosimilars aren’t made in one batch-they’re made across dozens, sometimes hundreds, of batches. Regulators test each one. The FDA requires that biosimilars show no clinically meaningful differences in safety across all those batches. That’s not just a formality. It’s a requirement.
Even long-term data, now reaching five to seven years for some biosimilars, shows no red flags. A 2023 review of over 300 real-world studies concluded that biosimilars are as safe as the originals. That’s not opinion. That’s consensus from 47 experts across 15 countries.
Why do some doctors still hesitate?
If the data is this strong, why do 38% of U.S. physicians still express doubt? The answer isn’t science. It’s perception.
Many doctors were trained to think of generics as "cheap copies." They don’t realize biosimilars are held to a completely different standard. Some worry about switching patients mid-treatment. Others fear lawsuits if something goes wrong-even though the evidence shows no increased risk.
There’s also misinformation. A 2021 survey found many doctors believed biosimilars were "less tested" or "only approved because they’re cheaper." That’s false. The approval process for biosimilars is longer, more complex, and more expensive than for generics. It takes 8-10 years and hundreds of millions of dollars to bring one to market.
But awareness is changing. A 2023 survey of 1,500 rheumatologists found 78% reported identical outcomes with biosimilars. Only 4% believed the difference was due to the drug itself. The rest saw no change-or even better outcomes.
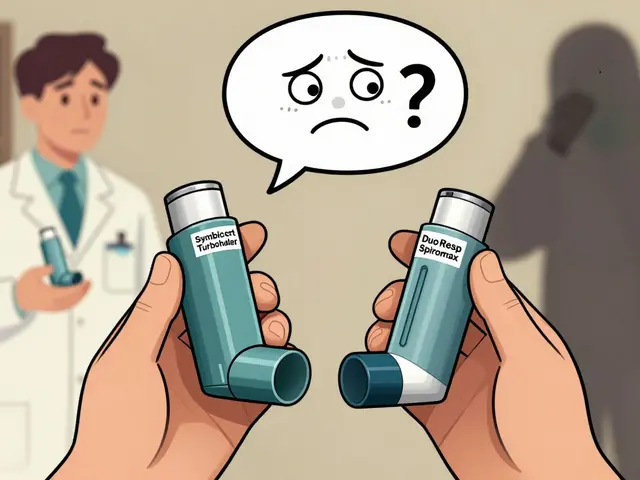
How do you know if a biosimilar is right for you?
If you’re on a biologic and your doctor suggests switching, here’s what to ask:
- Is this biosimilar approved for my exact condition? (Not all are approved for every use.)
- Has it been studied in patients like me?
- Will I need to be monitored after switching?
- Is this a substitution or a switch? (Some states allow pharmacists to substitute without asking the doctor-others don’t.)
Most switches happen smoothly. A 2023 study across 15 U.S. health systems showed that with proper patient education, refusal rates dropped from 22% to just 5%. Simple materials-like a one-page handout explaining how biosimilars are made and tested-made all the difference.
Some patients report a placebo effect-feeling like they’re on a "cheaper" drug, so they worry it won’t work. That’s normal. But when you track symptoms, lab results, and flare-ups, the numbers don’t lie. If you feel the same, your disease activity is stable, and your bloodwork looks good, you’re doing fine.
What’s the real benefit? Cost.
Biosimilars aren’t just safer-they’re cheaper. In the U.S., they’re typically 15-30% less than the original. In Europe, where competition is fiercer, they’re 25-85% cheaper.
That matters. A single dose of Humira can cost over $2,000. With a biosimilar, it’s $1,400. For a patient on lifelong therapy, that’s tens of thousands saved over a decade. Medicare saved $1.3 billion in 2022 just from biosimilar use. The Congressional Budget Office estimates biosimilars will save the U.S. healthcare system $169 billion over the next ten years.
That money doesn’t just go to insurance companies. It goes to patients who couldn’t afford treatment before. It goes to hospitals that can treat more people. It goes to research that might lead to the next breakthrough.
What’s next for biosimilars?
The next frontier? Biosimilar-to-biosimilar switching. If you’ve been on one biosimilar for years, can you switch to another? Early data says yes. A 2023 study in Clinical Rheumatology followed patients who switched between two different adalimumab biosimilars. After 12 months, drug retention rates were nearly identical to those who stayed on one.
Regulators are catching up, too. The FDA is proposing to eliminate some clinical trials if analytical and pharmacokinetic data are strong enough. That could bring more biosimilars to market faster-without sacrificing safety.
And the pipeline is full. Over 120 biosimilars are in development globally. New ones are coming for psoriasis, multiple sclerosis, and even rare blood disorders. The goal isn’t just to cut costs. It’s to make life-changing treatments available to everyone who needs them.
Bottom line: They work. They’re safe. They’re here to stay.
Biosimilars aren’t a gamble. They’re a proven alternative. Decades of data, hundreds of thousands of patients, and rigorous science all point to the same conclusion: they work as well as the original biologics. The safety profile is the same. The effectiveness is the same. The only real difference? The price tag.
If you’re considering a switch-or your doctor suggests one-ask questions. But don’t let fear hold you back. The evidence isn’t just strong. It’s overwhelming.








8 Comments
Biosimilars are kind of like learning a new language after knowing one fluently. You still understand the meaning, the tone, the emotion behind it - just the accent and some word choices are different. The science says they work. The people using them say they work. So why are we still arguing about it like it’s a religious debate?
US spends too much on drugs. Biosimilars save money. End of story.
It is important to recognize that the introduction of biosimilars represents a profound advancement in equitable healthcare access. The rigorous regulatory frameworks established by the FDA and EMA ensure that patients receive therapeutics of comparable safety and efficacy to originator biologics. The data presented in this post is not merely encouraging - it is definitive. Healthcare systems that embrace biosimilars are not compromising quality; they are optimizing sustainability without sacrificing patient outcomes.
Wow, this is so well-researched! I’m so glad someone finally broke this down clearly! Seriously, if you’re on a biologic and your doc suggests switching, don’t panic - check the approval status, ask about real-world data, and remember: it’s not a downgrade, it’s a smart upgrade! Also, please talk to your pharmacist - they’re your ally here! Don’t let fear drive your decisions - facts do!
ok so biosimilars are basically generics but with more steps? lol. i read somewhere that the original drugs are made by scientists in labs with lasers and unicorns or something. and biosimilars are made by some guy in a basement with a blender and a dream. but i guess if the fda says its cool then its cool. i mean i trust the gov right? right?? also i think my cousin’s dog got better on a biosimilar. maybe dogs are the real test subjects.
Let me tell you something - this whole biosimilar thing is a globalist scam. Big Pharma and the WHO are pushing this because they want to control the drug supply. Why do you think the FDA suddenly approved all these drugs after 2020? Coincidence? No. It’s part of the plan to make Americans dependent on cheap foreign-made medicine. India and China are flooding the market with untested versions. And now they want you to switch from Humira to some Indian-made copy? That’s not science - that’s surrender. My uncle got sick after switching. The hospital never told him the drug wasn’t American-made. That’s not transparency - that’s betrayal.
While I appreciate the thoroughness of this analysis, I must raise a concern: the data presented, though statistically significant, does not account for the psychological impact of perceived substitution. The placebo effect, when reversed, becomes the nocebo effect - and this is not trivial. Patients who believe they are receiving an inferior product may experience heightened anxiety, which can manifest as physiological symptoms indistinguishable from disease progression. Furthermore, the long-term immunogenicity data remains incomplete. The five-year studies are promising, but biologics are administered for decades. Where is the 15-year data? Where are the longitudinal studies tracking autoimmune flares across multiple generations? Until then, I remain unconvinced that this is anything other than cost-driven risk transfer.
ok so here’s the real truth nobody wants to say - biosimilars are just big pharma’s way of keeping their monopoly alive. they make the original drug for 10 years, then let some other company make a copy that’s 99.9% the same, but still charge $1400 instead of $100. why? because they own the patents on the manufacturing process. so now you’ve got two companies charging you $1400 instead of one charging $2000. it’s not saving you money - it’s just splitting the pie. and the worst part? they’re using your tax dollars to fund the research so they can charge you more later. this isn’t healthcare reform - it’s corporate theater. and don’t get me started on how they’re pushing this in schools now. they’re brainwashing us to think cheaper = better. but cheaper doesn’t mean safer. cheaper means they cut corners. and someone’s gotta pay for it - and it’s gonna be us.